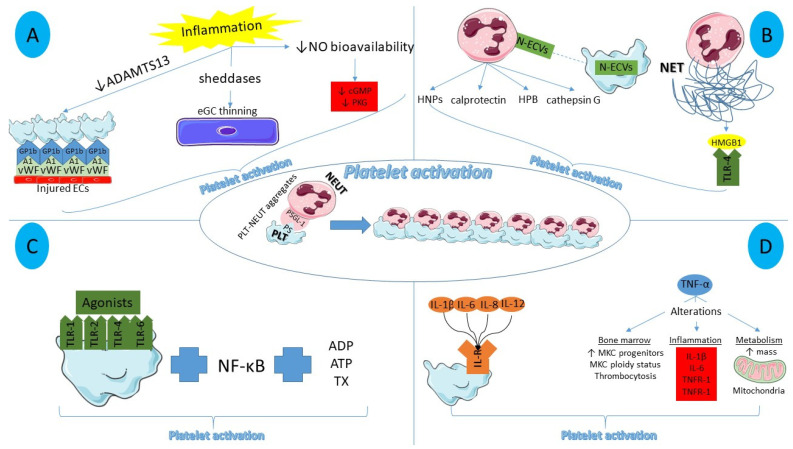
Figure 1.
Main inflammatory mediators of platelet activation. (A) Endothelial dysfunction in the setting of inflammation results in increased platelet–endothelial cell interactions, thinning of endothelial glycocalyx, and reduced nitric oxide bioavailability, contributing to platelet activation. (B) Neutrophil-derived molecules and extracellular vesicles aid platelet activation, together with the pro-thrombotic role of NET histones via a Toll-like receptor 4-related platelet activation. (C) Platelet toll-like receptors cannot directly induce platelet activation but they augment it, stimulated by NF-κB, thromboxane, adenosine diphosphate, and adenosine triphosphate. (D) Pro-inflammatory interleukins bind to interleukin receptors situated on the platelet surface while tumor necrosis factor-alpha promotes alterations in bone marrow, inflammation, and mitochondria, collectively facilitating platelet activation. ADAMTS13: A disintegrin-like and metalloprotease with thrombospondin type-1 repeats-13, NO: nitric oxide, EC: endothelial cells, eGC: endothelial glycocalyx, cGMP: cyclic guanyl monophosphate, PKG: protein kinase G, N-ECV: neutrophil extracellular vesicles, HNP: human neutrophil peptides, HBP: heparin binding protein, NET: neutrophil extraceullar trap, HMGB1: High mobility group box 1, TLR: toll-like receptor, ADP: adenosine diphosphate, ATP: adenosine triphosphate, TX: thromboxane, IL-R: interleukin receptor, MKC: megakaryocyte, TNFR: tumor necrosis factor receptor, PS: P Selectin, PSGL-1: P Selectin glycoprotein ligand-1, NEUT: neutrophil, PLT: platelet.