Abstract
Objective
To describe the impact of social determinants on the experience of the coronavirus disease 2019 (COVID-19) pandemic within the pediatric population, how this impact may influence the long-term health and security of children, and what measures can be taken to ameliorate this impact moving forward.
Data Sources
Nonsystematic review of relevant literature and news sources.
Study Selections
Relevant literature and news sources.
Results
There have been increases in housing insecurity and food insecurity during the pandemic, including global increases in poverty. Public policies such as school closures have had a disproportionate impact on those facing adverse social determinants. There has been a dramatic increase in reports of abuse-related injuries and other injuries indicative of child abuse during the pandemic. In addition, there are disproportionate impacts of COVID-19 based on race and ethnicity within the United States. It is clear that children are facing more adverse determinants as a result of this pandemic and that there are both short-term and long-term implications associated. For those living in poverty or with other adverse social determinants of health, the pandemic has made a bad situation worse. Ongoing studies are required to measure the impact of COVID-19 on those with adverse social determinants, in particular among children.
Conclusion
Social determinants of health must be part of pandemic research priorities, public health and vaccination goals, and economic policy implementation. The impact of the COVID-19 pandemic has further served to shed a light on the broad disparities that exist within our society and their direct and indirect impacts on health outcomes.
Key Messages.
-
•
Social determinants of health have helped contribute to the detrimental impact of coronavirus disease 2019 (COVID-19) on pediatric health, apart from direct disease manifestations.
-
•
COVID-19 has affected Black communities disproportionately, including higher infection and fatality rates and lower vaccination rates.
-
•
Households experiencing homelessness and housing insecurity as a result of the pandemic were associated with increased COVID-19–related morbidity and morbidity, secondary to reduced access to public health measures to reduce disease transmission.
-
•
Food insecurity among children has risen dramatically as a result of the pandemic, influenced in part by reduced access to school lunches, fragility in the food supply chain, rising food costs, and risks of unemployment.
-
•
Rates of extreme poverty (living on <$1.90 per day) are anticipated to rise for the first time in 20 years. Poverty is a negative influence on child health, in particular long-term conditions and mental health.
-
•
Domestic violence, including child abuse and intimate partner violence, has increased during the pandemic, both of which are associated with long-term adverse health outcomes in children.
Alt-text: Unlabelled box
Introduction
As of mid-October 2021, the novel severe acute respiratory syndrome coronavirus 2 (coronavirus disease 2019 [COVID-19]) has affected more than 129 million individuals internationally with more than 4.86 million deaths.1 Within the United States, there are more than 45 million cases and more than 726,000 deaths, the largest number in any country in the world.1
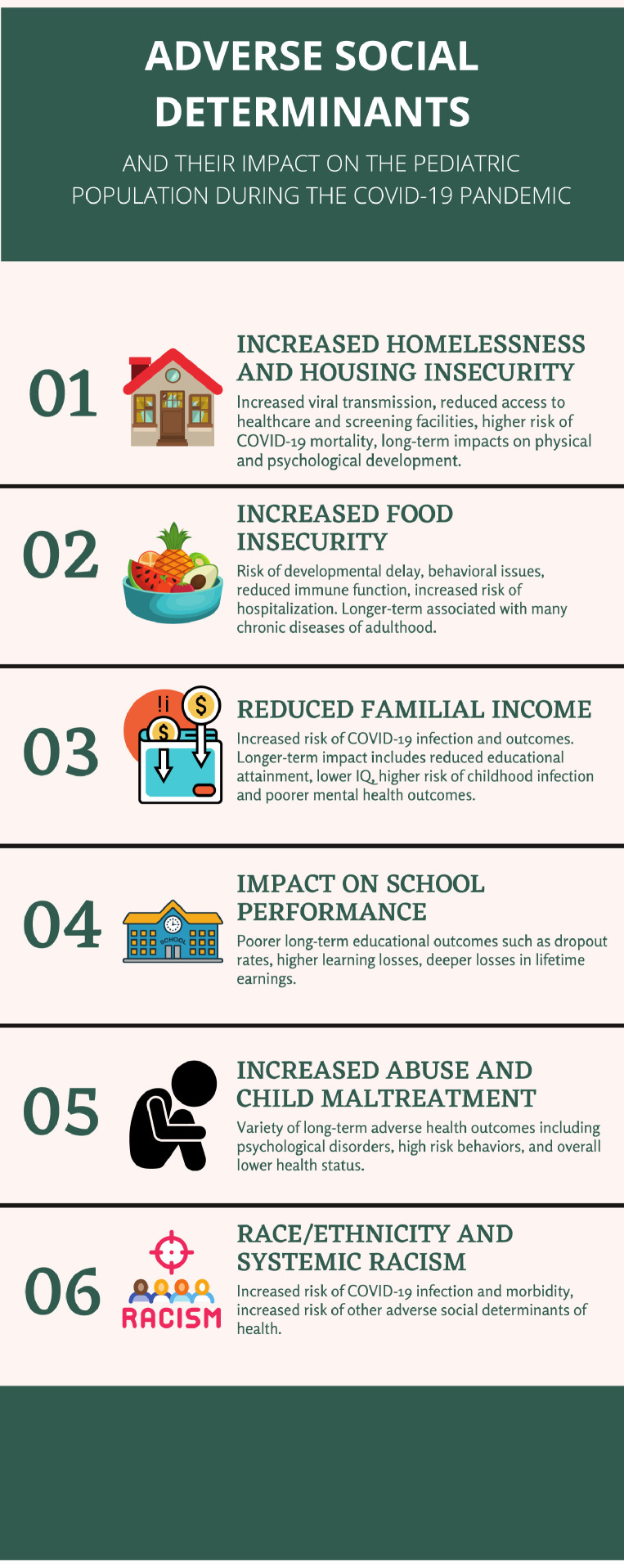
The World Health Organization defines social determinants of health as “the conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels.”2 Many of these social determinants, including housing security, food security, income, education, and race, have been affected significantly by the COVID-19 pandemic.1 Although much has been described on the overall impact of COVID-19 on adverse determinants, little has focused specifically on children. As a result, the focus of this narrative review is to describe the impact of social determinants on the experience of the COVID-19 pandemic within the pediatric population, how this impact may influence the long-term health and security of children, and what measures can be taken to ameliorate this impact moving forward. This review aims to emphasize the impact of the pandemic on already existing social disparities that affect our patients, without emphasizing any disease-specific effects. Although these disparities are not allergy specific, they speak to the broader principle that adverse social determinants have a profound impact on the global health of our patients and are a necessary factor to consider as a “component of the physician's role as an advocate for patients and a steward of medical care.”3 Figure 1 details key health disparities discussed in this review.
