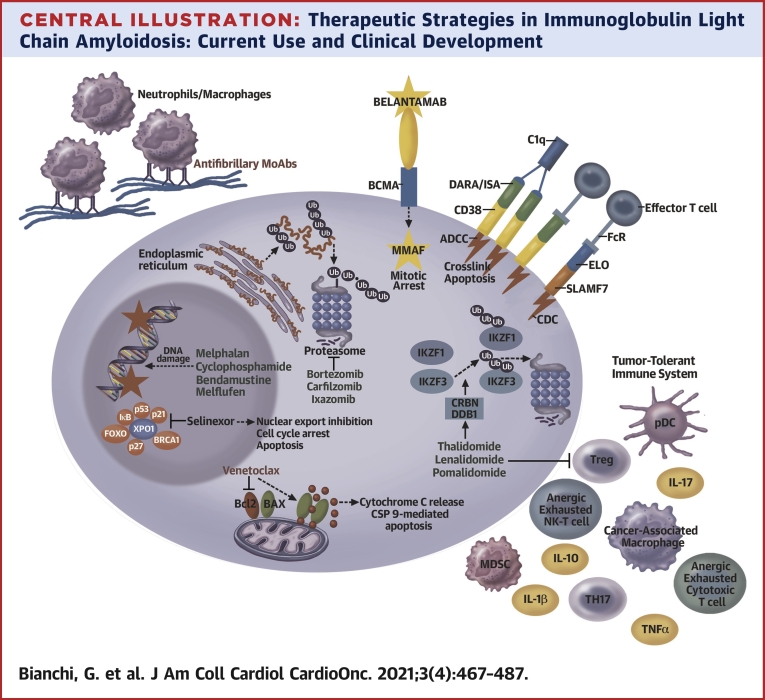
Central Illustration.
Therapeutic Strategies in Immunoglobulin Light Chain Amyloidosis: Current Use and Clinical Development
The Figure outlines the target and/or mechanisms of action of the most frequently used drugs in immunoglobulin light chain amyloidosis and agents in advanced clinical development. Proteasome inhibitors block the function of the proteasome, inducing polyubiquitinated protein accumulation. IMiDs induce Ikaros and Aiolos (IKZF1 and IKZF2, respectively) proteasome-mediated degradation and enhance T-cell and NK-T-cell function. MoAbs DARA and ISA cause complement-dependent cytotoxicity (CDC), antibody-dependent cell cytotoxicity (ADCC), and direct cytotoxicity from crosslinking. ELO triggers ADCC, and the antibody drug conjugated (ADC) targeting BCMA, belantamab mafodotin, induces DNA damage via MMAF. Alkylating agents similarly induce DNA damage and selinexor blocks XPO1. Venetoclax binds BCL2, releasing BAX and triggering cytochrome C release and caspase 9-mediated apoptosis. Antifibrillary antibodies facilitating macrophage-mediated amyloid reabsorption are depicted in the top left corner. U.S. Food and Drug Administration–approved drugs in MM therapy are green, whereas investigational agents are in red. DARA = daratumumab; ELO = elotuzumab; IL = interleukin; ISA = isatuximab; MMAF = monomethyl auristatin F; TNFα = tumor necrosis factor alpha; MDSC = myeloid derived suppressor cell; pDC = plasmacytoid dendritic cell; TH17 = T helper 17; Treg = regulatory T cells; Ub = ubiquitin; XPO1 = exportin 1.