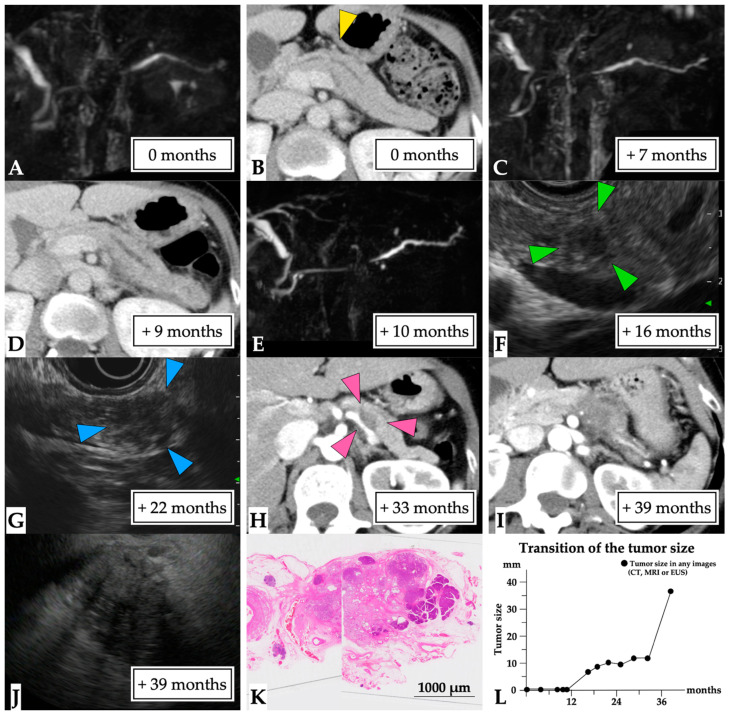
Figure 6.
A 36 mm lesion over a 39-month observation period (Case 9 in Supplementary Table S1). A 49-year-old woman presented with idiopathic acute pancreatitis and underwent MRCP, which showed slight MPD stenosis accompanied by distal MPD dilation (first-time MRCP, (A)). CE-CT scans detected a partial MPD stenosis without tumor lesion or pancreatic stone (yellow arrow head, (B)), and the patient was diagnosed with chronic pancreatitis. Subsequently, a recurrent attack of pancreatitis occurred, and MPD stenosis and distal MPD dilation were clearly observed on MRCP and CT findings (C–E). An EUS scan performed after 16 months detected a 7 mm diameter tumor (green arrow head, (F)). However, EUS-FNA could not be performed because the endoscopist failed to recognize the tumor lesion. Therefore, ERCP was performed to determine a diagnosis of malignancy after 19 months. However, pancreatic juice cytology findings did not indicate malignancy. Subsequently, the tumor lesion was observed to have gradually progressed on EUS (blue arrow head, (G)) and CT (pink arrow head, (H)) images. This patient was referred to our hospital after 39 months following clear detection of the tumor (I). EUS-FNA was performed on the 36 mm diameter tumor (J), and the pathological diagnosis was adenocarcinoma (final tumor size, 36 mm). Therefore, distal pancreatectomy was performed for PC after NAC. The final diagnosis was the presence of a 30 mm invasive nodule in the pancreatic body (T3 N1 M0, stage IIB, (K)). This patient was diagnosed at 39 months after the first MRCP (L). Abbreviations: EUS, endoscopic ultrasound; CE-CT; contrast-enhanced computed tomography; CT, computed tomography; FNA, fine needle aspiration; IPMN, intraductal papillary mucinous neoplasm; MPD, main pancreatic duct; MRCP, magnetic resonance cholangiopancreatography; NAC, neoadjuvant chemotherapy; PC, pancreatic cancer.