Figure 1.
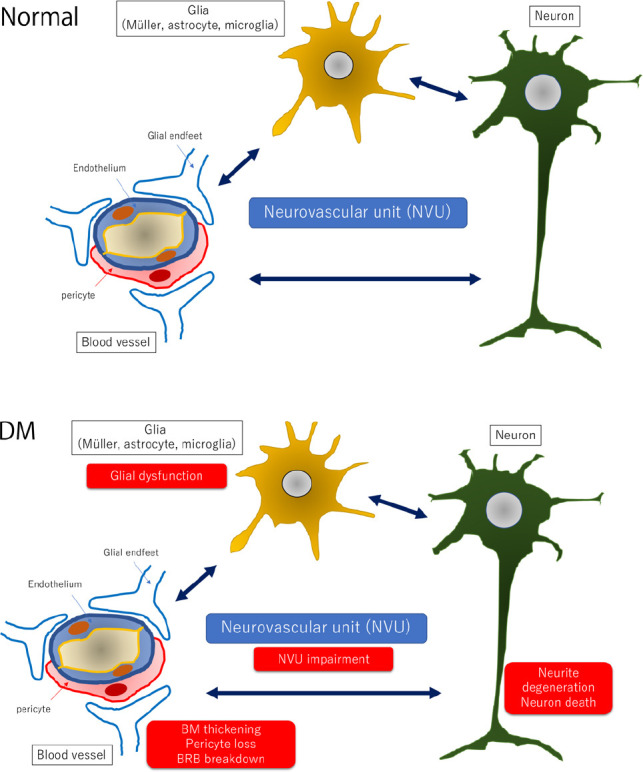
Hypothetic schemes of neurovascular units and pathological changes of the diabetic retina.
In the normal retina (upper panel), the neurovascular units are composed of vascular cells (pericyte and endothelial cell), glial cells (Müller cell, microglia and astrocyte), and neurons. Vascular cells and glial processes form the BRB, and pericytes are considered to maintain the function of retinal cells by maintaining the appropriate environment because the loss of platelet-derived growth factor signaling in pericytes causes a breakdown of the BRB and neuronal cell death. Glial cells including microglia may monitor the changes in the vessels and the condition of the retina and transfer the changes into neuronal cells. In the diabetic retina (lower panel), glial dysfunction may occur first by an increase expression of glial fibrillary acidic protein in Müller cells and reduction of glial fibrillary acidic protein expression in astrocytes. Activated glial cells are partly associated with an increase of cytokines such as tumor necrosis factor-α, interleukin-1β, interleukin-6, interleukin-8, monocyte chemoattractant protein-1, and vascular endothelial growth factor and a decrease of growth factors such as nerve growth factor, brain-derived growth factor, and pigment epithelium-derived growth factor. These glial changes contribute to neuronal abnormalities including neuronal cell death and neurite degeneration. Pericytes are affected faster than endothelial cells and increase the expression of extracellular matrix components, partly contributing to BRB breakdown. BM: Basement membrane; BRB: blood-retinal barrier; DM: diabetes mellitus.
