ABSTRACT
Background: Frederick Banting approached Toronto physiology professor JJR Macleod with a way to prevent pancreatic trypsin from destroying the pancreas’ internal secretion. Banting proposed to induce exocrine atrophy by ligating canine pancreatic ducts and to use extracts of islet-rich residua to treat pancreatectomized dogs. His next plan was to make extracts from fetal pancreas, which he had read was islet-rich and lacked exocrine tissue capable of making trypsin; this work has not been historically evaluated. Methods: Banting’s fetal calf pancreas story is told using primary and secondary historical sources and then critically examined using both historical and recent data on species phylogeny, islet ontogeny, fetal/neonatal islet culture/transplantation, etc. Results/Discussion: Only ruminants develop dual islets populations sequentially; fetal calf pancreata, at the gestational ages Banting used, possess numerous insulin-rich giant peri-lobular islets, which credibly explain the potency of his fetal calf insulin extract. Use of non-ruminant fetal pancreata would have failed.
KEYWORDS: Medical history, discovery of insulin, Frederick Banting, Charles Best, Edouard Laguesse, islet development, islet histology, ruminant, fetal calf, fetal sheep
Background
While it is difficult to pick an exact date, the centenary of the discovery of insulin in Toronto is nigh upon us. Some readers may consider this to be the summer of 1921, when Frederick Grant Banting (1891–1941) and Charles Herbert Best (1899–1978) injected depancreatized diabetic dogs with extracts made from duct-ligated dog pancreata. Others recognize that Georg L. Zuelzer (1870–1949) of Berlin, Ernest Lyman Scott (1877–1966) at University of Chicago, Israel S. Kleiner (1885–1966) at the Rockefeller Institute in New York City, and Nicolas C. Paulesco (1869–1931) of Bucharest published similar promising results in animals, and, therefore, consider Toronto’s primacy in the discovery to have been unequivocally sealed by the injection of a purified extract produced by James Bertram Collip (1892–1965) into a adolescent boy in diabetic ketoacidosis on January 23, 1922; Collip’s extract normalized Leonard Thompson’s blood glucose levels, revived his consciousness, and his ketonuria disappeared; all of this was accomplished without toxic side effects. No other investigators could claim definitive clinical results. While there are many old sources on the history of insulin, Michael Bliss (1941–2017) is widely recognized for providing the definitive scholarly history of insulin,1,2 and I have used his chronology.
Most histories of the discovery of insulin start with Banting’s “great idea.” While the general story is well-known, it will be briefly summarized. After returning from service in World War I, Banting, a young Canadian surgeon, started an unsuccessful private practice in London, Ontario and was supplementing his income by providing medical school lectures. While preparing a lecture on diabetes, he read a paper by Moses Baron (1884–1978) on the evening of Sunday October 31, 1920 which tweaked an idea of how to prove the existence of the elusive internal secretion of the pancreas. Colleagues suggested Banting approach University of Toronto (UofT) physiology professor John James Rickard Macleod (1876–1935) and present his nascent great idea, which involved ligating pancreatic ducts in dogs to induce pancreatic atrophy, and then transplanting the residual islet–rich tissue into depancreatized diabetic dogs. After some initial discouragement, Macleod agreed to supervise the research and offered Banting access to laboratory space, a dozen dogs, and two student assistants. It is not entirely clear how the decision was made to produce an extract of degenerated pancreas rather than transplant it; this is discussed in detail elsewhere.3 The two summer students, Best and E. Clark Noble (1900–1978),4 flipped a coin to determine who would work with Banting first. One month later, Macleod went on vacation to Scotland. Banting and Best worked in the heat of the summer, with much failure but scattered success. While Macleod offered occasional helpful advice through correspondence, Banting became increasingly bitter about his working conditions and other simultaneous disappointing aspects of his life. Because it had taken considerable time for Best to become a competent surgical assistant, it was agreed that, for the good of the project, Noble would not replace him and that Best would continue working with Banting.1,2,4 When Macleod returned at the end of the summer, he raised some legitimate issues needing to be addressed but found the results sufficiently promising to continue and worthy of additional resources. At Banting’s request, Macleod asked Collip, an University of Alberta biochemistry professor on sabbatical in Toronto, to join the insulin team, which occurred on December 12, 1921. Using intact adult bovine pancreata, Collip quickly made more potent extracts; one of these was used at Toronto General Hospital to successfully treat Leonard Thompson (1908–1935) on January 23, 1922. The initial supply of insulin was erratic, and the already strained dynamics within the Toronto insulin team further deteriorated as Banting believed Macleod and Collip were trying to steal credit that rightfully belonged to him and Best. Banting was further incensed when he and Macleod were co-recipients of the 1923 Nobel Prize in Physiology and Medicine, as Banting did not believe that Macleod had made important contributions to the discovery. Banting shared his half of the award money with Best, and Macleod shared his half with Collip.1,2 While multiple pre-1980 histories of insulin have minimized Macleod’s role (and some have even presented him as lacking academic integrity), Bliss’ books and his other writings have firmly established Macleod’s contributions as worthy of his Nobel Laureate status. Sadly, the discovery of insulin was a source of great interpersonal conflict and brought little happiness to its discoverers.5
The Great Idea Was a Bad Idea
Banting’s great idea was wrong, but Banting’s unwavering belief in it powered Banting and Best through the hot and miserable summer of 1921. Months were spent ligating pancreatic ducts in dogs and then waiting for the pancreas to degenerate. Sometimes atrophy occurred and sometimes it did not. According to Bliss, Banting “never realized that he and Best made a serious error on August 17 when they did not recognize that an extract they had made from fresh whole pancreas was just as effective … as extract of duct-ligated pancreas. Had they reflected on this result (it threw the fundamental hypothesis about duct-ligation and atrophication into question) Banting and Best might have speeded up the work by months.”3p20 While the results they generated during the summer of 1921 supported the existence of an internal secretion, their results were no more definitive than some of their predecessors.1,2
Banting and Best began writing their initial paper describing the treatment of depancreatized dogs with extracts from duct-ligated, degenerated dog pancreata in the late autumn of 1921 and it was published in February 1922 in the Journal of Laboratory and Clinical Medicine.6 Macleod’s presence on the journal’s editorial board was undoubtedly responsible for its rapid publication. It was immediately clear to some readers that Banting’s great idea did not make physiological sense. Ffrangcon Roberts, a Cambridge physician who had published a textbook of physiology in 1920, published a scathing review in the December 16, 1922, issue of the British Medical Journal.7 Bliss succinctly summarized Roberts’ analysis:
