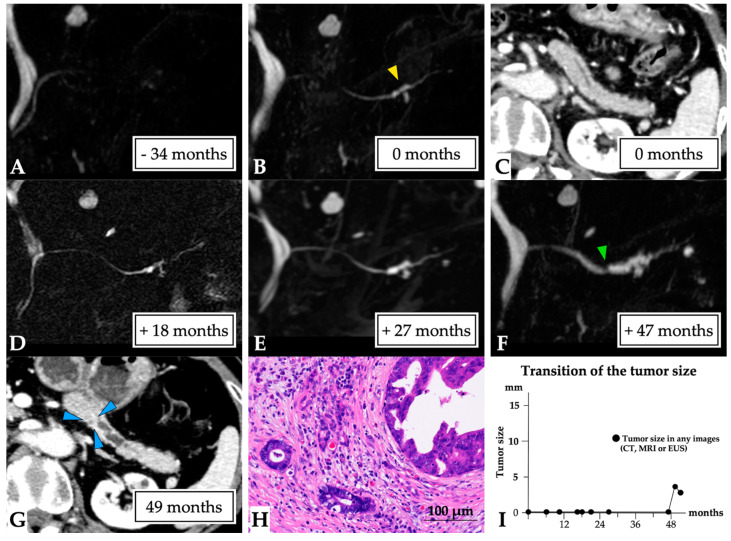
Figure 4.
A 3 mm lesion over a 50-month observation period (Case 4 in Supplementary Table S1). The case of a 73-year-old woman who had a history of idiopathic acute pancreatitis at 4 years prior is presented. No MPD abnormalities were observed on MRCP (A); however, solitary MPD and branch pancreatic duct dilation were evident in the pancreatic tail (yellow arrow head, first-time MRCP, (B)), although no tumor lesions were detected on CT (C). The MPD abnormality gradually progressed (D,E), and MPD stenosis was detected at the beginning of solitary MPD dilation after 47 months (green arrow head, (F)). No tumor lesion was observed on CT or EUS images. ERCP detected localized irregular stenosis with suspected malignancy by pancreatic juice cytology findings. In addition, a tiny lesion was detected on CT after 49 months (blue arrow head, (G)). Therefore, surgery was undertaken after 50 months for a suspected small PC. The final diagnosis was the presence of a 3 mm invasive PC in the pancreatic tail (T1 N0 M0, stage IA, final tumor size: 3 mm, (H)). This patient was diagnosed at 50 months after the first MRCP (I). Abbreviations: EUS, endoscopic ultrasound; CT, computed tomography; IPMN, intraductal papillary mucinous neoplasm; MPD, main pancreatic duct; MRCP, magnetic resonance cholangiopancreatography; MRI, magnetic resonance imaging; PC, pancreatic cancer.