Abstract
Several studies revealed that mental disorders' prevalence increased during the COVID-19 pandemic, particularly in young and female individuals. Such studies represent individuals' subjective perceptions and not the number of mental health cases treated in primary care. Thus, this study aimed to describe the changes in depression, anxiety, and stress disorder diagnoses in General Practitioner (GP) practices during the COVID-19 pandemic. More than three million patients of 757 German GP practices were included in this cross-sectional analysis. Descriptive statistics were used to assess changes in the number of incident depression, anxiety disorders, and reaction to severe stress and adjustment disorders documented by GPs in 2020 compared to the average of the years 2017–2019. There was a tremendous decrease in mental health diagnoses during the first lockdown that was only slightly compensated later. Overall populations and the entire year 2020, there was no change in documented depression (0%) and stress disorders (1%), but anxiety disorders were more often documented (+19%), especially for the elderly population (>80 years; +24%). This population group also received more frequently new depression (+12%) and stress disorder diagnoses (23%). The younger population was diagnosed more frequently at the end of 2020, nine months after the first lockdown. Anxiety disorders but not depression and stress diagnoses were elevated, which is not in line with previously published studies. We speculate that the elderly population was affected most by the pandemic immediately after the first lockdown was announced. The younger population has probably become more and more affected the longer the pandemic lasts.
Keywords: Covid-19, Elderly, Lockdown, Mental health, Healthcare utilization, Recognition
1. Introduction
The COVID-19 diseases, caused by the coronavirus strain Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2), spread rapidly worldwide and infected more than 115 million individuals and caused over two and a half million deaths (as of March 15, 2021) (Huang et al., 2020; P. Wu et al., 2020). After China, Europe became the next epicentre of the virus, first Italy and afterward all other European countries (Lapolla et al., 2020). The number of cases in Germany grew rapidly at the beginning of March 2020 during the first wave. Until now, the total number of cases in Germany stands at more than 2.5 million (March 2021), representing the fifth-highest number in Europe after the UK, France, Spain, and Italy ((RKI, 2020; Medicine, 2020). Across the globe, the COVID-19 pandemic was associated with several restrictions in social life due to the introduced lockdowns and contact bans. These initiated measures aimed to reduce the infection rate and prevent strain on the healthcare systems (Chu et al., 2020). Germany reduced social contacts (contact ban) throughout the country at the beginning of the first pandemic wave between March and June 2020, and again until October during the second wave. The introduced measures should minimize close interaction between individuals and decrease individual mobility as much as possible ((RKI, 2020; Chu et al., 2020; Glass et al., 2006; Wilder-Smith and Freedman, 2020).
The COVID-19 pandemic and its associated measures have been a near-ubiquitous exposure for populations, significantly affecting their social life. The more restrictive the introduced measures are, the higher the perceived changes in life (Benke et al., 2020). Several systematic reviews and meta-analyses estimated the pooled prevalence of symptoms of mental disorders related to the COVID-19 pandemic using subjective measures and psychometric questionnaires (Cenat et al., 2021; Deng et al., 2021; Ren et al., 2020). In these studies, the pooled annual prevalences of depression and anxiety were between 16% and 28% and 15% and 25%, respectively. The prevalence of psychological stress was 13% (Cenat et al., 2021). Even though the authors stated that these results should be interpreted with caution, the findings suggest that mental disorders' prevalence was more than 3-fold higher during COVID-19 than before COVID-19 and remained elevated over time (Ettman et al., 2020; Hetkamp et al., 2020; Lakhan et al., 2020). Furthermore, people already suffering from depressive, anxiety, or stress disorders are likely to experience a detrimental impact on their mental health from the COVID-19 pandemic (Pan et al., 2021). Particularly young and female individuals with lower social and economic resources, and greater exposure to stressors, like job loss or loneliness, reported a greater mental burden (Ettman et al., 2020; Liu et al., 2021). Contrary to this, older adults reported lower stress (Adamson et al., 2020). Therefore, a position paper underlined the priority of collecting high-quality data on the mental health effects of the COVID-19 pandemic across the whole population and vulnerable groups (Holmes et al., 2020).
However, pandemic and policy-related aspects and methodological and respondent-related factors could have a tremendous impact on the generalizability of demonstrated study results (Richter et al., 2021). Survey sampling and design of the survey must be led by their purpose (Pierce et al., 2020). Most studies were based on surveys using different mental health screening instruments to detect populations' changes in depression, anxiety, or stress over time. To understand prevalence in a population, how survey respondents are recruited is crucially important. Individuals with existing mental health illnesses are likely to participate online, which could bias the results (Pierce et al., 2020). Such surveys would not represent the primary care situation demonstrated by practitioners' claim data and mental health diagnoses made. During the initial lockdowns, physician consultations and hospital admissions decreased significantly, and incident diagnoses were documented less frequently, raising concerns about the maintenance of routine primary care (Mansfield et al., 2021; Michalowsky et al., 2021).
Therefore, retrospective studies are urgently needed to evaluate the long-term effects of lockdowns on diagnosed depression, anxiety, and stress disorders in physician practices. Until now, there is very limited quantitative evidence based on data from the clinical practice. Thus, this study aimed to describe the changes in documented mental health diagnoses, e.g. depression, anxiety, and stress disorder, in German General Practitioner (GP) practices during the COVID-19 pandemic compared to the average of the years before (2017–2019).