The work began there with Banting’s hypothesis that it was necessary to protect the internal secretion of the pancreas from the powerful external secretion, the proteolytic enzyme trypsin, by ligating the pancreatic ducts to cause the trypsin-producing cells to atrophy. Roberts declared that the hypothesis was simply false. “Now it is one of the best established facts in physiology,” he [Roberts] wrote, “that the proteolytic enzyme exists in the pancreas in an inactive form – trypsinogen – which is activated normally on contact with another ferment, enterokinase, secreted by the small intestine.” Roberts allowed that trypsinogen is also activated when a pancreas is cut out and begins to deteriorate, but this happens only slowly and can easily be prevented by chilling. Given these facts, there was no physiological basis at all for Banting and Best’s duct ligation experiment. They had undertaken a cumbersome, time-consuming process to forestall enzyme action which would never have taken place … Roberts examined Banting and Best’s experiments carefully and critically. In passing, he pointed out some factual disparities between the charts and text … [using their own published data, Roberts built a case that] Banting and Bests’ own evidence showed the incorrectness of their working hypothesis.1p203-204
Current historians of insulin generally agree that Banting’s great idea (i.e., duct ligation) played no essential part in the discovery of insulin – other than that Banting and Best’s findings during the summer of 1922 convinced Macleod to focus his laboratory on the purification, characterization, and clinical application of insulin. Joseph H. Pratt (1872–1956) built a compelling and often cited argument for this almost 70 y ago.8 Much speculation has focussed on how Macleod, a world-renowned physiologist who wrote medical student textbooks that specifically mentioned trypsinogen’s inactivity, missed this. Because of this oversight, which was obvious to some scientists but not the lay public celebrating Banting’s great idea, British MRC Director Sir Henry H. Dale (1875–1968) once quipped “insulin could only have been discovered in a lab whose director was slightly stupid.1p278,FN38” Regardless, although Banting and Best had generated some promising results, duct ligation was a slow, tedious, and prohibitively expensive means of generating pancreatic extract.6 Banting’s next idea came straight out of a physiology laboratory demonstration he had attended when he was a medical student at UofT.
From mid-August to mid-September, Banting and Best's supply of duct-ligated donor dogs was almost depleted. Banting describes what happened next in his Cameron Prize Lecture (30 October 1928):
By the administration of extract from five degenerated pancreases the [depancreatized] dog was maintained in good condition for eight days. At the end of this time we had used up all the available supply of what we then called “isletin.” The severe symptoms of diabetes became evident. About three o’clock in the morning, while watching the development of terminal symptoms, it occurred to me that it might be possible to get rid of the toxic materials associated with the products of the acinous cell in another manner … It was hoped that the classroom experiment of injecting secretin to stimulate the production of pancreatic juice could be continued long enough to exhaust the acinous cells. … [One extract from a secretin-stimulated pancreas worked but they could not repeat these results and the dog died 20 days after pancreatectomy]. [Banting concluded:] The exhausted gland extracts were not practical, but they served as contributory evidence in favour of the main theory of obtaining extracts of the island cells free from the products of the acinous cells.9p5-6
Bliss’ summary of these studies was simply that this “short-cut had not worked at all satisfactorily.”1p91
Banting’s Second Great Idea
Macleod returned to Toronto on September 21, 1921, and he reviewed Banting and Best’s work. He had them complete a long overdue review of the literature. On November 14, Banting presented his and Best’s work at a departmental journal club, where a young UofT physiologist suggested a longevity study to determine how long pancreatic extracts could keep a depancreatized dog alive. Macleod and Banting agreed this was worthwhile, but there was still an acute shortage of duct-ligated dogs. In fact, there was only one available, and generating more would involve many delicate operations on many dogs as well as a hiatus of 4–7 weeks while the pancreata degenerated in vivo. Therefore, the longevity study could not proceed. In a moment of desperation, Banting came up with the idea of using fetal calf pancreas as a source of isletin.1,2 In his Cameron Lecture, he describes this eureka moment (2 AM on November 16), which hereafter will be called his “second great idea.” According to Banting:
It was then inevitable that a more practical means of obtaining extract must be found if progress was to be made. [Edouard] Laguesse had found that there were relatively more islet cells in the pancreas of a new-born than in the adult pancreas. The first idea was to extract the pancreas of new-born animals. It seemed reasonable to conclude that the pancreas of a partly developed foetus might contain even more abundant islet cells. It was finally conjectured that if one could obtain the pancreas of a foetus at the end of the first third of pregnancy that the internal secretion of the islet cells would be present since other internal secretions (e.g. epinephrine) are present at this stage of development. At the same time, it seemed reasonable to conclude that since digestion is not called into play till after the birth of the animal that there would not be powerful digestives present in the foetus. Having been born and raised on the farm, and being familiar with stock-breeding, I knew that cattle are frequently bred before fattening in order to make better feeders. There would therefore be plenty of foetal calves available at the abattoirs. The next morning at nine o’clock, having obtained sterile instruments and containers, Mr. Best and I proceeded to the abattoir where we obtained the pancreases of nine foetal calves varying from three to four months’ gestation [NB, Gestation period for cows range is 279-287 days; mean is 283 days (9.1 mo). Normal for humans is 280 days].
An extract was made in the usual way and carefully administered intravenously to a depancreatised dog on 19th November 1921. Following the injection the blood sugar fell from 0.33 to .017 in one hour. This result was confirmed by subsequent injections. We were thus able to maintain an adequate supply of the active principle of the islands of Langerhans with no expense to the laboratory, and in quantities which provided for repeated trials and various extractions. It was found that the active principle could be extracted from the foetal gland with acetone and alcohol, and that it was not destroyed by chloroform or ether.9p6-7
Banting and Best published these results and then moved on to extracting adult bovine pancreata. Their second paper was published in the May 1922 issue of the Journal of Laboratory and Clinical Medicine.10 The paper concluded: “By intravenous and subcutaneous injections of neutral saline extracts prepared from the pancreas of bovine fetus at about the fifth month, the percentage of blood sugar and the daily urinary excretion of sugar are markedly reduced in depancreated dogs. Daily injections of extract of pancreas enabled a depancreatized dog to live for seventy days … .The depressor action of the extract is short-lived.”10p472
Other Historical Sources on the Second Great Idea
All historical coverage on the discovery of insulin herald the use of fetal bovine pancreas to keep a longevity dog (Figure 1) alive as an important breakthrough.1–3,9,11–16 Even books for children of various ages (and print sizes) on the discovery of insulin include this story.17–19 Strangely, while the facts related to the discovery of insulin have remained disputed and controversial for a century, the fetal calf pancreas story has always been taken at face value and has never been critically evaluated; in most sources, it is covered in a few short paragraphs, and then the story quickly moves on.