Figure 1.
Adverse social determinants of health and the impact on children and families during the COVID-19 pandemic. Summary of 6 major social determinants of health that have affected the lives of children and their families during the pandemic. COVID-19, coronavirus disease 2019.
Housing Security
Homelessness is a major health disparity facing children, and this poses general difficulties to maintaining optimal pediatric health. It may also worsen the ability for children to maintain control over long-term illnesses, such as asthma or other allergic diseases. Epidemiologic studies have linked housing insecurity and poor housing conditions with worsening long-term conditions, such as asthma, and with increased risk of respiratory infections that can precipitate asthma exacerbations.4 Pest infestations including mouse infestation have also been linked broadly to pediatric asthma outcomes.5
Prepandemic, more than 500,000 families have experienced homelessness in the United States at some point in the previous decade.6 A fact often missed is that up to 59% of people experiencing homelessness are children, and in a 1-year period, close to 5% of adolescents reported homelessness unaccompanied by an adult caregiver.7 , 8 There has been a significant increase in housing insecurity and homelessness during COVID-19. It has been estimated in the United States that an additional 400,000 shelter beds are required to accommodate all families experiencing homelessness during the current pandemic.9
This increase in housing insecurity in the United States may have profound impacts on children. One such impact is the increased risk of COVID-19 disease spread among multigenerational families in overcrowded housing. In a Boston study of 408 individuals experiencing homelessness and living in a shelter, 147 (36%) had a positive polymerase chain reaction test result for severe acute respiratory syndrome coronavirus 2.10 Families experiencing homelessness are more difficult to track, contact trace, and both treat or vaccinate for COVID-19 than the general population.11 This higher risk of COVID-19 transmission and morbidity is attributed to a variety of factors. Families experiencing homelessness may have reduced access to public health measures to reduce COVID-19 transmission, such as the ability to self-isolate and access hygiene supplies.8 , 11 Crowded living facilities, such as shelters or campgrounds, especially those with communal kitchens and bathrooms, reduce the ability to physically distance.8 , 11 Families facing homelessness also have reduced access to health care and screening facilities and are generally more mobile, which makes contact tracing and medical treatment more challenging.12 , 13 Children experiencing homelessness and their families have higher rates of underlying medical comorbidities that put them at higher risk of infection in general and have higher acuity as a result of these infections, including being more likely to require emergency department care.8 , 14 This, in particular, could be troublesome for children with asthma or who are immunocompromised.
Poor community housing conditions (such as overcrowding or incomplete kitchen or plumbing facilities) affect up to 15% of US families and can also influence COVID-19 outcomes.15 A cross-sectional analysis of count-level data from the US Centers for Disease Control and Prevention of 3135 US counties found that for each 5% increase in percent households with poor housing conditions, there was a 50% higher risk of COVID-19 incidence and a 42% higher risk of COVID-19 mortality.15 Families living in poverty are more likely to have jobs deemed essential and are more likely to use public transportation.16 , 17 Mobility data from an anonymized sample of smartphone users revealed a strong and statistically significant gradient between neighborhood income and physical distancing, associated with increased family employment outside of the home.18 To some degree, “the ability to practice social distancing has become a social determinant of health during this crisis.”8
Housing insecurity also has detrimental long-term impacts on the physical and psychological development of children. Children experiencing homelessness are at increased risk of lead poisoning, anemia, asthma, recurrent infections, poor dental hygiene and nutrition, educational-developmental delays, and psychiatric comorbidities, including depression and anxiety.19 , 20 Although “an ounce of prevention is worth a pound of cure” with respect to children and housing insecurity, the current pandemic and resulting economic insecurity has exacerbated the challenges in addressing and mitigating the impact of homelessness among children in the United States.20 It is unclear what impact this has had regarding outcomes with respect to specific allergic diseases, in particular those that need more regular follow-up care that could be disrupted by housing insecurity issues.