2. Material and methods
2.1. Database
This observational study was based on cross-sectional medical record data from the Disease Analyzer database (IQVIA), which compiles drug prescriptions, diagnoses, and general medical and demographic data obtained directly in anonymous format from computer systems used in the practices of GPs and specialists (Rathmann et al., 2018). Diagnoses, prescriptions, and the quality of reported data are monitored by IQVIA based on an array of criteria. In Germany, the sampling methods used to select physicians' practices have been shown to be appropriate for obtaining a population-representative database of primary and specialized care (Rathmann et al., 2018). The study was carried out following the latest version of the Declaration of Helsinki.
2.2. Study population and variables
The analysis included 3,021,042 patients who visited at least one out of 757 GP practices that routinely send data to the Disease Analyzer database (IQVIA) between 2017 and 2020.
2.2.1. Study outcomes
This study's primary outcomes were the number of incident mental health diagnoses documented by GPs in 2020 compared to the average of the years 2017–2019. The following ICD-10 diagnoses (International Statistical Classification of Diseases and Related Health Problems) were used to demonstrate the incident mental health diagnoses documented in the different physician practices: depression (ICD-10: F32, F33), anxiety disorders (F41), and reaction to severe stress and adjustment disorders (F43). All diagnoses had to be initial diagnoses that had not previously (one year before) been documented by the practitioner to ensure that only first diagnoses of incident diseases were included in this analysis.
2.2.2. Prepandemic and pandemic COVID-19 intervals in Germany considered
The utilization of healthcare services and that of incident diseases recognized were demonstrated separately for each month during the COVID-19 pandemic. According to Holloway et al.(Holloway et al., 2014), the pre-pandemic interval is characterized by an investigation of first COVID-19 cases and the recognition of an increased potential for ongoing transmission, corresponding to February in Germany. The pandemic interval between March and May was characterized by the initiation and acceleration of the pandemic wave. There were less than 200 confirmed COVID-19 cases in Germany at the end of February (pre-pandemic interval), but 50,000, 125,000, and 180,000 cases at the end of March, April, and May (pandemic interval), respectively. The number of confirmed cases per day peaked at the beginning of April (6561 new cases/day). A downward trend was then recorded, with 178 confirmed cases per day at the end of May.
2.3. Statistical analyses
We used descriptive statistics to map mental health diagnoses during the COVID-19 pandemic in 2020 (April to December) in Germany. To assess the changes in recognition of incident mental health diseases, we compared the results for 2020 with the average incident mental health diagnosis for the corresponding year before (April to December 2017, 2018, and 2019) and calculated the percentage change between the period of 2017–2019 and 2020. To demonstrate practitioners' perceived changes, we also used the mean number of documented incident mental health diagnoses per practice. Differences between the periods were assessed using Wilcoxon tests. To estimate the association between age, sex, and interaction effect of age and sex, and the relative difference between the number of new anxiety patients in 2020 versus 2019, multivariable linear regression model was performed. One-sample Kolmogorov-Smirnov test was used to check whether the data (patient number per practice) are distributed normally or not. As there was an evidence that the data were not normally distributed, this variable was log-transformed. The reporting of the results followed the STROBE guidelines (von Elm et al., 2007). Analyses were carried out using SAS version 9.4 (Cary, NC: SAS Institute Inc).
3. Results
3.1. Patient characteristics
Patients newly diagnosed with depression and stress in 2020 were significantly older (53.5 vs 52.8, and 47.5 vs 46.5, respectively) and more likely male (38.3% vs 37.4%, and 37.8% vs 36.9%, respectively) as compared to those that were diagnosed in the year before. However, patients newly diagnosed with anxiety disorders were significantly younger (51.3 vs 51.5) but still more likely males (36.2% vs 34.5%). On the day of diagnosis, patients newly diagnosed with anxiety and depression disorders received significantly less frequent therapies with antidepressants and benzodiazepines in 2020 than over the years before. The characteristics of patients are depicted in Table 1 .
Table 1.
Sociodemographic characteristics and comorbidities of patients newly diagnosed with anxiety disorder in April–December 2017–2019 and 2020.
| Incident anxiety disorder in April–December 2017–2019 (n = 63,374) | Incident anxiety disorder in April–December 2020 (n = 25,033) | p-value | Incident depression disorders in April–December 2017–2019 (n = 171,542) | Incident depression disorders in April–December 2020 (n = 57,474) | p-value | Incident reaction to severe stress disorders in April–December 2017–2019 (n = 117.950) | Incident reaction to severe stress disorders in April–December 2020 (n = 39,962) | p-value | |
|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic characteristics | |||||||||
| Age in years, mean (SD) | 51.5 (19.0) | 51.3 (19.1) | <0.001 | 52.8 (18.9) | 53.5 (18.9) | <0.001 | 46.5 (16.8) | 47.5 (17.0) | <0.001 |
| Age 18–25 years | 9.6 | 10.7 | <0.001 | 8.4 | 8.6 | <0.001 | 11.8 | 11.8 | <0.001 |
| Age 26–40 years | 22.8 | 23.3 | 20.9 | 20.7 | 28.2 | 27.0 | |||
| Age 41–60 years | 36.2 | 35.2 | 37.6 | 36.4 | 41.2 | 40.5 | |||
| Age 61–80 years | 23.4 | 22.7 | 24.0 | 24.2 | 15.3 | 16.6 | |||
| Age >80 years | 8.0 | 8.1 | 9.1 | 10.1 | 3.5 | 4.1 | |||
| Sex | |||||||||
| Men | 34.5 | 36.2 | <0.001 | 37.4 | 38.3 | <0.001 | 36.9 | 37.8 | <0.001 |
| Women | 65.5 | 63.8 | 62.6 | 61.7 | 63.1 | 62.2 | |||
| Prescribed Therapies* | |||||||||
| Antidepressants | 19.3 | 16.9 | <0.001 | 26.7 | 25.5 | <0.001 | 8.5 | 8.2 | 0.081 |
| Benzodiazepines | 13.2 | 10.2 | <0.001 | 2.8 | 2.9 | 0.633 | 3.7 | 3.4 | 0.011 |
Data are percentages unless otherwise specified.; SD, standard deviation; *Therapy prescribed on the day of diagnosis of patients newly diagnosed with anxiety disorder, depression, or reaction to severe stress in April–December 2017–2019 and 2020.