Figure 1.
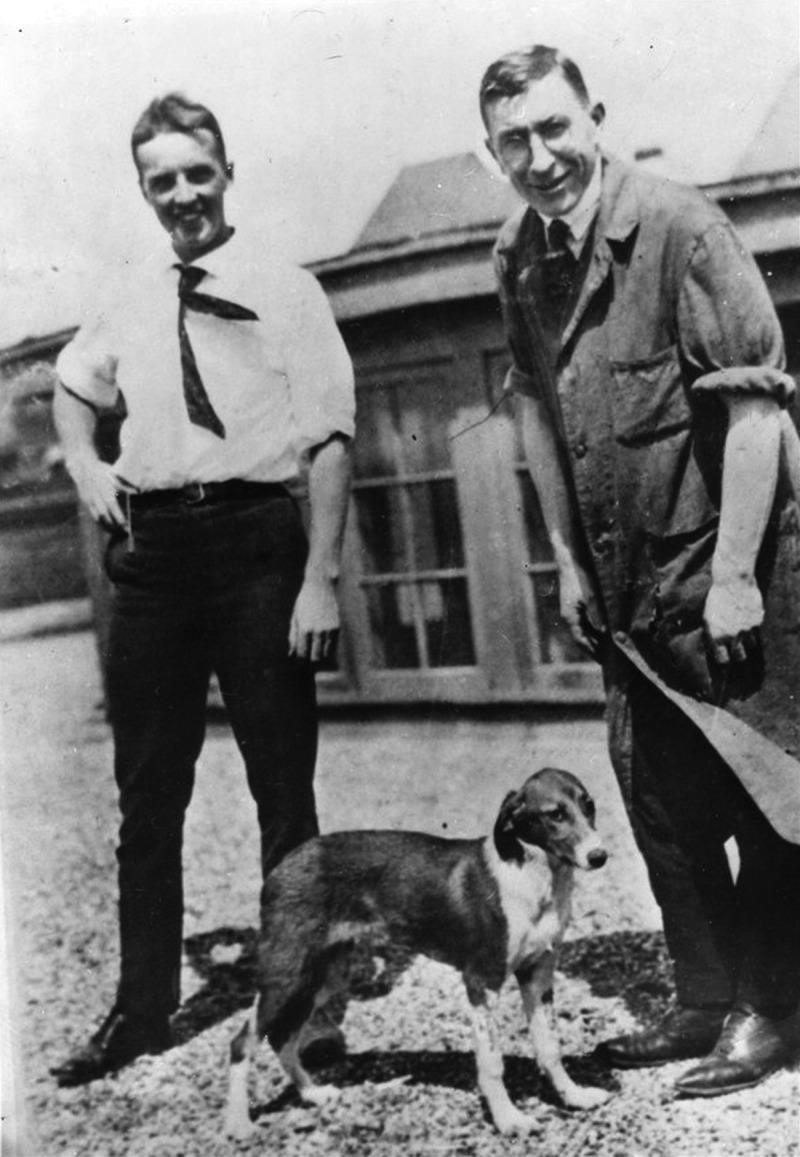
Charles Best (left) and Frederick Banting (right) posing on the roof of the Medical Building with a dog. Sources disagree with regards to the date and whether this is the longevity dog treated with extract derived from fetal calf pancreata
A few additional details are found in some sources. Bliss’ The Discovery of Insulin notes that, minutes before his eureka moment, “Banting first thought of obtaining foetal pancreases by producing abortion in dogs.”1p92 Bliss, who was a corporate and business historian before focusing on medical history, even identified the abattoir – “William Davies Company in northwest Toronto”1p92 and was personally aware of its history.20 It is, perhaps, ironic that fetal calves were utilized in Hogtown, Toronto’s nickname after the early 1900s. In the early 20th century, the William Davies Company, the largest pork-packing operation in the British Empire, was slaughtering half a million hogs a year and exporting most of the product to Britain.20 As will be demonstrated below, had Banting used fetal piglets, his second great idea would also have failed. Fortunately, Banting was already focused on cattle, as six weeks earlier (October 4), Banting and Best had visited Connaught farm (the location of UofT’s Connaught Anti-Toxin Laboratories) and tried to ligate the pancreatic ducts of a calf, but it died from the anesthetic.1p85 Hidden in a footnote, Bliss also reports that “Connaught gave them three calves for exhausted gland [secretin] experiments,” but that “there are no [further] records of these.”1p259,FN5 Bliss’ sequel, Banting: A Biography, covers the entire fetal calf topic in two short paragraphs and does not provide any additional details.2
Medical historian Lloyd G. Stevenson (1918–1988), who authored the definitive Banting biography prior to Bliss, notes that Banting said that fetal bovine extract was only used on depancreatized dogs but was “the most potent thing tried.”11p104 In this book, which describes these events by simply quoting Banting’s Cameron Lecture, Stevenson appends a footnote: “Banting speaks here as if this had all been a matter of conjecture except for the discovery made by Laguesse of the relatively more abundant islet cells in the pancreas of a new-born animal. It had been demonstrated by Ibrahim, however, that the pancreas … up to the fourth month of intrauterine life contains no active proteolytic enzyme (i.e., digestive ferment) while the experiments of Carlson and Drennan seemed to indicate the presence of a substance producing hypoglycemia.”11p90
Banting and Best freely acknowledged that the studies of Ibrahim21 and Carlson and Drennan22 influenced them.10 As for Ibrahim’s study, the importance to Banting of not having to deal with trypsin in fetuses up to 4 months gestation is obvious. Carlson and Drennan had found that pregnant dogs undergoing pancreatectomies near term did not become diabetic and speculated: “the internal secretion of the fetal pancreas passes through the uterine membranes in sufficient quantity to prevent diabetes in the mother”22p393 However, it should be noted that this conclusion was highly tenuous as it was based on a small number of dogs and, since it had been performed in 1910 before blood glucose measurements were practical,23 only a few urine sugar measurements over 2–3 d. Banting and Best wrote: “The most natural interpretation of Carlson’s result is that the pancreas of the fetus furnishes to the mother an internal secretion which is necessary for the metabolism of sugar.”10p464 However, they cautiously noted that another investigator had been unable to replicate Carlson’s study.10
While Banting credits Laguesse in his Cameron Lecture, Banting and Best make no specific mention of him in their fetal calf pancreatic extract paper.10 Which Laguesse paper or papers did Best, whose French translations skills were poor but better than Banting’s, read (NB, Best famously mistranslated Paulesco’s paper that predated theirs and reported that his pancreatic extracts did not work6)? Laguesse had been highly prolific and had published on fetal human and ovine pancreatic histology in the 1890s (see below). Therefore, there was no need for Banting to speculate that “a partially developed foetus might contain even more abundant islet cells” than a newborn, as Laguesse had already shown this.