Various measures have been proposed to address the impact of housing insecurity, including a ban on evictions for failure to pay rent, meal programs in shelters that allow for physical distancing, increased numbers of beds within shelters, areas designed within shelters for isolation-quarantine and recovery, and drop-in sites in hotels and motels to increase capacity.12 , 21 Some municipalities have used existing infrastructure with increased capacity owing to the pandemic to enable self-isolation and ideal physical distancing, such as hotel rooms. To meaningfully affect the burden of housing insecurity, further expansion of both temporary and permanent solutions is needed, so that children have a stable housing situation, and this does not disrupt the family's ability to manage any chronic disease, including asthma, that the child may have.
Food Security
Food insecurity is defined by being unable to consistently access adequate and appropriate food and affected approximately 10% of US families before the COVID-19 pandemic.22 Food insecurity disproportionately affects specific populations, such as immigrant families, families headed by single women, families with lower healthy literacy, and Black or Hispanic families.23 In 2018, the prevalence of food insecurity was significantly higher in Black (21.2%) and Hispanic (16.2%) households than in the general population (11.1%).24 Estimates suggest that food insecurity in US households with children have doubled to tripled during the COVID-19 pandemic.25 , 26 As early as April 2020, it was reported that 2 in 5 households with preadolescent children were food-insecure (unable to afford for all family members to have enough food to live healthy lives), and 50% of these households were actively experiencing food insecurity.27 , 28
There is significant and long-term morbidity associated with even brief periods of food insecurity during childhood. Specific to allergic conditions, food insecurity has been linked with an increased risk of asthma in school-aged children, and household poverty strengthens this association. Poor nutrition is also tied to other risk factors for respiratory illness.26 For children with food allergy, food insecurity can be potentially dangerous as this may result in decreased access to allergen-safe foods for the child.29
More broadly, children from food-insecure households are at higher risk of developmental delay30 and behavioral issues, including anxiety and reduced social skills.31 Food insecurity in childhood is associated with a reduced immune innate and adaptive immune responses (which has the potential to increase risk of viral transmission)32 , 33 and increased risk of hospitalization.34 Longer-term food insecurity in childhood and adolescence is associated with many chronic diseases of adulthood, including type 2 diabetes and cardiovascular disease.35 In a retrospective cohort study at urban centers in the United States (N = 11,539 children), food-insecure children had a nearly 2-fold higher odds of “fair or poor” health (adjusted odds ratio, 1.9; 95% confidence interval, 1.66-2.18) and a higher odds of being hospitalized since birth (adjusted odds ratio, 1.31; 95% confidence interval, 1.16-1.48).36
The causes of this dramatic increase in food insecurity during the pandemic to some degree have been attributed in part to school closures and the resulting lack of access to the US Department of Agriculture National School Lunch Program, School Breakfast Program, and Child and Adult Care Food Program, on which more than 35 million children in the United States depend.32 , 37 School meals can comprise up to 70% of a child's daily nutrition needs, and it has been noted that meals eaten in schools are often healthier than those which are brought from home.32 Some of these meals also help guarantee provision of an allergen-safe meal in children with food allergy.29
Nevertheless, the dramatic increase in food insecurity during COVID-19 is not attributed to lack of school lunch programs alone (which may even further disproportionately affect children with food allergy and asthma dependent on such programs), and broader conceptual and bidirectional models to explain the impact of COVID-19 on food insecurity have been developed.38 For example, changes to the fragile food system (increased demand for food at home, disruptions to food supply) and structural factors (increased unemployment, reduced grocery store donations to food banks with increased panic purchasing, higher costs for food banks) contribute as well.38 Of those who lost their jobs during the pandemic, 31% report food insecurity and 33% report eating less owing to financial constraints.39 It has been noted that already vulnerable populations are more likely to have both higher rates and more intense forms of food insecurity during COVID-19, which is predicted to persist long after the immediate effects of the pandemic have resolved.38
There have been various solutions proposed to help address the issue of food insecurity among children, especially with respect to lack of access to the school lunch programs. One solution, which has been implemented in some states, involves “grab and go” meal sites or meal deliveries to bus stops or homes.32 Nevertheless, it has been noted that this approach may not ensure equitable food distribution and may not access those at highest need or provide access to allergen-safe food that children with food allergy require.32 Another recommended approach is to adopt the US Department of Agriculture's summer feeding program structure within school districts.32 Pediatricians and other primary care providers have a role in screening for food insecurity and assisting with liaising families with federal nutritional assistance programs.40
Familial Income, Social Status, and Neighborhood
The World Bank has estimated that the global rate of extreme poverty (living on <$1.90 per day) is expected to rise for the first time in more than 20 years as a result of the COVID-19 pandemic.41 Preliminary estimates are that an additional 88 to 115 million people will be categorized as living in extreme poverty, with the total rising to up to 150 million by the end of 2021. The United States has the highest child poverty rate among all high-income countries (approximately 22%) with this level anticipated to rise during the current pandemic.42 Close to 8 million Americans experienced poverty between the spring and fall of 2020, with close to 900,000 families filing for unemployment benefits in a single week in the fall.43
Poverty is strongly associated with the risk of COVID-19 infection and adverse outcomes. A US study documented that counties with higher overall poverty had larger numbers of confirmed COVID-19 cases, and greater number of deaths attributed to COVID-19, than counties with lower poverty.16 Another US study, inclusive of 158 counties in 10 major US cities, found that the death rate owing to COVID-19 was 3.8 times higher among counties with more, vs less, poverty.44 There are many potential contributors to this, including the following: poor housing conditions, unemployment or employment in a field considered essential with greater exposure risk, use of public transportation, and lack of health care access (which may be a compounded risk for children with chronic disease).16 , 17