3.2. Documented incident diseases in 2020 compared to the average of the years before
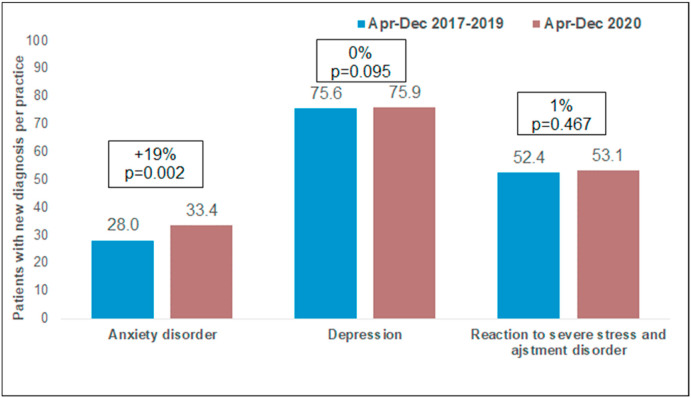
Whereas the number of new incident anxiety disorders recognized significantly increased over the entire calendar year 2020 compared to the years before, there was no change in depression and stress disorders (0% and 1%, respectively). Anxiety diagnoses documented by GPs increased by up to 19% in the calendar year 2020 (Fig. 1 ). When comparing other years, there was no significant increase in the number of new incident diagnoses (from 2017 to 2018: 27.3 vs. 27.9, +2.0%, p = 0.564; from 2018 to 2019: 27.9 vs. 28.0, +0.4%).
Fig. 1.
Average number (per practice) of patients with new anxiety disorder, depression, and adjustment disorder diagnoses in German general practices in April–December 2019 and 2020.
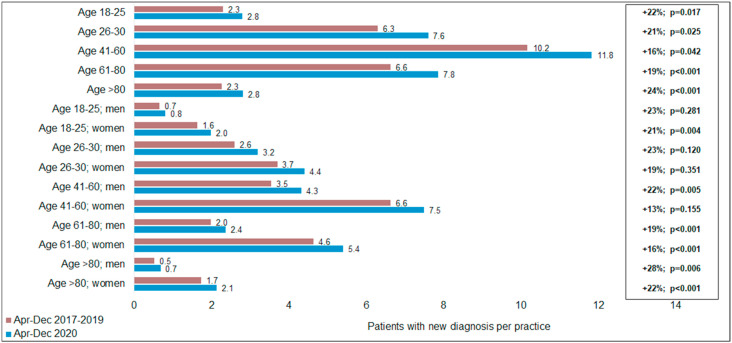
The significant increase of anxiety diagnoses in 2020 compared to the years before was mainly caused by the older population. In the age and sex stratified analysis, in two age groups (41–60 and > 80 years), the increase was stronger in men than in women what may indicate an interaction effect between age group and male sex (Fig. 2 ). In the regression analysis, there was a significant association between age group (p < 0.001) and age-sex-interaction (p = 0.006) and the relative difference in the number of new anxiety patients in 2020 vs 2019. No significant effect was observed for sex alone (p = 0.497).
Fig. 2.
Average number (per practice) of patients with new anxiety disorder diagnoses in German general practices in April–December 2019 and 2020 by age group and sex.
The recognition of new incident anxiety, depression, and stress conditions in GP practices is demonstrated in Table 2 . The population group being 80 and above also received significantly more depression and stress disorders in 2020 than in the years before (Table 2).
Table 2.
Total annual change in new anxiety, depression, stress disorder diagnoses (per practice) in general practices (April–December 2020 compared to April–December 2017–2019).
| Anxiety |
Depression |
Stress |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 2017–2019 |
2020 |
change |
2017–2019 |
2020 |
change |
2017–2019 |
2020 |
change |
|
| mean (SD) | mean (SD) | in % | mean (SD) | mean (SD) | in % | mean (SD) | mean (SD) | in % | |
| Total | 28.07 (26.69) | 33.38 (45.83) | 19** | 75.57 (72.53) | 75.92 (129.3) | 0 | 52.4 (52.39) | 53.07 (58.14) | 1 |
| Sex | |||||||||
| Men | 9.63 (10.27) | 11.95 (24.46) | 24*** | 28.17 (31.82) | 28.64 (64.91) | 2 | 19.27 (21.64) | 19.67 (27.03) | 2 |
| Women | 18.44 (17.87) | 21.43 (24.09) | 16** | 47.4 (43.47) | 47.29 (66.19) | 0 | 33.13 (32.56) | 33.41 (33.72) | 1 |
| Age groups | |||||||||
| 18-25 | 2.73 (3.15) | 3.33 (8.94) | 22* | 6.20 (9.76) | 6.01 (13.63) | −3 | 6.14 (7.62) | 5.93 (9.94) | −3 |
| 26-40 | 6.27 (7.26) | 7.56 (5.39) | 21* | 15.59 (20.90) | 15.16 (41.88) | −3* | 14.69 (17.23) | 14.21 (18.96) | −3 |
| 41-60 | 10.17 (10.73) | 11.82 (15.99) | 16* | 28.55 (28.3) | 28.03 (49.82) | −2* | 21.76 (21.16) | 22.07 (21.89) | 1 |
| 61-80 | 6.63 (7.26) | 7.86 (8.09) | 19*** | 18.27 (16.48) | 19.06 (22.97) | 4 | 8.12 (9.94) | 9.03 (10.79) | 11* |
| >80 | 2.26 (3.38) | 2.81 (3.69) | 24*** | 6.96 (7.16) | 7.77 (7.97) | 12** | 1.84 (3.24) | 2.26 (4.25) | 23* |
*p < 0.05; **p < 0.01; ***p < 0.001.