Nevertheless, while primary historical source material is limited, all sources agree that the second great idea was important. Famously, Macleod and Banting rarely agreed about anything, but Macleod, in his “History of the Researches Leading to the Discovery of Insulin,” considered this work an important step toward the discovery and fully credits Banting for this idea.14 Banting, on the other hand, never acknowledged the brilliance of Macleod’s idea to use teleost fish islet organs (NB, certain bony fish have anatomical separation of their endocrine and exocrine pancreata) as a source of insulin and as definitive proof that the islets were the source of insulin; while fetal calf islets were never used as a clinical source of insulin, insulin produced from Atlantic cod was used clinically at Toronto General Hospital (see below).24
Unfortunately, William R. Feasby’s account adds confusion by crediting Best for leading this work;15 no other source corroborates this version of the story. Feasby (1912–1970), the medical historian for the Canadian Army, started collecting information about the discovery of insulin for a book and a movie late in life. By that time, Banting was dead and so he interviewed Best extensively. Bliss was highly critical of Feasby’s historical research on the discovery of insulin and convincingly demonstrated that it was full of errors in his carefully researched but scathing paper “Rewriting medical history: Charles Best and the Banting and Best myth.”25 Feasby’s version is erroneous.
Reality Check: Does the Fetal Calf Pancreas Make Biological Sense Today?
As discussed above, Banting’s great idea played no essential role in the discovery of insulin. His second great idea appears to have been crucially important, but could it be wrong too? Banting described his fetal calf pancreas work as the transformative step in his and Best’s insulin research. But is the idea even biologically plausible – is it compatible with what we know today? Because of my 20 y interest in the history of insulin4,5,23,24,26 and my 30+ y career as a pediatric-perinatal pathologist clinician-scientist running an islet xenotransplantation laboratory,27–32 I decided to use the approaching 100th anniversary of the discovery of insulin as an excuse to address this perplexing, unanswered historical-biological question. In reading primary and secondary historical sources on Banting’s second great idea, it appears to have been based upon his and Best’s readings about both human and livestock fetal pancreata.
As a pediatric-perinatal pathologist who has performed over a thousand human fetal autopsies, it never made biological sense to me that fetal pancreas, while admittedly loaded with islets, contains much insulin. The term human fetal pancreas measures <5 cms in length, weighs ~ 4 grams, and contains about 6.1% to 12.9% immature islet tissue by volume (NB, the adult human pancreas measures 15–25 cm in length, weighs 100 gm, and is comprised of 1–2% mature islet tissue). Histochemical and immunohistochemical staining for insulin shows beta cells comprise only 40% of fetal islets; therefore, there is simply not much insulin in fetal pancreas.33,34 While current day ethical norms preclude the consideration of fetal human pancreas for islet transplantation, this was not always the case everywhere; older Australian and Swedish studies culturing human fetal pancreatic tissue consistently noted the low content of insulin-producing cells and focused on finding ways to facilitate beta cell differentiation in vitro; it required 2–6 months after xenotransplantation into diabetic nude or scid mice for the beta cell mass to expand to the point of maintaining normoglycemia in a mouse.35–40 While there is evidence that part of the initial poor function may be due to the lack of glucose-responsiveness in fetal beta cells,41 clearly fetal human islet data do not support great idea #2.
As an experimental islet xenotransplantation scientist, making highly potent extracts from fetal livestock pancreata also seemed implausible. The most popular large animal donor for islet xenotransplantation is the pig; since adult pig islets are difficult to isolate, both fetal and neonatal pig islets have been extensively studied as substitutes. Both are normally harvested by retrieving islet-rich fetal or neonatal pancreata and then chopping them into fragments for culture and transplantation. However, the literature is clear both are poorly differentiated and must grow and differentiate in tissue culture and after transplantation before they produce sufficient insulin to maintain normoglycemia in diabetic nude mice; in most studies this has required several months.42–44 A Swedish study transplanting neonatal porcine islet clusters into diabetic patients also confirmed the absence of significant immediate function.45,46 If fetal or neonatal pig islets contain so little insulin, it is biologically implausible that potent extracts could be made from these structures. Could species differences between fetal pig and fetal cow islets explain this seeming discrepancy?
While adult cows were initially considered as donors for islet xenotransplantation,47,48 this donor source was never aggressively pursued, likely because of concerns as to whether ruminant islets would function appropriately after transplantation into diabetic patients. I am unaware of any studies transplanting fetal or neonatal calf pancreata. There is one 30 y old Russian study on culturing fetal calf islets.49
In summary, using fetal islets as a source for insulin extraction intuitively seemed implausible but merited further historical/biological investigation. Laguesse had studied fetal ovine pancreas50 and Banting and Best used fetal bovine pancreas for their extractions. Could herbivore (sheep and cattle) fetal pancreata be fundamentally different than omnivore (human and porcine) fetal pancreata? What literature existed a hundred years ago and what exists now?
Laguesse and His Pancreatic Islet Research Opus
All versions of Banting’s second great idea begin with Laguesse (Figure 2). Unfortunately, there is little biographical literature on Gustave Edouard Laguesse (1861–1927).51,52 He was born and raised in Dijon, France. His father, a physician who did not practice medicine, was professor of botany at the Medical and Pharmaceutical School of Dijon and director of the botanical gardens. Edouard graduated in Paris as doctor of medicine in 1885 and doctor of science in 1890. Next he moved to Lille, where his earliest histological studies focused on the pancreatic islet organs in bony fish.24 He soon completed comprehensive histological studies on human and sheep pancreata.53–55 From 1896 to 1927, he was professor and head of the laboratory of histological research at Lille. Laguesse and Edouard Hédon (1863–1933), a physiologist at Montpellier who completed important two-stage pancreatectomy studies in dogs (NB, Macleod taught Banting the Hédon pancreatectomy method prior to departing for Scotland) contemporaneously with Laguesse’s histological studies in the 1890s, were awarded the Prix Albert I de Monico by the Academy of Medicine in Paris for their roles in the discovery of the internal secretion of the pancreas. Laguesse, who became increasingly interested in the high degree of vascularity of islets, developed the concept of secretion of a product into the “milieu intérieur” and also coined the term “endocrine secretion.” Laguesse was first to suggest that islets were endocrine structures.52
Figure 2.

