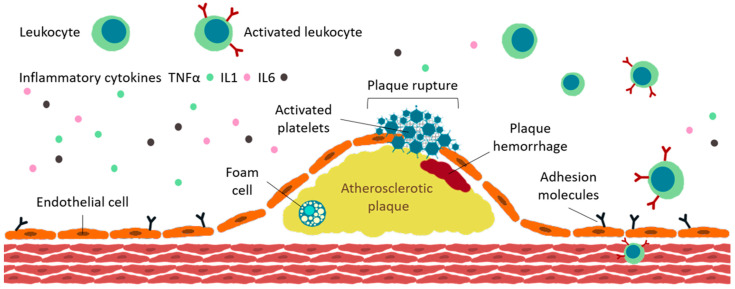
Figure 3.
Atherosclerosis (ATS) plaque formation. Immune system is implicated through various mechanisms in atherogenesis; the presence of immune cells (such as TNFα, IL-1, and IL-6) in atherosclerotic plaques proves this concept. Vascular endothelium is involved in regulation of physiological processes taking place in the vessel. The first step in the development of atherosclerosis is the accumulation of low-density lipoproteins (LDLs) and leukocytes into the sub-endothelium. LDLs are modified and become aggregated and/or oxidized. The monocytes present in the sub-endothelium layer differentiate to macrophages, which will engulf Ox-LDL, thus determine the accumulation of cholesterol in macrophages and formation of foam cells, which will lead to increased secretion of cytokine and chemokine and further recruitment of circulating immune cells. High levels of endothelial adhesion molecules, such as vascular cell adhesion molecule-1 (VCAM-1), monocyte chemoattractant protein-1 (MCP-1), and intracellular adhesion molecule-1 (ICAM-1) are identified. Apoptosis and necrosis are stimulated by high levels of cholesterol in foam cells and, after cellular death, cholesterol esters will accumulate and produce atherosclerotic plaque. The most frequent cause of thrombosis is plaque instability and then fracture. Once the fibrous cap is ruptured, the substances from the plaque are released and put in contact with blood; this may cause obstruction of blood flow and, in the end, the specific symptoms of thrombosis. TNF, tumor necrosis factor; IL, interleukin (after [130]).