In contrast to the overall numbers for the entire calendar year 2020, there were differences in documented incident diagnoses. Depression and stress disorders were diagnosed less frequently (−11% and −9%) in the second quarter of the year 2020, where the first strict lockdown was introduced, but more frequently for the third (+3% and +4%) and fourth quarter (9% and 9%, respectively) of 2020 compared to the years before. Again, the oldest-old population has contributed most to the increase in newly diagnosed depression and stress disorders. The data confirmed that the more time passes in the pandemic, the more depression and stress diagnoses were documented. In contrast to the trend of depression and stress disorders, anxiety disorders were documented significantly more often in all quarters of the year 2020 as compared to the corresponding periods of 2017–2019, primarily due to a significant increase of documented diagnoses for the population at the age of 61 and above. However, anxiety diagnoses substantially increased for the younger people (18–25 years) at the end of the year 2020 compared to the second quarter of 2020 (+40% vs 7%). A detailed description of the number of diagnoses documented in GP practices during the second, third and fourth quarters of the year 2020 compared to the corresponding quarters of the years 2017–2019 is demonstrated in Table 3 .
Table 3.
New anxiety, depression, and stress disorder diagnoses (per practice) in general practices in the second, third, and fourth year quarter (April–December 2020 compared to April–December 2017–2019).
| 2nd Quarter |
3rd Quarter |
4th quarter |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2017–2019 |
2020 |
change |
2017–2019 |
2020 |
change |
2017–2019 |
2020 |
change |
||
| mean (SD) | mean (SD) | in % | mean (SD) | mean (SD) | in % | mean (SD) | mean (SD) | in % | ||
| Anxiety disorders | ||||||||||
| Total | 9.05 (9.26) | 10.74 (12.22) | 19*** | 9.68 (9.61) | 11.26 (21.54) | 16 | 9.29 (9.62) | 11.29 (17.67) | 22*** | |
| Sex | ||||||||||
| Men | 3.12 (3.63) | 3.78 (5.13) | 21** | 3.32 (3.86) | 4.08 (12.74) | 23* | 3.17 (3.90) | 4.05 (9.27) | 28*** | |
| Women | 5.93 (6.35) | 6.96 (7.86) | 17** | 6.36 (6.56) | 7.18 (9.92) | 13 | 6.12 (6.47) | 7.23 (9.36) | 18** | |
| Age groups | ||||||||||
| 18-25 | 0.84 (1.26) | 0.86 (1.35) | 3 | 0.93 (1.40) | 1.25 (5.13) | 34* | 0.87 (1.28) | 1.22 (3.61) | 40** | |
| 26-40 | 1.97 (2.69) | 2.26 (3.64) | 14 | 2.27 (7.31) | 2.62 (7.31) | 15 | 2.11 (2.76) | 2.67 (6.55) | 28* | |
| 41-60 | 3.31 (3.91) | 3.97 (5.21) | 20* | 3.52 (4.06) | 3.89 (7.35) | 10 | 3.33 (3.90) | 3.93 (5.83) | 18* | |
| 61-80 | 2.16 (2.77) | 2.64 (3.23) | 22*** | 2.2 (2.68) | 2.6 (3.10) | 18*** | 2.25 (2.89) | 2.59 (3.07) | 15** | |
| >80 | 0.76 (1.31) | 1.01 (1.67) | 32*** | 0.77 (1.42) | 0.92 (1.55) | 19* | 0.73 (1.38) | 0.88 (1.37) | 21*** | |
| Depression disorders | ||||||||||
| Total | 24.71 (26.1) | 21.89 (37) | −11*** | 25.73 (24.76) | 26.57 (39.34) | 3 | 25.13 (25.21) | 27.46 (55.28) | 9 | |
| Sex | ||||||||||
| Men | 9.18 (11.41) | 8.39 (19.56) | −9*** | 9.63 (10.64) | 9.99 (19.65) | 4 | 9.36 (11.60) | 10.25 (26.65) | 10 | |
| Women | 15.53 (16.00) | 13.5 (18.20) | −13*** | 16.1 (15.19) | 16.58 (20.74) | 3 | 15.77 (14.87) | 17.21 (29.23) | 9 | |
| Age groups | ||||||||||
| 18-25 | 2.01 (3.54) | 1.53 (2.91) | −24*** | 2.07 (3.26) | 2.22 (5.14) | 7 | 2.12 (3.75) | 2.25 (6.13) | 6 | |
| 26-40 | 4.99 (7.48) | 4.31 (16.13) | −14*** | 5.42 (7.11) | 5.40 (12.02) | 0 | 5.17 (7.35) | 5.42 (14.50) | 5 | |
| 41-60 | 9.27 (10.23) | 8.05 (14.86) | −13*** | 9.72 (10.16) | 9.56 (14.04) | −2 | 9.56 (9.75) | 10.38 (22.16) | 9 | |
| 61-80 | 6.1 (6.62) | 5.57 (5.39) | −9** | 6.13 (6.02) | 6.59 (7.96) | 7 | 6.03 (6.21) | 6.88 (11.97) | 14 | |
| >80 | 2.34 (2.98) | 2.43 (2.68) | 4 | 2.38 (2.76) | 2.8 (3.47) | 17* | 2.24 (2.76) | 2.53 (3.32) | 13* | |
| Stress disorders | ||||||||||
| Total | 16.95 (17.49) | 15.36 (16.44) | −9** | 17.96 (18.98) | 18.63 (23.11) | 4 | 17.49 (17.88) | 19.08 (22.2) | 9 | |
| Sex | ||||||||||
| Men | 6.2 (7.39) | 5.57 (7.1) | −10*** | 6.68 (8.15) | 6.95 (11.61) | 4 | 6.39 (7.32) | 7.15 (10.56) | 12 | |
| Women | 10.75 (11.05) | 9.8 (10.15) | −9* | 11.28 (11.71) | 11.68 (12.83) | 4 | 11.1 (11.39) | 11.93 (12.78) | 8 | |
| Age groups | ||||||||||
| 18-25 | 2.02 (2.73) | 1.59 (2.25) | −21*** | 2.06 (3.01) | 2.15 (5.28) | 5 | 2.04 (2.78) | 2.13 (3.58) | 5 | |
| 26-40 | 4.67 (5.66) | 3.83 (5.06) | −18*** | 5.15 (6.66) | 5.16 (7.70) | 0 | 4.83 (6.01) | 5.10 (7.62) | 6 | |
| 41-60 | 6.98 (7.44) | 6.34 (6.67) | −9** | 7.36 (7.67) | 7.50 (8.34) | 2 | 7.36 (7.44) | 8.04 (8.76) | 9 | |