Gustave Edouard Laguesse (1861–1927). https://en.wikipedia.org/wiki/%C3%89douard_Laguesse#/media/File:Professeur_Laguesse_CIPH0239.jpg
Victor Medvie (1905–2000), in his massive A History of Endocrinology, relates the following pertinent information about Laguesse and Paul Langerhans (1847–1888). In 1893, Laguesse, while studying ovine pancreatic histology, was somehow aware that Langerhans’ medical student dissertation from 1869 had previously described islands of pale-staining cells in the rabbit pancreas and charitably suggested the eponym islets of Langerhans. While Langerhans had not suggested any function for them (and had concluded in his dissertation that he had found nothing new and hoped his examiners would look tolerantly on his efforts), Laguesse was first to suspect they were endocrine in nature.56 Langerhans had described these as “Zellhaüchen” (little heaps of cells), which Laguesse translated as islands. Additional details about early islet histology and histopathology critical to the discovery of insulin have been reviewed in detail elsewhere.23
Following in Laguesse’s Footsteps
In 1896, Laguesse published important works on the histology of the fetal ovine pancreas and noted that fetal islets were increased in size and numbers and that a population of large islets developed first.50,55 In 1931, Max Aron (1892–1974) of Strasbourg, using fetal calf pancreas, described two distinct populations of islets, large and small, developing at different gestational ages. The primary generation (which he called ílots de Laguesse) could not be identified after birth, whereas the secondary generation (which he called ílots de Langerhans) functioned after birth.57 As noted by Susan Bonner-Weir and Arthur A. Like (1929–2013), who published a seminal study almost 50 y later, Aron’s observations were not believed because subsequent investigators using different species could not confirm the presence of dual islet populations. Bonner-Weir and Like studied bovine pancreata from early fetus (2 month gestation) to adult using histology, histocytochemistry, immunohisochemistry, morphometic analysis, and electron microscopy; they confirmed the presence of two distinct types of islets.58 Large islets, measuring up to 6 mm in diameter, were generally enmeshed in interlobular connective tissue and almost exclusively comprised of beta cells. While beta cells were poorly granulated at 2 months gestation, maximal granulation was achieved by three and a half months gestation and remained well-granulated at term (9 months gestation). On the other hand, small islets (<200um in diameter) were found scattered within acinar tissue and resembled other mammalian islets. They conclude that “the prominence and growth of the large islets during fetal life and their apparent subsequent cessation of growth after birth, suggest that the large islets are physiologically important in the fetus and neonate but may be a developmental vestige in the functional adult ruminant.”58p169 Other studies on fetal bovid pancreata or fetal ovine pancreata have reported similar large “perilobular giant islets.”59–61 While studies reported subtle differences, all confirm the existence of giant beta cell-rich perilobular islets in Banting and Best’s mid-trimester timeframe, and it appears that this population must be responsible for their highly potent fetal calf pancreas extracts. Merkwitz et al. reported that perilobular giant islets are absent in the pancreata of adult cattle, but that intralobular small islets are abundant.59 Therefore, we can surmise that the insulin Collip purified from adult cattle pancreata in January 1922, as well as the insulin that was mass-produced by pharmaceutical companies such as Eli Lilly for many decades afterward, was derived from intralobular small islets. As noted by Bonner-Weir and Like when discussing dual populations of islets, “cattle and sheep share two common characteristics: both are fructogenic as fetuses and ruminant as adults … pigs [which are not ruminants] do not have dual population of islets.”58p169 Unfortunately, a recent paper by Carlsson et al. directly comparing immunohistochemical staining for islet peptides and transcription factors in developing bovine and porcine islets was performed primarily in embryos rather than fetuses and so is noncontributory.62 Considering the animosity that existed within the team, it seems strangely appropriate that Banting, who physically attacked Collip during a heated laboratory confrontation in January 1922, and Collip, while using the same species, used two different islet populations to make their most potent insulin extracts. Collip, who was fortuitously on sabbatical in Toronto at the time of the discovery, was already a skilled biochemist.63
Biochemical studies also support the credibility of Banting’s second great idea. In 1934, Albert Madden Fisher and David Aylmer Scott (1892–1971) of the UofT Connaught Laboratories, using an ingenious hypoglycemic convulsion-based “mouse method of assay” (i.e., before the advent of radioimmunoassay), observed 18-fold higher insulin concentrations in fetal (under 5 months gestation) calf pancreas in international units per gram pancreas than in adult (9 y or older) bovine pancreas; when they tested fetal calf pancreata of 5–7 months gestation, the concentration was still 13-fold higher.64 It should be noted that these two distinguished chemists, along with Hans Christian Hagedorn (1888–1971) of Nordisk Laboratories in Denmark, later developed the longer-acting protamine-zinc insulin.65 Twenty-five years later, Willes et al., who measured insulin concentrations in acid-ethanol extracts of fetal ovine pancreatic tissue, found that the concentration (Units/g pancreas) increased throughout gestation and then declined sharply after birth; in fact, the mean insulin concentration was almost 7-fold lower in 2–6 y old adults than at one day after birth.61 D’Agostino et al. provided one final important piece of the puzzle when they extracted and quantified insulin in fetal bovine pancreas by radioimmunoassay. They found that the amount of immunoreactive insulin (IRI) in first trimester pancreata was slightly higher than in adult bovine pancreata on a per gram of tissue basis. However, IRI increased rapidly with gestational age and, by the third trimester, was 7-fold higher than in the adult. They noted: “When pancreatic IRI concentrations were standardized for protein content of the extracts, a decrease was noted between the midsecond and third trimesters. This is most likely the result of dilution of the endocrine portion of the pancreas by the rapidly growing exocrine pancreas.”66p1108 By a combination of good luck and good planning, Banting and Best hit just the right timeframe (early second trimester) for fetal calf pancreata.
There is one final twist. While Banting credited Laguesse for sparking his idea of using fetal calf pancreas, he never provided any details related to this claim and, in fact, he may not have been entirely aware of the idea’s origin. Leonid V. Sobolov (1876–1919), a Russian pathologist who trained under physiologist Ivan P. Pavlov (1849–1936) and pathologist Konstantin Nikolaevich Vinogradov (1847-????), had a career-long interest in the islets of Langerhans. Almost 20 y before Banting’s first great idea tweaked, Sobolov, while studying the pathology of experimental pancreatic duct-ligation, suggested making extracts from both duct-ligated pancreas and newborn calf pancreas in his doctoral thesis (1901).67,68 While the thesis was published in Russian and was not easily accessible, an abridged version was published in German in 1902, and Sobolov’s ideas were well-known in the early 20th century. Although Banting did not enjoy reading the literature, he may also have stumbled across Sobolov’s work. Regardless, Banting’s ideas about making extracts from calf islets would have been derived at least indirectly from Laguesse, as this was likely the origin of Sobolov’s idea.