There is also a longer-term impact of poverty on childhood development and health. Poverty is associated with reduced educational attainment (with high school graduation rates less than 50% in areas of the United States with high poverty rates) and lower IQ (even after correcting for parental age, marital status, education, and ethnicity).42 Living in poverty increases the risk of childhood infection, chronic disease into adulthood, and mental health outcomes as well.42
There are no economic stimulus packages within the United States which have specifically targeted children directly.37 Although various relief packages, such as the US Families First Coronavirus Response Act and the US Coronavirus Aid, Relief and Economic Security Act, may indirectly affect children, a focus specifically on the impact of poverty on long-term outcomes of children is absolutely essential.37
Educational Attainment
Public policies such as school closures, although often essential to mitigate the spread of COVID-19, have a disproportionately negative impact in those already facing other adverse social determinants. School closures have had a significant impact on school performance especially among vulnerable populations. Brown University projected, based on learning patterns of 5 million students, that school-aged children in the United States started school in the fall having learned less than 50% of math skills and less than 70% of language art skills than they would have acquired with in-person learning the previous spring.45 A decision analytical model found that missed instruction owing to school closures in the United States in the spring of 2020 would be associated with an estimated 5.53 million years of life lost, which was greater than would have been observed if primary schools had been left open during the first wave of the pandemic.46
Although school closures have occurred in 138 countries and affected the education of approximately 80% of children worldwide,47 losses in educational attainment are estimated to be more severe among those already facing adverse social determinants including those from lower-income or single-income households, families in whom English is a second language, and families who do not have access to technology at home.45 A recent editorial poignantly stated that “no credible scientist, learning expert, teacher or parent believes that children aged 5 to 10 years can meaningfully engage in online learning without considerable parental involvement, which many families with low incomes are unable to provide because parents must work outside the home.”48 In some low-income urban areas of the United States, up to 30% of students were not participating in online classes in the spring, largely owing to lack of virtual access at home.37 In 2020, although 81% of adults with an income of more than $75,000 per year use the internet, only 34% of those with an income of less than $30,000 per year use the internet.49 Long-term absenteeism (missing more than 10% of the school year) disproportionately affects children living in poverty, a gap that has been further widened with COVID-19, and has been associated with poorer long-term educational outcomes, including higher school dropout rates.37 For children dependent on school-based health programs for management of chronic diseases, school closures may critically risk reducing access to necessary care, including school-based asthma management programs.50
The Organization for Economic Cooperation and Development has estimated that school closures in the spring will result in approximately a 3% lower income for children affected by the closures over their entire lifetime, but it will be even more deeply felt by vulnerable children who will have larger learning losses, and therefore deeper losses in lifetime earnings.51 As described in a recent editorial, the impact of school closures on children living in poverty has been deemed a “social crisis in the making.”47
Moving forward, it has been suggested that “future decisions regarding school closures during the pandemic should consider the association between educational disruption and decreased expected lifespan and give greater weight to the potential outcomes of school closure on children's health.”46 In addition, decisions regarding school closures must bear in mind providing support to lower-income families, who are much more affected by school closures.
Abuse and Child Maltreatment
Internationally, there has been a dramatic increase in reports of abuse-related head injuries, and other injuries indicative of child abuse, during the COVID-19 pandemic. Child maltreatment and abuse have been associated with a variety of long-term adverse health outcomes, including psychological disorders (eg, depression, anxiety disorder, eating disorders, posttraumatic stress disorder), high-risk behaviors (eg, smoking, alcohol abuse, unsafe sexual practices), and overall lower health status.52 In the first month of the pandemic in the United Kingdom, there was a more than 100-fold increase in admissions for suspected abusive head trauma in the United Kingdom.53 In April 2020, reports of child abuse and maltreatment to the Childhelp National Child Abuse Hotline in the United States increased approximately 20% compared with the previous year.54 Notably, these statistics may still reflect some degree of underreporting of suspected abuse owing to pandemic school closures and fewer child interactions with trusted adults outside the home.55
Both the World Health Organization and United Nations Children's Fund have identified school closures, unemployment, and social isolation (all of which have reduced usual sources of support for families) as contributing to an increased risk of child abuse.56 , 57 There has also been disruption in community based services that support families during times of stress, such as access to social workers, mental health care, and overall health care professionals.55 In the United States, approximately 20% of reports of abuse and neglect to child protective services are made by schools.58 Physical distancing measures, although at times essential, have resulted in a distancing of children from adults most likely to be protective, such as their teachers and other family members.55 School closures seem to be putting children at even higher risk than usual because a usual source of identification of abuse is not occurring. During the pandemic, as recently stated, “nobody's watching kids except the families … there may be abuse that hasn't been reported because nobody knows that it's happening.”54