| 61-80 | 2.66 (3.60) | 2.84 (3.76) | 7 | 2.76 (3.74) | 3.09 (3.96) | 12** | 2.67 (3.54) | 3.02 (4.17) | 13 | |
| >80 | 0.62 (1.33) | 0.76 (1.66) | 21 | 0.63 (1.25) | 0.71 (1.50) | 14 | 0.59 (1.26) | 0.78 (1.68) | 33** | |
*p < 0.05; **p < 0.01; ***p < 0.001.
4. Discussion
This analysis provides valuable information on the documentation of incident anxiety, depression, and stress disorders in primary care during the year 2020 that was tremendously affected by the COVID-19 infection and the imposed measures. The results demonstrated an increase in anxiety disorders, especially for the elderly population. This population group seems to be affected mainly by the pandemic and its imposed measures, developing significantly more frequently depression and stress disorder in the year 2020 compared to the years before. The longer the pandemic lasts, the more mental health diagnoses were documented in 2020, which could be related to the enormous burden of the imposed measures to prevent the spread of the COVID-19 diseases. The younger population was diagnosed more frequently with anxiety disorders at the end of 2020, nine months after the first lockdown was imposed in Germany. The increase in depression and stress disorder in the third and fourth quarter could be seen as compensating effects of the tremendous decrease during the second quarter in 2020, where the first lockdown was imposed. However, these compensational effects were minor, not exceeding the initial reduction of recommended and documented mental health diagnoses.
Several systematic reviews and meta-analyses (Cenat et al., 2021; Deng et al., 2021; Ren et al., 2020) revealed that the prevalence of mental disorders was more than 3-fold higher during the COVID-19 pandemic compared to the times before (Ettman et al., 2020; Lakhan et al., 2020; T. Wu et al., 2021). The study of Wu et al. (T. Wu et al., 2021) revealed a pooled prevalence of 31%, 32% and 41% for depression, anxiety, and stress, respectively. However, mental health problems vary broadly across different countries (Zurcher et al., 2020). In Germany, several studies revealed that the COVID-19-pandemic significantly worsened individuals' mental health, but the heightened levels of mental disorders were lower than studies from other counties (Bauerle et al., 2020; Skoda et al., 2020, 2021).
Several methodological, response, pandemic, and health policy-related factors need to be considered when trying to gain a broader perspective on the prevalence of mental health problems during the COVID-19 pandemic (Richter et al., 2021). The number of COVID-19 cases in Germany was much lower during the year 2020 than in the United Kingdom, France, Italy, and Spain. Differences in the reported prevalence of mental disorders could be caused by the different severity of the pandemic and the countries' lockdown strengths. Richter et al. (2021) highlighted that mental health care utilization indicators did not suggest an increased demand during the first lockdown phase, which is in line with our results. Also, Moradian et al. (2021) demonstrated the impact of COVID-19 on patients mental health in Germany using longitudinal data, revealing a prolonged negative impact on people's mental health in Germany despite the fact that less intensive restrictions were introduced during the second lockdown compared to the first, which may be interpreted as pandemic fatigue. This is in line with this analysis' results, demonstrating that anxiety disorders were documented more often the more prolonged the COVID-19 pandemic and its imposed measures last.
Differences in the prevalence of mental illnesses could also be caused by the different methods used to assess patients' mental health. Most of the previously published prevalence rates of mental health were based on surveys. The early insights into the population's mental health might be valuable but have to be interpreted with caution because they could be prone to substantial bias. Most surveys were carried out online using membership lists, existing large convenience samples, or social media. Bias can affect any study but can be particularly problematic in mental health surveys (Pierce et al., 2020). Even though most of the previously published surveys were based on standardized and well-validated psychometric mental health assessment tools, individuals with existing or severe mental health problems are more likely to participate than those without such conditions. This could partly explain the differences between the high prevalence of mental health in health surveys and the lower prevalence of documented mental health diagnoses in a more representative sample of GP practices.