Macleod’s Closely Related Great Idea
Banting’s preoccupation with his first great idea led to his second great idea; both focused on the desirability of extracting the internal secretion from pancreatic tissue depleted of or mostly devoid of exocrine pancreatic tissue. However, Banting never recognized the brilliance of JJR Macleod’s ultimate extension of this idea. Macleod was aware that certain teleost (bony) fish have anatomical separation of their endocrine and exocrine pancreata. In 1922 while Banting was busy maligning his research supervisor in Toronto,1,2,5 Macleod spent his summer at the Atlantic Biological Station in St. Andrew’s, New Brunswick making extracts from monkfish and sculpin islets as well as their exocrine pancreas. He showed definitively that islet extracts, but not exocrine pancreas extracts, contained insulin,69 which impressed the Nobel Prize Committee;24 so it was Macleod, not Banting who provided the definitive proof that the pancreatic islets were the source of insulin (NB, Banting and Best’s crude extracts and Collip’s purified extracts were never derived from pure islet tissue). Macleod chose sculpins and monkfish because they were known to possess a large “principal islet” (sometimes measuring greater than 5 mm in diameter) and then one or more smaller, but still macroscopically visible, islets; this characteristic also allowed him to perform isletectomy experiments.24 Over the next 2 y, Macleod and two of his graduate students, Noble and Norman A. McCormick (1901–1967), studied islets in many Atlantic Ocean fish species as well as the logistics of commercial production of insulin from fish; in fact, during early insulin shortages, diabetic patients in Toronto were unknowingly treated with fish insulin.4,24 It is now known that most teleost fish possess a few large and many smaller islets, and that the timing of development of these is dissimilar to the two distinct islet populations in fetal calves and lambs. Prototypically, fish larvae initially develop a single islet which is followed by subsequent continuous development of newer islets, all of which grow continuously throughout the lifespan of the fish.70–73 Larger teleost fish islets are simply older than smaller islets, which, unlike the large fetal islets in ruminants, do not disappear in adulthood. Teleost fish islets are often called Brockmann bodies and are named after German physician Heinrich Adolph Christian Brockmann (1820–1858) who described these structures in his doctoral thesis De Pancreate Piscium in 1846.
Medical History Based Upon Biological Plausibility
Most medical history research focuses on examination of historical figures and events; sequences of events are important for determining priority of discoveries. Clearly, the viewpoints of contemporaries are important in assessing the importance and meaning of such events. Historians collect available and relevant data on a figure or event, sift through it to determine what seems credible, analyze this in the context of its totality, and then develop a narrative that best fits the credible historical data. This current historical analysis of an important medical discovery highlights that, in some instances, historical research should also be able to stand up to biological plausibility testing as well as peer-review by both biological and historical content experts.
In honor of the 100th anniversary of the discovery of insulin, this paper adds a new biological dimension to its medical history. I critically examined part of the story that all contemporaries agree was a crucial step but that has been largely ignored by historians. As a medical historian with content expertise in islet ontogeny and physiology, I have dissected the part of this story that initially seemed biologically implausible (making a highly potent insulin from fetal pancreas) and, by using historical and more contemporary scientific literature, have shown it to be highly credible. Clearly, Banting’s second great idea was much better than his first! However, while addressing an important historical issue, this paper raises a new biological question. Why do islets from ruminant species produce/secrete so much insulin, as compared to other mammalian species, during fetal life?
Acknowledgments
The author thanks Kristin Rodgers, MLIS, The Ohio State University Medical Heritage Center; the University of Calgary Interlibrary Loan service, Thomas Kryton BFA, and Charlotte Monroe.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Bliss M. The Discovery of Insulin. Chicago: The University of Chicago Press; 1982. [Google Scholar]
- 2.Bliss M. Banting: a biography. University of Toronto Press; 1992. [Google Scholar]
- 3.Bliss M The discovery of insulin at the University of Toronto. The International Research Symposium on Diabetes held at the University of Toronto and the Toronto General Hospital, 6-9 October 1996, Toronto: Thomas Fisher Rare Book Library; 1996. [Google Scholar]
- 4.Wright JR Jr. Almost famous: E. Clark Noble, the common thread in the discovery of insulin and vinblastine. CMAJ. 2002. Dec 10;167(12):1391–1396. [PMC free article] [PubMed] [Google Scholar]
- 5.Wright JR Jr, Gale EAM. Winner’s curse: the sad aftermath of the discovery of insulin. Diabetic Med. 2021; 00:e14677. 10.1111/dme.14677 [DOI] [PubMed] [Google Scholar]
- 6.Banting FG, Best CH. The internal secretion of the pancreas. J Lab Clin Med. 1922. Feb;7(5):251–267. [Google Scholar]
- 7.Roberts F. Insulin. Br Med J. 1922;2:1193–1194. [Google Scholar]
- 8.Pratt JH. On the history of the discovery of insulin. In: von Engelhardt D, editor. Diabetes Its Medical and Cultural History. Berlin, Germany: Springer-Verlag; 1989. p. 411–419. Reprinted from Sudhoff's Archiv. 1954;38:48–57. [Google Scholar]
- 9.Banting FG. The history of insulin (Cameron Lecture). Edinb Med J. 1929;36:1–18. [Google Scholar]
- 10.Banting FG, Best CH. Pancreatic extracts. J Lab Clin Med. 1922. May;7(8):464–472. [PubMed] [Google Scholar]