These same social factors also put children at higher risk of sexual exploitation online, bullying, and exposure to intimate partner violence (IPV).53 , 59 A New York Times article noted a dramatic increase in calls on IPV within the United States; poignantly stating that “No one can leave … You're literally mandating that people who probably should not be together in the same space stay.”54 Stay-at-home public health recommendations have led to situations whereby those experiencing IPV are in such close quarters that reporting abuse is unfeasible and have increased concerns on leaving for a shelter where close contact may increase the risk of COVID-19 transmission.54 There have also been reductions in shelter personnel during the pandemic and closures of shelter hotlines.54 Loss of employment also makes it hard for those experiencing IPV to move out on their own.54 Domestic violence has been termed “a pandemic within a pandemic” in the United States, causing both short-term and long-term harm to the children involved.60 Witnessing IPV has been found to affect children's relationships with peers, dating partners, and long-term partners.61
It has been recommended that given school closures, school educators should receive training in identifying children at risk in a distance-learning model and screen for home safety with virtual learning models.58 In addition, as in the past, health care providers can play a key role in identifying child maltreatment and supporting vulnerable families, including screening for family stress, identifying children at risk, and recognizing signs of child maltreatment.55
Race or Ethnicity and Systemic Racism
In the United States, predominantly Black counties are experiencing 3 times the COVID-19 infection rate and 6 times the COVID-19 mortality rate compared with predominantly White counties.62 Moreover, COVID-19 vaccination rates are lagging in these same areas compared with predominantly White areas.63 Although the Black population comprises approximately 30% of the Chicago population, more than 50% of COVID-19 cases and almost 70% of COVID-19 fatalities in Chicago have been among the Black population.62 In a cross-sectional study of 2595 patients in the United States tested for COVID-19, test positivity and hospitalization were both independently associated with Black race.64 A retrospective study of COVID-19 daily death counts from 1976 US nonmetropolitan counties between March and July 2020 found that compared with counties in the bottom quartile of Black and Hispanic populations, counties in the top quartile of percent Black populations have an average daily increase that is 70% higher and counties in the top quartile of percent Hispanic have an average daily increase that is 50% higher.65 With COVID-19 vaccine rollout, the vaccination rate for the White population in the United States is double that of the vaccination rate for the Black population.66 Many of the same determinants that drive COVID-19 outcomes also drive asthma outcomes, including the risk of exacerbations.67
It has been stated that “racism, not race, drives inequity across the COVID-19 continuum”68 and what may have driven a disproportionate impact of COVID-19 on racialized communities is systemic racism that predated the pandemic, but continued during it. Food insecurity disproportionately affects Black and Hispanic households.38 Close to 80% of families experiencing homelessness identify as non-White.8 African Americans have poorer access to care and can have more comorbid medical conditions which put them at higher risk.69 , 70 Structural racism (an understanding that racism is not just a result of personal prejudice but also compounded by policy and social norms)71 and its impact on American neighborhoods have led to housing areas that are overcrowded and underserviced.72 A recent rapid review found evidence from 3 large observational studies of an association between race or ethnicity and socioeconomic deprivation and increased likelihood of COVID-19 infection and hospitalization.73 The noted health disparities by race are not driven by genetic constructs but instead by structural and interpersonal racism.74 As noted by the World Health Organization, “In societies marked by racial discrimination and exclusion, people's belonging to a marginalized racial-ethnic group affects every aspect of their status, opportunities and trajectory throughout the life-course.”75
Mitigating racism and its impacts both direct and indirect on this pandemic is by no means a straightforward task. Nevertheless, the first step in dealing with this contributor is first recognizing its influence and making a fulsome effort to prioritize strategies that promote equality rather than simply equity. The Centers for Disease Control and Prevention note that “Community- and faith-based organizations, employers, healthcare systems and providers, public health agencies, policy makers, and others all have a part in helping to promote fair access to health … (we must work together) to ensure that people have resources to maintain and manage their physical and mental health, including easy access to information, affordable testing, and medical and mental health care.”76 Nevertheless, community engagement is not enough, and broader more just policy solutions are urgently needed.
Conclusion
Much remains to be learned on the impact of adverse social determinants of health on the long-term outcomes of children as a result of the COVID-19 pandemic. Nevertheless, it is clear that children are facing more adverse determinants as a result of this pandemic and that there are both short-term and long-term implications associated. For those living in poverty or with other adverse social determinants of health, the pandemic has made a bad situation worse. Ongoing studies are required to measure the impact of COVID-19 on those with adverse social determinants, in particular among children.
Past pandemics have taught us that those facing adverse determinants suffer the brunt of any long-term impact.13 , 77 Moving forward, social determinants of health must be part of pandemic research priorities, public health and vaccination goals, and economic policy implementation. Figure 2 outlines future steps that could help address the disparities discussed herin.
Figure 2.
Future steps to addressing COVID-19 pandemic-related social disparities affecting children and their families. Six strategies to help improve on pandemic-related social disparities. COVID-19, coronavirus disease 2019.
The impact of the COVID-19 pandemic has further served to shed a light on the broad disparities that exist within our society and their direct and indirect impact on health outcomes. Nevertheless, there also remains the opportunity to further recognize how disparity directs health outcomes, particularly during a global pandemic, and to focus efforts to ameliorate unjust disparities moving forward.13 , 62 Success in reducing social disparities indeed has the potential to improve the long-term outcomes of children, perhaps even more poignantly so in times of crisis.