On the one hand, these differences could be related to patients' behaviours concerning the primary care system's utilization during the pandemic. Patients became aware and very concerned about the seriousness of the situation and the risk of infection, especially in medical practices and hospitals. Betsch et al. (Betsch, 2020) revealed that more than 70% of the population were (very) concerned about COVID-19 at the beginning of March, very early on in the COVID-19 pandemic. This study revealed that diagnosis trends varied during the different periods of the year, tremendously falling at the beginning of the year where the first strict lockdown was imposed and, afterward, slightly compensated. Various studies have evaluated the impact of the COVID-19 pandemic on patients' utilization of healthcare services during COVID-19 (Guo et al., 2020; Haffer et al., 2020; Houshyar et al., 2020; Hoyer et al., 2020; Kenyon et al., 2020; Lu et al., 2007; Michalowsky et al., 2021), demonstrating a remarkable reduction of hospital and physician services and recognition of incident diagnoses during the first waves. Michalowsky et al. (2021) revealed that the decrease in recognition of incident diseases was twice as large as the decrease in the utilization of GPs during the first lockdown in Germany.
Therefore, it can reasonably be assumed the decreasing healthcare utilization trends at the beginning of the COVID-19 pandemic, and the missing compensational effects were caused by patients' concerns about infection with COVID-19 in primary care practices. Additionally, it seems that patients prefer not to be treated or treated only in more severe illness during the period with higher infection risk. This, in turn, would mean that even if patients were subjectively stressed, depressed or anxious, these burdens, in the perception of the affected patients, were not severe enough to require medical treatment and care provided by practitioners. This could be particularly evident among the younger populations, being generally less ill and utilizing less frequent healthcare services than the older population. The increase in mental health problems could be seen as general distress that is to be expected during global health crises (Richter et al., 2021).
Several studies revealed that particularly young and female individuals with lower social and economic resources, and greater exposure to stressors, like job loss or loneliness, reported a more significant mental burden (Ettman et al., 2020; Liu et al., 2021; Riedel-Heller and Richter, 2020). Contrary to this, older adults reported lower stress (Adamson et al., 2020). All of this is contrary to our findings, where the elderly population contributed most to the dramatic increase of anxiety, depression, and stress disorders in 2020 compared to the years before. This analysis revealed a consistent rate of mental illness for the younger population over the entire calendar year 2020. Solely at the end of 2020, nine months after introducing the first imposed lockdown in Germany, a higher risk for mental health illnesses was demonstrated.
The elderly population is at a higher risk of complications in the clinical course of COVID-19 and are more likely to die (Ji et al., 2020; Lian et al., 2020). Thus, the elderly population became aware and very concerned about the risk of infection and the progression of the COVID-19 disease. Also, the elderly population was affected most by the introduced measures to prevent the spread of the COVID-19 diseases and asked to reduce their mobility and social contacts as much as possible. Therefore, it can reasonably be assumed that the tremendous increase in the elderly population's mental health diagnoses was associated with the long-lasting pandemic crisis, its imposed measures, and the higher risk for this specific population group. For the younger population, the impact of the COVID-19 pandemic becomes more profound the longer the pandemic lasted. This could be caused by the prolonged stress and strain of balancing work and life, especially if children had to be cared for at home. Our results revealed 30% more anxiety diagnoses in this population group nine months after the first imposed lockdown than in the corresponding period of previous years. This may reflect the dramatic situation the younger population was faced with and that they may no longer be able to cope with the stress caused by the imposed measures to prevent the ongoing spread of Covid-19.
Further research is needed to analyze the differences between the subjective and objective measures and the long-term consequence of delayed recognition of mental diseases and initiation of necessary treatment and care. This evidence should be used to guide governmental action in mitigating the mental and physical health consequences of the COVID-19 lockdown. Strategic considerations are urgently needed regarding implementing a strategy to maintain diagnosis, treatment, and care during lockdowns and pandemic phases, especially for the elderly population. This includes the patients' conditions during the pandemic, characterized by social isolation, which could cause additional severe mental health problems (Gerst-Emerson and Jayawardhana, 2015; Santini et al., 2020).
5. Limitations
First, the data documentation may be less accurate than usual due to physician practices' organizational challenges and the circumstances during the COVID-19 pandemic. Second, it is impossible to assess the extent to which emergency, urgent, and deferrable services have been provided within the available diagnostic categories. Third, this considerably limits an assessment of whether the appropriate guidelines for diagnosis and treatment strategies have been followed in the individual medical practices because of the high-risk situation and the lockdown. Also, special circumstances in 2017, 2018 or 2019, such as the wave of influenza that was averted in 2020, may have influenced the results. Fourth, data pertaining to socioeconomic status (e.g., education and income), and lifestyle-related risk factors (e.g., smoking, alcohol, and physical activity) were lacking. Fifth, database used does not contain information on disease severity and mortality. Sixth, the number of patients with mental disorder diagnoses may be underestimated due to the decrease of physician consultations during the Covid-19 pandemic. Seventh, due to data protection rules no investigation was possible, whether the changes in incident mental disorder diagnoses differ between German federal states. Eighth, analyses were performed for age groups and separately mean and women, however no interaction between age and sex was analyzed. Ninth, this is only a descriptive analysis without hypothesis testing using the multivariable regression models. Finally, the database does not allow for the establishment of a patient-related connection between different specialists. Therefore, double reporting of patients' diagnoses cannot be precluded.