- 11.Stevenson L. Sir Frederick Banting. Toronto [Canada]: The Ryerson Press; 1946. [Google Scholar]
- 12.Harris S. Banting’s miracle: the story of the discoverer of insulin. Toronto: JM Dent & Sons (Canada) Ltd; 1946. [Google Scholar]
- 13.Wrenshall GA, Hetenyi G, Feasby WR. The story of insulin: forty years of success against diabetes. Bloomington, IN: Indiana University Press; 1962. [Google Scholar]
- 14.Macleod JJR. History of the researches leading to the discovery of insulin: with an introduction by Lloyd G. Stevenson. Bull Hist Med. 1978 Fall;52(3):295–312. [PubMed] [Google Scholar]
- 15.Feasby WR. The discovery of insulin. Bull Med Libr Assoc. 1960;48(1):11–20. [PMC free article] [PubMed] [Google Scholar]
- 16.Best HBM. Margaret and Charley: the personal story of Dr. Charles Best, the co-discoverer of insulin. Toronto, Canada: Dundurn; 2003. [Google Scholar]
- 17.Levine IE. The discoverer of insulin. Vancouver,Canada: Copp Clark Publishing Co.; 1959. [Google Scholar]
- 18.Roland J. The insulin man: the story of Sir Frederick Banting. London, UK: Lutterworth Press; 1965. [Google Scholar]
- 19.Bankston J. Frederick Banting and the Discovery of Insulin (Unlocking the Secrets of Science series). Bear [DE]: Mitchell Lane Publishers; 1974. [Google Scholar]
- 20.Bliss M, Davies W. Dictionary of Canadian Biography. Vol. 15. University of Toronto/Université Laval:2003. Available from: http://www.biographi.ca/en/bio/davies_william_15E.html. Accessed April 24, 2021 [Google Scholar]
- 21.Ibrahim J. Trypsinogen und Enterokinase beim menschlichen neugeborenen und Embryo. Biochem Ztschr. 1909;22:24–32. [Google Scholar]
- 22.Carlson AJ, Drennan FM. The control of pancreatic diabetes in pregnancy by the passage of the internal secretion of the pancreas of the fetus to the blood of the mother. Am J Physiol. 1911;28:391–395. [Google Scholar]
- 23.Wright JR Jr. Essential contributions of pathologists and laboratory physicians leading to the discovery of insulin. Arch Pathol Lab Med. 2020;144(7):894–904. [DOI] [PubMed] [Google Scholar]
- 24.Wright JR Jr. From ugly fish to conquer death: J J R Macleod’s fish insulin research, 1922-24. Lancet. 2002. Apr 6;359(9313):1238–1242. [DOI] [PubMed] [Google Scholar]
- 25.Bliss M. Rewriting medical history: Charles Best and the Banting and Best myth. J Hist Med Allied Sci. 1993;48:253–274. [DOI] [PubMed] [Google Scholar]
- 26.Wright JR Jr, McIntyre L. Misread and mistaken: Étienne Lancereaux’s enduring legacy in the classification of diabetes mellitus. J Med Biogr. https://journals.sagepub.com/doi/10.1177/0967772020914797. [DOI] [PubMed] [Google Scholar]
- 27.Wright JR Jr, Polvi S, MacLean H. Experimental transplantation with principal islets of teleost fish (Brockmann bodies): long-term function of tilapia islet tissue in diabetic nude mice. Diabetes. 1992;41(12):1528–1532. [DOI] [PubMed] [Google Scholar]
- 28.Yang H, Dickson B, O’Hali W, Kearns H, Wright JR Jr.. Functional comparison of mouse, rat, and fish islet grafts transplanted into diabetic nude mice. Gen Comp Endocrinol. 1997;106(3):384–388. [DOI] [PubMed] [Google Scholar]
- 29.Wright JR Jr, Pohajdak B. Cell therapy for diabetes using piscine islet tissue. Cell Transplant. 2001;10(2):125–143. [PubMed] [Google Scholar]
- 30.Xu BY, Yu Y, Al Abdullah I, Kandeel F, Hering B, Wright JR Jr.. Long-term survival and function of intraportal porcine and human islets xenografts in non-diabetic nude mice. Transplant Proc. 2008;40(2):584–586. [DOI] [PubMed] [Google Scholar]
- 31.Wright JR Jr, Yang H, Hyrtsenko O, Xu B-Y, Yu W, Pohajdak B. A review of piscine islet xenotransplantation using wild-type tilapia donors and the production of transgenic tilapia expressing a “humanized” tilapia insulin. Xenotransplant. 2014;21(6):485–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hrytsenko O, Pohajdak B, Wright JR Jr. Ancestral genomic duplication of the insulin gene in tilapia: an analysis of possible implications for clinical islet xenotransplantation using donor islets from transgenic tilapia expressing an humanized insulin gene. Islets. 2016. Jul 3;8(4):e1187352. doi: 10.1080/19382014.2016.1187352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jaffe R, Hashida Y, Yunis EJ. The endocrine pancreas of the neonate and infant. Perspect Pediatr Pathol. 1982;7:137-165. [PubMed] [Google Scholar]
- 34.Ruchelli E. Pancreas. In: Ernst LM, Ruchelli E, Huff DS, editors. Color atlas of fetal and neonatal histology. New York: Springer. 2011. [Google Scholar]
- 35.Tuch BE, Jones A, Turtle JR. Maturation response of human fetal pancreatic explants to glucose. Diabetologia. 1985;28:28–31. [DOI] [PubMed] [Google Scholar]
- 36.Si Z, Tuch BE, Walsh DA. Development of human fetal pancreas after transplantation into SCID mice. Cells Tissues Organs. 2001;168:147–157. [DOI] [PubMed] [Google Scholar]
- 37.Sandler S, Andersson A, Schnell A, Mellgren A, Tollemar J, Borg H, Petersson B, Groth CG, Hellerström C. Tissue culture of human fetal pancreas. Development and function of B-cells in vitro and transplantation of explants to nude mice. Diabetes. 1985;34(11):1113–1119. [DOI] [PubMed] [Google Scholar]
- 38.Sandler S, Andersson A, Landström AS, Tollemar J, Borg H, Petersson B, Groth CG, Hellerström C. Tissue culture of human fetal pancreas. Effects of human serum on development and endocrine function of isletlike cell clusters. Diabetes. 1987; 36(12): 1401–1407. [DOI] [PubMed] [Google Scholar]
- 39.Otonkoski T, Knip M, Panula P, Andersson S, Wong I, Goldman H, Simell O. Morphology, yield and functional integrity of islet-like cell clusters in tissue culture of human fetal pancreata obtained after different means of abortion. Acta Endocrinol (Copenh). 1988. May; 118(1): 68–76. [DOI] [PubMed] [Google Scholar]
- 40.Sandler S, Andersson A, Korsgren O, Tollemar J, Petersson B, Groth CG, Hellerström C. Tissue culture of human fetal pancreas. Effects of nicotinamide on insulin production and formation of isletlike cell clusters. Diabetes. 1989. Jan;38(1):168–171. [DOI] [PubMed] [Google Scholar]