Footnotes
Disclosures: Dr Shaker is a member of the Joint Taskforce on Allergy Practice Parameters; has a family member who is the chief executive officer of Altrix Medical; serves on the editorial board of the Journal of Allergy and Clinical Immunology: In Practice, the Journal of Food Allergy, and the Annals of Allergy, Asthma & Immunology. Dr Greenhawt has received past support from the Agency for Healthcare Research and Quality; is an expert panel and coordinating committee member of the National Institute of Allergy and Infectious Diseases–sponsored guidelines for peanut allergy prevention; has served as a consultant for Aquestive; is a member of physician-medical advisory boards for DBV Technologies, Sanofi-Regeneron, Genentech, Nutricia, Novartis, Acquestive, Allergy Therapeutics, Pfizer, US World Meds, Allergenis, Aravax, and Prota, all unrelated to vacines-vaccine development or COVID-19 treatment; is a member of the scientific advisory council for the National Peanut Board; is a member of the Brighton Collaboration Criteria Vaccine Anaphylaxis 2.0 working group; is the senior associate editor for the Annals of Allergy, Asthma, and Immunology, and is member of the Joint Taskforce on Allergy Practice Parameters. He has received honorarium for lectures from ImSci and MedLearningGroup. The remaining authors have no conflicts of interest to report.
Funding: The authors have no funding sources to report.
References
- 1.Johns Hopkins Coronavirus Resource Center. Available at: https://coronavirus.jhu.edu/map.html. Accessed October 15, 2021.
- 2.World Health Organization. Social determinants of health. Available at: https://www.who.int/social_determinants/sdh_definition/en/. Accessed August 1, 2021.
- 3.Daniel H, Bornstein SS, Kane GC, et al. Addressing social determinants to improve patient care and promote health equity: an American College of Physicians position paper. Ann Intern Med. 2018;168(8):577–578. doi: 10.7326/M17-2441. [DOI] [PubMed] [Google Scholar]
- 4.Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92(5):758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abrams EM, Szefler SJ, Becker AB. Time for allergists to consider the role of mouse allergy in non-inner city children with asthma. J Allergy Clin Immunol Pract. 2019;7(6):1778–1782. doi: 10.1016/j.jaip.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 6.The Council of Economic Advisers the State of Homelessness in America. 2019. Available at: https://www.nhipdata.org/local/upload/file/The-State-of-Homelessness-in-America.pdf. Accessed August 1, 2021.
- 7.Morton MH, Dworsky A, Matjasko JL, et al. Prevalence and correlates of youth homelessness in the United States. J Adolesc Health. 2018;62(1):14–21. doi: 10.1016/j.jadohealth.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coughlin CG, Sandel M, Stewart AM. Homelessness, children, and COVID-19: a looming crisis. Pediatrics. 2020;146(2):e20201408. Available at: https://pediatrics.aappublications.org/content/146/2/e20201408.abstract. Accessed August 1, 2021. [DOI] [PubMed]
- 9.National Alliance to End Homelessness. Population at-risk: homelessness and the COVID-19 crisis. Available at: http://endhomelessness.org/wp-content/uploads/2020/03/Covid-Fact-Sheet-3.25.2020-2.pdf. Accessed August 1, 2021.
- 10.Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA. 2020;323(21):2191–2192. doi: 10.1001/jama.2020.6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Heal. 2020;5(4):e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perri M, Dosani N, Hwang SW. COVID-19 and people experiencing homelessness: challenges and mitigation strategies. CMAJ. 2020;192(26):E716–E719. doi: 10.1503/cmaj.200834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med. 2020;8(7):659–661. doi: 10.1016/S2213-2600(20)30234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beharry MS, Christensen R. Homelessness in pediatric populations: strategies for prevention, assistance, and advocacy. Pediatr Clin North Am. 2020;67(2):357–372. doi: 10.1016/j.pcl.2019.12.007. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad K, Erqou S, Shah N, et al. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PLoS One. 2020;15(11):e0241327. doi: 10.1371/journal.pone.0241327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finch WH, Finch MEH. Poverty and COVID-19: rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Front Sociol. 2020;5:47. doi: 10.3389/fsoc.2020.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel JA, Nielsen FBH, Badiani AA, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. 2020;183:110–111. doi: 10.1016/j.puhe.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jay J, Bor J, Nsoesie EO, et al. Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat Hum Behav. 2020;4(12):1294–1302. doi: 10.1038/s41562-020-00998-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hwang SW. Homelessness and health. CMAJ. 2001;164(2):229–233. [PMC free article] [PubMed] [Google Scholar]
- 20.Dwomoh I, Dinolfo EA. Effects of homelessness on children. Pediatr Rev. 2018;39(10):530–532. doi: 10.1542/pir.2018-0047. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Laws and Regulations. 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cdcresponse/laws-regulations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcovid-eviction-declaration.html. Accessed August 1, 2021.