6. Conclusion
COVID-19 poses novel challenges for patients that have been exposed to considerable risks and stress. Over the entire period of 2020, stress and depression diagnoses remained stable. Only anxiety disorders were elevated compared to the years before the pandemic, which is not in line with previously published studies that revealed a three-fold higher prevalence of such conditions. These differences can be explained mainly because objective measures, like documented diagnoses by practitioners, did not correspond well with patients' subjective perceptions. Thus, the novel and COVID-19 related challenges caused a substantial burden for the population. Anxiety disorders were documented significantly more frequently over the entire year, especially among the elderly who are most at risk for COVID-19-related deaths. The elderly population was also more often affected by depression and stress, underlining the strain of Covid-19 for this population group. However, also for the younger people, significantly more anxiety disorders were diagnosed later on. The elderly population was exposed to a higher risk for progression of the Covid-19 diseases. The younger population was exposed to higher stress due to balancing work and life during the imposed lockdowns, particularly the longer the pandemic lasts. Our results revealed that fewer mental health diagnoses were diagnosed within the first lockdown period and that compensatory effects, later on, demonstrated by a higher disease detection rate, were smaller. The long-term effects of the altered disease detection rate in the elderly population should be evaluated.
Declaration of competing interest
JB received consultant fees from the companies Wilmar Schwabe and Biogen. BM received consultant fees from Biogen. The other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
The authors have received no financial support for the research, authorship, and/or publication of this article.
Author contributions
Bernhard Michalowsky and Jens Bohlken contributed to the design of the study, managed the literature searches, wrote the first draft of the manuscript, and corrected the manuscript. Steffi Riedel-Heller and Wolfgang Hoffmann corrected the manuscript. Karel Kostev contributed to the design of the study, performed the statistical analyses, and corrected the manuscript. All authors contributed to and have approved the final manuscript.
Acknowledgements
This work was not funded.
References
- Adamson M.M., Phillips A., Seenivasan S., Martinez J., Grewal H., Kang X., Spiegel D. International prevalence and correlates of psychological stress during the global COVID-19 pandemic. Int. J. Environ. Res. Publ. Health. 2020;17(24) doi: 10.3390/ijerph17249248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauerle A., Teufel M., Musche V., Weismuller B., Kohler H., Hetkamp M., et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health. 2020;42(4):672–678. doi: 10.1093/pubmed/fdaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benke C., Autenrieth L.K., Asselmann E., Pane-Farre C.A. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatr. Res. 2020;293:113462. doi: 10.1016/j.psychres.2020.113462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betsch C. In: Erfurt U., editor. 2020. Ergebnisse aus dem COVID-19 Snapshop MOnitoring COSMO: die psychologische Lage.https://projekte.uni-erfurt.de/cosmo2020/archiv/ [Google Scholar]
- Cenat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatr. Res. 2021;295:113599. doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schunemann H.J., Covid- Systematic Urgent Review Group Effort study Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Y., Chen Y., Zhang B. Different prevalence trend of depression and anxiety among healthcare workers and general public before and after the peak of COVID-19 occurred in China: a meta-analysis. Asian J. Psychiatr. 2021;56:102547. doi: 10.1016/j.ajp.2021.102547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerst-Emerson K., Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am. J. Publ. Health. 2015;105(5):1013–1019. doi: 10.2105/AJPH.2014.302427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass R.J., Glass L.M., Beyeler W.E., Min H.J. Targeted social distancing design for pandemic influenza. Emerg. Infect. Dis. 2006;12(11):1671–1681. doi: 10.3201/eid1211.060255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H., Zhou Y., Liu X., Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J. Dent. Sci. 2020 doi: 10.1016/j.jds.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffer H., Schomig F., Rickert M., Randau T., Raschke M., Wirtz D., et al. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery in university hospitals in Germany: results of a nationwide survey. J. Bone Joint. Surg. Am. 2020 doi: 10.2106/JBJS.20.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetkamp M., Schweda A., Bauerle A., Weismuller B., Kohler H., Musche V., et al. Sleep disturbances, fear, and generalized anxiety during the COVID-19 shut down phase in Germany: relation to infection rates, deaths, and German stock index DAX. Sleep Med. 2020;75:350–353. doi: 10.1016/j.sleep.2020.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway R., Rasmussen S.A., Zaza S., Cox N.J., Jernigan D.B. Updated preparedness and response framework for influenza pandemics. MMWR Recomm. Rep. (Morb. Mortal. Wkly. Rep.) 2014;63(RR-06):1–18. [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houshyar R., Tran-Harding K., Glavis-Bloom J., Nguyentat M., Mongan J., Chahine C., et al. Effect of shelter-in-place on emergency department radiology volumes during the COVID-19 pandemic. Emerg. Radiol. 2020 doi: 10.1007/s10140-020-01797-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyer C., Ebert A., Szabo K., Platten M., Meyer-Lindenberg A., Kranaster L. Decreased utilization of mental health emergency service during the COVID-19 pandemic. Eur. Arch. Psychiatr. Clin. Neurosci. 