- 41.Bonner-Weir S, Aguayo-Mazzucato C, Weir GC. Dynamic development of the pancreas from birth to adulthood. Upsala J Med Sci. 2016;121(2):155–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Korsgren O, Sandler O, Schnell-Landström A, Jansson L, Andersson A. Large-scale production of fetal porcine pancreatic islet like cell clusters. Transplantation. 1988;45:509–514. [DOI] [PubMed] [Google Scholar]
- 43.Korsgren O, Jansson L, Eizirik D, Andersson A. Functional and morphological differentiation of fetal porcine islet-like cell clusters after transplantation into nude mice. Diabetologia. 1991;34:379–386. [DOI] [PubMed] [Google Scholar]
- 44.Korbutt GS, Elliot JF, Ao Z, Smith DK, Warnock GL, Rajotte RV. Large scale isolation, growth, and function of porcine neonatal islet cells. J Clin Invest. 1996;97:2119–2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Groth CG, Andersson A, Korsgren O, Tibell A, Tollemar J, Kumagai-Braesch M, Möller E, Bolinder J, Ostman J, Bjöersdorff A, et al. Transplantation of porcine fetal islet-like cell clusters into eight diabetic patients. Transplant Proc. 1993. Feb;25(1 Pt 2), 970. [PubMed] [Google Scholar]
- 46.Groth CG, Korsgren O, Tibell A, Tollemar J, Möller E, Bolinder J, Ostman J, Reinholt FP, Hellerström C, Andersson A. Transplantation of porcine fetal pancreas to diabetic patients. Lancet. 1994. Nov 19;344(8934):1402–1404. [DOI] [PubMed] [Google Scholar]
- 47.Hering BJ, Romann D, Clarius A, Brendel M, Slijepcevic M, Bretzel RG, Federlin K. Bovine islets of Langerhans. Potential source for transplantation? Diabetes. 1989. Jan;38(1):206–208. [DOI] [PubMed] [Google Scholar]
- 48.Marchetti P, Giannarelli R, Cosimi S, Masiello P, Coppelli A, Viacava P, Navalesi R. Massive isolation, morphological and functional characterization, and xenotransplantation of bovine pancreatic islets. Diabetes. 1995Apr, 44(4), 375–381. [DOI] [PubMed] [Google Scholar]
- 49.Ablamunits VG, Kirsanova LA. [In vitro phenomenon of beta cell migration from fetal calf pseudoislets]. Biull Eksp Biol Med. 1992. Jun;113(6):658–660. [PubMed] [Google Scholar]
- 50.Laguesse E. Récherches sur l’histogénie du pancréas chez le mouton, III Origine et évolution des îlots de Langerhans (pseudo-follicules). J Anat Physiol. 1896;32:209–255. [Google Scholar]
- 51.Hoet JP. Gustave Edouard Laguesse: his demonstration of the significance of the islands of Langerhans. Diabetes. 1953. Jul;2(4):322–324. [DOI] [PubMed] [Google Scholar]
- 52.Fossati P. Edouard. Laguesse à Lille en 1893 crée le terme “endocrine” et ouvre l’ère de l’endocrinologie Son modèle: l’îlot endocrine du pancréas et le diabèt. Hist Sci Med. 2004;38(4):433–439. [PubMed] [Google Scholar]
- 53.Laguesse E. Sur la formation des ilots de Langerhans dans le pancreas. Comptes Rend Soc Biol. 1893;5:819–820. [Google Scholar]
- 54.Laguesse E. Recherches sur l’histogenie du pancréas chez le mouton. J Anat Physiol. 1895;31:475–500. [Google Scholar]
- 55.Laguesse E. Recherches sur l’histogénie du pancréas chez le mouton. Paris: Alcan; 1896. [Google Scholar]
- 56.Medvei VC. A History of Endocrinology. Lancaster (UK): MTP Press; 1982. [Google Scholar]
- 57.Aron M. Evolution du pancréas endocrine. Bull Biol. 1931;65:441–463. [Google Scholar]
- 58.Bonner-Weir S, Like AA. A dual populations of islets of Langerhans in bovine pancreas. Cell Tissue Res. 1980;206:157–170. [DOI] [PubMed] [Google Scholar]
- 59.Merkowitz C, Lochhead P, Böttger J, Matz Soja M, Sakurai M, Gebhardt R, Ricken AM. Dual origin, development, and fate of bovine pancreatic islets. J Anat. 2013. Mar;222(3):358–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gupta D, Uppal V, Bansal N, Gupta A. Differentiation of pancreatic endocrine islets in buffalo fetus. Indian J Animal Sci. 2020;90:693–697. [Google Scholar]
- 61.Willes RF, Boda M, Stokes H. Cytological localization of insulin and insulin concentration in the fetal ovine pancreas. Endocrinol. 1969;84:671–675. [DOI] [PubMed] [Google Scholar]
- 62.Carlsson GL, Scott Heller R, Serup P, Hyttel P. Immunohistochemistry of pancreatic development in cattle and pig. Anat Histol Embryol. 2010;39:107–119. [DOI] [PubMed] [Google Scholar]
- 63.Li A. J.B. Collip and the Development of Medical Research in Canada. Montreal & Kingston: McGill-Queens University Press; 2003. [Google Scholar]
- 64.Fisher AM, Scott DA. The insulin content of the pancreas in cattle of various ages. J Biol Chem. 1934;106:305–310. [Google Scholar]
- 65.Rutty CJ From insulin to heparin: innovation at Connaught Labs during the 1930s. Available from: https://connaught.research.utoronto.ca/history/article5/ Accessed May 2, 2021.
- 66.D’Agostino J, Field JB, Frazier ML. Ontogeny of immunoreactive insulin in the fetal bovine pancreas. Endocrinol. 1985;116:1108–1116. [DOI] [PubMed] [Google Scholar]
- 67.Van Beck C, Leonid V. Sobolev 1876-1919. Diabetes. 1958;7(3):245–248. [DOI] [PubMed] [Google Scholar]
- 68.Tattersall R. The pissing evil: a comprehensive history of diabetes mellitus. Ayrshire, UK: Swan & Horn; 2017. [Google Scholar]
- 69.Macleod JJR. The source of insulin: a study of the effect produced on blood sugar by extracts of the pancreas and principal islets of fishes. J Metab Res. 1922;2:149–172. [Google Scholar]
- 70.Morrison CM, Miyake T, Wright JR Jr.. Histological study of the development of embryo and early larva of Oreochromis niloticus (Pisces: cichlidae). J Morphol.FF 2001;247(2):172–195. [DOI] [PubMed] [Google Scholar]
- 71.Morrison CM, Pohajdak B, Tam J, Wright JR Jr.. Development of the islets, exocrine pancreas and related ducts in the Nile tilapia, Oreochromis niloticus (Pisces: cichlidae). J Morphol. 2004;261(3):377–389. [DOI] [PubMed] [Google Scholar]
- 72.Yang H, Morrison CM, Conlon JM, Laybolt K, Wright JR Jr.. Immunocytochemical characterization of the pancreatic islet cells of the tilapia (Oreochromis niloticus). Gen Comp Endocrinol. 1999;114(1):47–56. [DOI] [PubMed] [Google Scholar]
- 73.Morrison CM, Fitzsimmons K, Wright JR Jr.. Atlas of tilapia histology. Baton Rouge, LA: World Aquaculture Society; 2006. [Google Scholar]