- 22.National Research Council . The National Academies Press; Washington, DC: 2006. Food Insecurity and Hunger in the United States: an Assessment of the Measure. Panel to Review the U.S. Department of Agriculture's Measurement of Food Insecurity and Hunger. [Google Scholar]
- 23.Chilton M, Black MM, Berkowitz C, et al. Food insecurity and risk of poor health among US-born children of immigrants. Am J Public Health. 2009;99(3):556–562. doi: 10.2105/AJPH.2008.144394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman-Jensen AR, Rabbitt MP, Gregory CA, Singh A. US Department of Agriculture, Economic Research Service; Washington, DC: 2019. Household Food Insecurity in the United States in 2018. ERR-270. [Google Scholar]
- 25.Hetrick RL, Rodrigo OD, Bocchini CE. Addressing pandemic-intensified food insecurity. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-006924. [DOI] [PubMed] [Google Scholar]
- 26.Sinha IP, Lee AR, Bennett D, et al. Child poverty, food insecurity, and respiratory health during the COVID-19 pandemic. Lancet Respir Med. 2020;8(8):762–763. doi: 10.1016/S2213-2600(20)30280-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bauer KW, Chriqui JF, Andreyeva T, et al. A safety net unraveling: feeding young children during COVID-19. Am J Public Health. 2020;111(1):116–120. doi: 10.2105/AJPH.2020.305980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bauer L. Brookings Institution; Washington, DC: 2020. The COVID-19 Crisis Has Already Left Too Many Children Hungry in America. [Google Scholar]
- 29.Brown E, Das R, Brewer AG, Martinez E, Bilaver LA, Gupta RS. Food insecure and allergic in a pandemic: a vulnerable population. J Allergy Clin Immunol Pract. 2020;8(7):2149–2151. doi: 10.1016/j.jaip.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rose-Jacobs R, Black MM, Casey PH, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121(1):65–72. doi: 10.1542/peds.2006-3717. [DOI] [PubMed] [Google Scholar]
- 31.Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–e868. doi: 10.1542/peds.2006-0239. [DOI] [PubMed] [Google Scholar]
- 32.Dunn CG, Kenney E, Fleischhacker SE, Bleich SN. Feeding low-income children during the COVID-19 pandemic. N Engl J Med. 2020;382(18):e40. doi: 10.1056/NEJMp2005638. [DOI] [PubMed] [Google Scholar]
- 33.Bourke CD, Berkley JA, Prendergast AJ. Immune dysfunction as a cause and consequence of malnutrition. Trends Immunol. 2016;37(6):386–398. doi: 10.1016/j.it.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cook JT, Black M, Chilton M, et al. Are food insecurity's health impacts underestimated in the U.S. population? Marginal food security also predicts adverse health outcomes in young U.S. children and mothers. Adv Nutr. 2013;4(1):51–61. doi: 10.3945/an.112.003228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.COUNCIL ON COMMUNITY PEDIATRICS; COMMITTEE ON NUTRITION Promoting food security for all children. Pediatrics. 2015;136(5):e1431–e1438. doi: 10.1542/peds.2015-3301. [DOI] [PubMed] [Google Scholar]
- 36.Cook JT, Frank DA, Berkowitz C, et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134(6):1432–1438. doi: 10.1093/jn/134.6.##. [DOI] [PubMed] [Google Scholar]
- 37.Dooley DG, Bandealy A, Tschudy MM. Low-income children and coronavirus disease 2019 (COVID-19) in the US. JAMA Pediatr. 2020;174(10):922–923. doi: 10.1001/jamapediatrics.2020.2065. [DOI] [PubMed] [Google Scholar]
- 38.Leddy AM, Weiser SD, Palar K, Seligman H. A conceptual model for understanding the rapid COVID-19-related increase in food insecurity and its impact on health and healthcare. Am J Clin Nutr. 2020;112(5):1162–1169. doi: 10.1093/ajcn/nqaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Raifman J, Bor J, Venkataramani A. Unemployment insurance and food insecurity among people who lost employment in the wake of COVID-19. medRxiv. Preprint posted online July 30, 2020. doi:10.1101/2020.07.28.20163618 [DOI] [PMC free article] [PubMed]
- 40.Frank DA, Bruce C, Ochoa E. SNAP is medicine for food insecurity. Pediatrics. 2020;146(3) doi: 10.1542/peds.2020-002105. [DOI] [PubMed] [Google Scholar]
- 41.The World Bank. COVID-19 to add as many as 150 million extreme poor by 2021. Available at: https://www.worldbank.org/en/news/press-release/2020/10/07/covid-19-to-add-as-many-as-150-million-extreme-poor-by-2021. Accessed August 1, 2021.
- 42.Wood D. Effect of child and family poverty on child health in the United States. Pediatrics. 2003;112(3 Part 2):707–711. [PubMed] [Google Scholar]
- 43.BBC. Coronavirus: US poverty rises as aid winds down. 2020. Available at: https://www.bbc.com/news/business-54559008. Accessed August 1, 2021.
- 44.Adhikari S, Pantaleo NP, Feldman JM, Ogedegbe O, Thorpe L, Troxel AB. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw Open. 2020;3(7):e2016938. doi: 10.1001/jamanetworkopen.2020.16938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brown University. Projecting the potential impacts of COVID-19 school closures on academic achievement. Available at: https://edworkingpapers.com/sites/default/files/ai20-226-v2.pdf. Accessed August 1, 2021.
- 46.Christakis DA, Van Cleve W, Zimmerman FJ. Estimation of US children's educational attainment and years of life lost associated with primary school closures during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(11):e2028786. doi: 10.1001/jamanetworkopen.2020.28786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van Lancker W, Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. Lancet Public Heal. 2020;5(5):e243–e244. doi: 10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Christakis DA. School reopening-the pandemic issue that is not getting its due. JAMA Pediatr. 2020;174(10):928. doi: 10.1001/jamapediatrics.2020.2068. [DOI] [PubMed] [Google Scholar]
- 49.Pew Research Center. Internet/broadband fact sheet. 2021. Available at: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/. Accessed August 1, 2021.
