Figure 1:
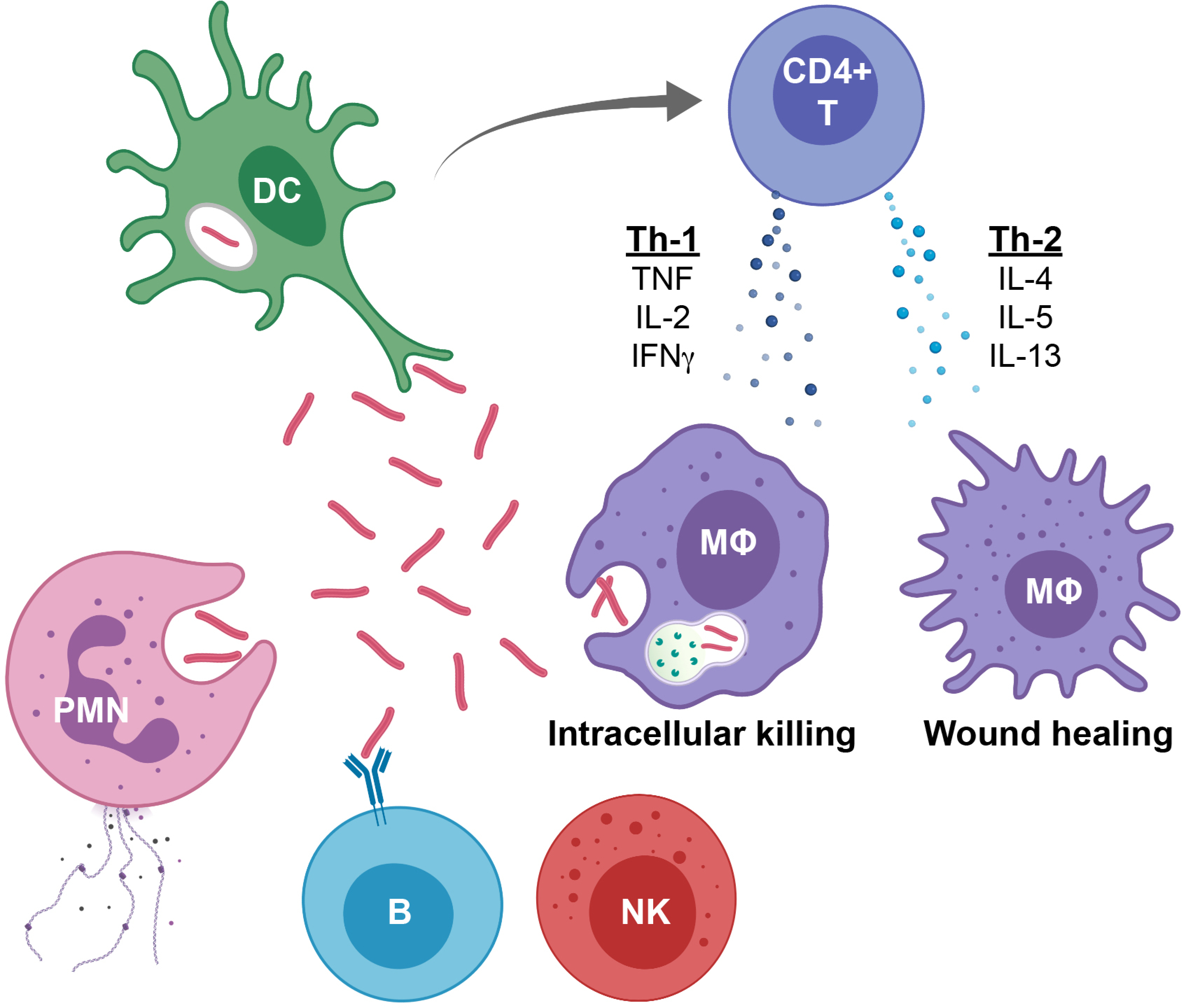
Overview of immune response to Mtb infection
1. Dendritic cells (DCs), polymorphonuclear neutrophils (PMNs), and macrophages phagocytose Mtb leading to either mycobacterial survival or death.
2. DCs are professional antigen presenting cells and bring Mtb antigens to the draining lymph node, where DCsimplement antigen presentation and activation the classic CD4+ T cell response.
3. Macrophages are the preferred intracellular niche for Mtb. When activated by TNF and IFN-γ, they upregulate ROS, lysosomal acidification and phagolysosome maturation and increase Mtb killing capacity (More M1-like macrophage). When activated by IL-10, IL-4, IL-5 or IL-13, they down-regulate these processes, temper intracellular killing and focus on wound healing (More M2-like macrophage). Tissue macrophages represent a spectrum that typically includes elements of both M1 and M2 phenotypic characteristics.
4. Neutrophils, phagocytose and kill Mtb, but also produce cytokines and when they die, they spew out an extracellular matrix of chromatin and proteins that alert other immune cells.
5. CD4+ T cells produce cytokines, such as Th-1 cytokines TNF, IL-2 and IFN-γ that stimulate macrophages for intracellular killing, or Th2 cytokines IL-4, IL-5 and IL-13 that promote macrophage wound healing.
6. Cytotoxic T cells, as well as Natural Killer (NK) cells, MAIT (mucosal associated invariant T cells) and Innate LymphoidCells (ILCs), in addition to producing activating or suppressive cytokines, can induce perforin and granzyme-mediate cytotoxic killing of Mtb-infected cells.
7. B cells produce antibodies that neutralize extracellular Mtb, mediate NK CD16 antibody dependent cytotoxicity, and mark Mtb for opsonophagocytic clearance.
