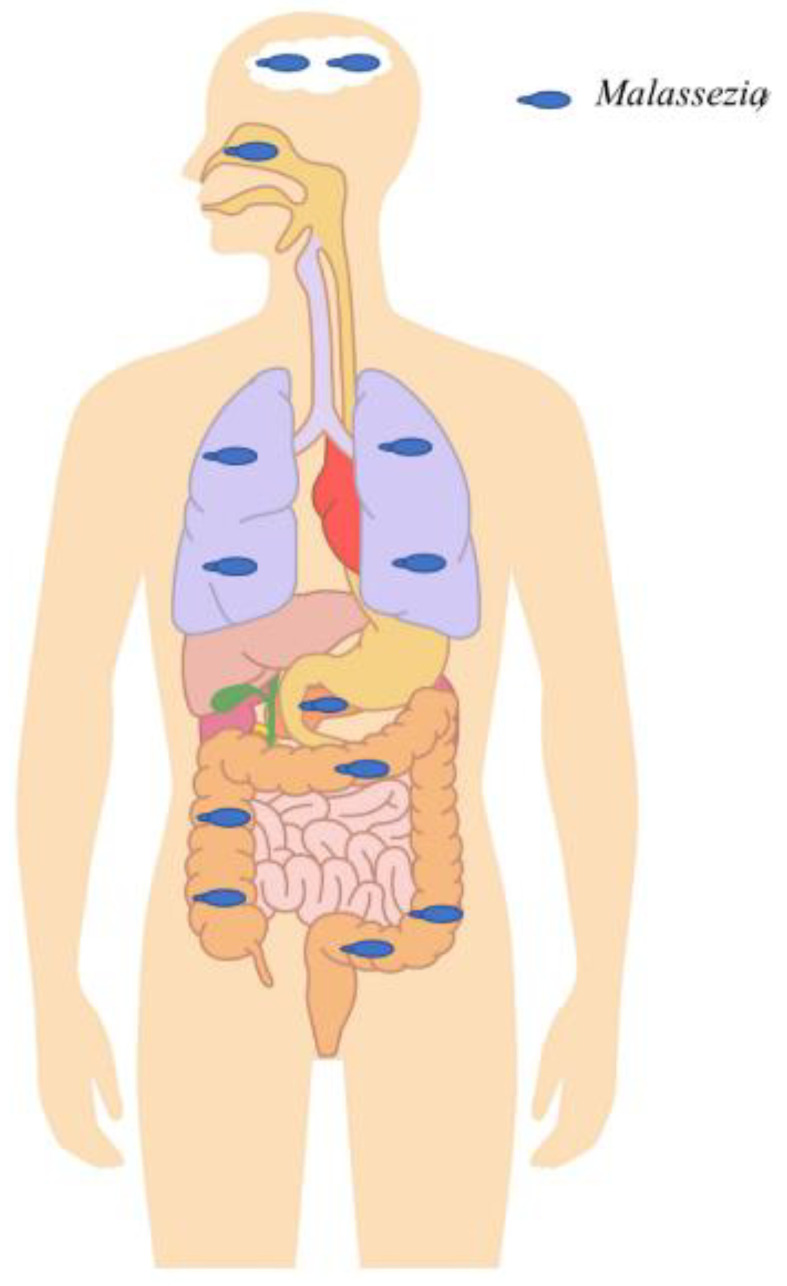
Figure 2.
Malassezia in different anatomical sites detected in the context of chronic diseases or healthy individuals outside the skin. Malassezia was abundantly detected in the digestive tract and was shown to be associated with Crohn’s disease by exacerbating colitis and inflammation. Furthermore, it was highly abundant in colorectal cancer patients compared to healthy subjects, suggesting a potential role in tumorigenesis. It was also shown to be able to migrate from the gastrointestinal tract lumen to the pancreas and to exacerbate pancreatic adenocarcinoma progression. High abundance was also found in the gastrointestinal tracts of HIV patients, probably due to HIV-related immunosuppression. It was highly detected in the upper and lower respiratory tract. Within the upper respiratory tract, it has been shown to interact with specific bacteria (Pseudomonas aeruginosa and Staphylococcus aureus) and to increase chronic rhinosinusitis-associated inflammation. Within the lower respiratory tract, it was shown to be associated with cystic fibrosis pulmonary exacerbations. Finally, Malassezia were detected with a relatively high prevalence and abundance in brain tissue samples of patients with neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease, etc.