2020 doi: 10.1007/s00406-020-01151-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji M., Yuan L., Shen W., Lv J., Li Y., Chen J., et al. A predictive model for disease progression in non-severely ill patients with coronavirus disease 2019. Eur. Respir. J. 2020;56(1) doi: 10.1183/13993003.01234-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenyon C.C., Hill D.A., Henrickson S.E., Bryant-Stephens T.C., Zorc J.J. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J. Allergy Clin. Immunol. Pract. 2020 doi: 10.1016/j.jaip.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakhan R., Agrawal A., Sharma M. Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J. Neurosci. Rural Pract. 2020;11(4):519–525. doi: 10.1055/s-0040-1716442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapolla P., Mingoli A., Lee R. Deaths from COVID-19 in healthcare workers in Italy-What can we learn? Infect. Control Hosp. Epidemiol. 2020:1–2. doi: 10.1017/ice.2020.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lian J., Jin X., Hao S., Cai H., Zhang S., Zheng L., et al. Analysis of epidemiological and clinical features in older patients with coronavirus disease 2019 (COVID-19) outside Wuhan. Clin. Infect. Dis. 2020;71(15):740–747. doi: 10.1093/cid/ciaa242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Heinzel S., Haucke M.N., Heinz A. Increased psychological distress, loneliness, and unemployment in the spread of COVID-19 over 6 Months in Germany. Medicina. 2021;57(1) doi: 10.3390/medicina57010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu T.H., Chou Y.J., Liou C.S. Impact of SARS on healthcare utilization by disease categories: implications for delivery of healthcare services. Health Pol. 2007;83(2–3):375–381. doi: 10.1016/j.healthpol.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansfield K.E., Mathur R., Tazare J., Henderson A.D., Mulick A.R., Carreira H., et al. Indirect acute effects of the COVID-19 pandemic on physical and mental health in the UK: a population-based study. Lancet Digit Health. 2021 doi: 10.1016/S2589-7500(21)00017-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicine, Johns Hopkins University Corona virus resource center. 2020. https://coronavirus.jhu.edu/map.html
- Michalowsky B., Hoffmann W., Bohlken J., Kostev K. Effect of the COVID-19 lockdown on disease recognition and utilisation of healthcare services in the older population in Germany: a cross-sectional study. Age Ageing. 2021;50(2):317–325. doi: 10.1093/ageing/afaa260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradian S., Bauerle A., Schweda A., Musche V., Kohler H., Fink M., et al. Differences and similarities between the impact of the first and the second COVID-19-lockdown on mental health and safety behaviour in Germany. J. Public Health. 2021 doi: 10.1093/pubmed/fdab037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan K.Y., Kok A.A.L., Eikelenboom M., Horsfall M., Jorg F., Luteijn R.A., Penninx B.W.J.H. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. 2021;8(2):121–129. doi: 10.1016/S2215-0366(20)30491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., McManus S., Jessop C., John A., Hotopf M., Ford T., et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7(7):567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathmann W., Bongaerts B., Carius H.J., Kruppert S., Kostev K. Basic characteristics and representativeness of the German Disease Analyzer database. Int. J. Clin. Pharm. Ther. 2018;56(10):459–466. doi: 10.5414/CP203320. [DOI] [PubMed] [Google Scholar]
- Ren X., Huang W., Pan H., Huang T., Wang X., Ma Y. Mental health during the Covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 2020;91(4):1033–1045. doi: 10.1007/s11126-020-09796-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter D., Riedel-Heller S., Zurcher S.J. Mental health problems in the general population during and after the first lockdown phase due to the SARS-Cov-2 pandemic: rapid review of multi-wave studies. Epidemiol. Psychiatr. Sci. 2021;30:e27. doi: 10.1017/S2045796021000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedel-Heller S., Richter D. [COVID-19 pandemic and mental health of the general public: is there a tsunami of mental disorders?] Psychiatr. Prax. 2020;47(8):452–456. doi: 10.1055/a-1290-3469. [DOI] [PubMed] [Google Scholar]
- RKI, Robert Koch Institute . 2020. COVID-19-Dashboard.https://experience.arcgis.com/experience/478220a4c454480e823b17327b2bf1d4 [Google Scholar]
- Santini Z.I., Jose P.E., York Cornwell E., Koyanagi A., Nielsen L., Hinrichsen C., Koushede V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62–e70. doi: 10.1016/S2468-2667(19)30230-0. [DOI] [PubMed] [Google Scholar]
- Skoda E.M., Bauerle A., Schweda A., Dorrie N., Musche V., Hetkamp M., Weismuller B. Severely increased generalized anxiety, but not COVID-19-related fear in individuals with mental illnesses: a population based cross-sectional study in Germany. Int. J. Soc. Psychiatr. 2020 doi: 10.1177/0020764020960773. 20764020960773. [DOI] [PubMed] [Google Scholar]
- Skoda E.M., Spura A., De Bock F., Schweda A., Dorrie N., Fink M., et al. [Change in psychological burden during the COVID-19 pandemic in Germany: fears, individual behavior, and the relevance of information and trust in governmental institutions] Bundesgesundheitsblatt - Gesundheitsforsch. - Gesundheitsschutz. 2021;64(3):322–333. doi: 10.1007/s00103-021-03278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E., Altman D.G., Egger M., Pocock S.J., Gotzsche P.C., Vandenbroucke J.P. Initiative, Strobe. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Trav. Med. 2020;27(2) doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P., Hao X., Lau E.H.Y., Wong J.Y., Leung K.S.M., Wu J.T., et al. Real-time tentative assessment of the epidemiological characteristics of novel coronavirus infections in Wuhan, China, as at 22 January 2020. Euro Surveill. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zurcher S.J., Kerksieck P., Adamus C., Burr C.M., Lehmann A.I., Huber F.K., Richter D. Prevalence of mental health problems during virus epidemics in the general public, health care workers and survivors: a rapid review of the evidence. Front. Publ. Health. 2020;8:560389. doi: 10.3389/fpubh.2020.560389. [DOI] [PMC free article] [PubMed] [Google Scholar]