- 50.Lemanske RFJ, Kakumanu S, Shanovich K, et al. Creation and implementation of SAMPRO: a school-based asthma management program. J Allergy Clin Immunol. 2016;138(3):711–723. doi: 10.1016/j.jaci.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hanushek EA, Woessmann L. The economic impacts of learning losses. 2020. Available at: http://www.oecd.org/education/The-economic-impacts-of-coronavirus-covid-19-learning-losses.pdf. Accessed XXX.
- 52.Springer KW, Sheridan J, Kuo D, Carnes M. The long-term health outcomes of childhood abuse. An overview and a call to action. J Gen Intern Med. 2003;18(10):864–870. doi: 10.1046/j.1525-1497.2003.20918.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuehn BM. Surge in child abuse, harm during COVID-19 pandemic reported. JAMA. 2020;324(7):621. doi: 10.1001/jama.2020.14433. [DOI] [PubMed] [Google Scholar]
- 54.New York Times. domestic violence calls mount as restrictions linger: ‘no one can leave’. Available at: https://www.nytimes.com/2020/05/15/us/domestic-violence-coronavirus.html. Accessed August 1, 2021.
- 55.Kang K, Jain N. Child abuse and neglect in the COVID-19 era: a primer for front-line physicians in British Columbia. BC Med J. 2020;62(7):238–240. [Google Scholar]
- 56.UNICEF. Global status report on preventing violence against children 2020. Available at: https://www.unicef.org/media/70731/file/Global-status-report-on-preventing-violence-against-children-2020.pdf. Accessed August 1, 2021.
- 57.World Health Organization. Countries failing to prevent violence against children, agencies warn. Available at: https://www.who.int/news/item/18-06-2020-countries-failing-to-prevent-violence-against-children-agencies-warn. Accessed August 1, 2021.
- 58.Thomas EY, Anurudran A, Robb K, Burke TF. Spotlight on child abuse and neglect response in the time of COVID-19. Lancet Public Health. 2020;5(7):e371. doi: 10.1016/S2468-2667(20)30143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557. doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Evans ML, Lindauer M, Farrell ME. A pandemic within a pandemic - intimate partner violence during COVID-19. N Engl J Med. 2020;383(24):2302–2304. doi: 10.1056/NEJMp2024046. [DOI] [PubMed] [Google Scholar]
- 61.Wood SL, Sommers MS. Consequences of intimate partner violence on child witnesses: a systematic review of the literature. J Child Adolesc Psychiatr Nurs. 2011;24(4):223–236. doi: 10.1111/j.1744-6171.2011.00302.x. [DOI] [PubMed] [Google Scholar]
- 62.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 63.Ndugga N, Hill L, Artiga S, Haldar S. Latest data on COVID-19 vaccinations by race/ethnicity. 2021. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/. Accessed August 1, 2021.
- 64.Muñoz-Price LS, Nattinger AB, Rivera F, et al. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw Open. 2020;3(9):e2021892. doi: 10.1001/jamanetworkopen.2020.21892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cheng KJG, Sun Y, Monnat SM. COVID-19 death rates are higher in rural counties with larger shares of Blacks and Hispanics. J Rural Health. 2020;36(4):602–608. doi: 10.1111/jrh.12511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.New York Times. pandemic's racial disparities persist in vaccine roll out. Available at: https://www.nytimes.com/interactive/2021/03/05/us/vaccine-racial-disparities.html. Accessed August 1, 2021.
- 67.Aligne CA, Auinger P, Byrd RS, Weitzman M. Risk factors for pediatric asthma. Contributions of poverty, race, and urban residence. Am J Respir Crit Care Med. 2000;162(3 Pt 1):873–877. doi: 10.1164/ajrccm.162.3.9908085. [DOI] [PubMed] [Google Scholar]
- 68.Khazanchi R, Evans CT, Marcelin JR. Racism, not race, drives inequity across the COVID-19 continuum. JAMA Netw Open. 2020;3(9):e2019933. doi: 10.1001/jamanetworkopen.2020.19933. [DOI] [PubMed] [Google Scholar]
- 69.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. In: Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press (US); 2003. [PubMed]
- 71.Bailey ZD, Feldman JM, Bassett MT. How structural racism works - racist policies as a root cause of U.S. racial health inequities. N Engl J Med. 2020;384(8):768–773. doi: 10.1056/NEJMms2025396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wright LS, Louisias M, Phipatanakul W, et al. The United States’ reckoning with racism during the COVID-19 pandemic: what can we learn and do as allergist-immunologists? J Allergy Clin Immunol. 2021;147(2):504–506. doi: 10.1016/j.jaci.2020.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Upshaw TL, Brown C, Smith R, Perri M, Ziegler C, Pinto AD. Social determinants of COVID-19 incidence and outcomes: a rapid review. PLoS One. 2021;16(3):e0248336. doi: 10.1371/journal.pone.0248336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.The Lancet Diabetes Endocrinology COVID-19 and racism-a double edged dagger. Lancet Diabetes Endocrinol. 2020;8(8):649. doi: 10.1016/S2213-8587(20)30243-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.World Health Organization. A conceptual framework for action on the social determinants of health. Available at: https://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf?ua=1. Accessed August 1, 2021.
- 76.Centers for Disease Control and Prevention. Health equity considerations and racial and ethnic minority groups. 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Accessed August 1, 2021.
- 77.Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Heal. 2020;5(5):e240. doi: 10.1016/S2468-2667(20)30085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]