Abstract
Objective
This study aimed to evaluate the association between perceived social support during pregnancy and levels of anxiety among postpartum women using an anxiety-specific screening instrument.
Methods
Using a prospective cohort design, a two-stage methodology was conducted to collect data from women seeking maternal care at the King Abdullah University Hospital in northern Jordan. In the first stage, perceived social support was assessed among pregnant women using the Medical Outcomes Study Social Support Survey. During the first six months after childbirth, postpartum women were contacted to complete the second stage, wherein their perceptions of infant-focused anxieties were assessed using the Postpartum Specific Anxiety Scale. In our study, two types of infant-focused anxieties were investigated among a final sample of 419 mothers: infant safety and welfare anxieties and practical infant care anxieties.
Results
The results of multivariate linear regression analysis indicated that providing pregnant women with high levels of emotional support from close social networks (β= −0.08, p= 0.01) and perceiving informational support from health care providers (β= −0.71, p< 0.01) were protective factors for reducing the levels of postpartum anxiety concerning infant safety and welfare. Our findings also demonstrated that pregnant mothers who perceived high informational support from health care providers had a lower level of postpartum anxiety about practical infant care (β= −0.20, p< 0.01). In contrast, mothers who reported receiving high tangible support from close social networks during pregnancy had a significantly higher level of perceived anxiety concerning practical infant care after delivery (β= 0.13, p= 0.02).
Conclusion
Our study suggests that postpartum anxiety would be reduced if effective informational support were readily available for pregnant women. There is a clear need for building bridges between women, their families, and providers to distinguish the specific type and amount of support that should be provided to mothers during pregnancy.
Keywords: postpartum anxiety, infant care, social support, pregnancy, childbirth, postnatal care, infant-focused anxieties
Introduction
While the degree of response to the arrival of a new baby is normal and adaptive for many mothers, others may experience more severe, long-lasting changes in their emotional and mental health, including feelings of anxiety and depression.1 Anxiety disorders are common after childbirth, with an estimated incidence ranging from 6.1% to 27.9% of women experiencing anxiety symptoms during the first six months postpartum.2 Unlike postpartum depression (PPD), symptoms of anxiety experienced postnatally have been largely overlooked.2–5 Unfortunately, postpartum anxiety (PPA) is often not sufficiently differentiated by health care providers, mislabeling it as PPD or attributing it to infant care demands and changes in roles and responsibilities.6–9 According to a recent Canadian study by Fairbrother et al,4 the prevalence of anxiety disorders during the early postpartum period (17.1%) exceeded the incidence of depression by more than three times (4.8%). Other studies have also suggested that anxiety occurs independently and more frequently than depression in the postpartum period.2,3,10,11
The World Health Organization (WHO) has reported that the postpartum period attracts little attention from healthcare providers compared to the prenatal and childbirth periods.8 The postpartum period is commonly defined as the time that begins immediately after childbirth and lasts for the next six months.12 About 80% of women experience at least some symptoms of postpartum blues shortly after giving birth.8,13 These symptoms typically include mood swings, crying spells, sleep disturbances, and fatigue.8,13 Postpartum blues usually begin the first couple of days after delivery and taper off by the end of the second week postpartum. While many mothers can bounce back to feeling more normal, others find the postpartum stage a challenging time that is further aggravated by excessive worries about infant safety and well-being, feelings of dissociation, and avoidance of social situations.2,12 Having such anxieties was also found to be associated with adverse consequences for mothers and children, including poor mother-infant bonding,8,14 newborn breastfeeding problems, excessive infant crying,5 and impaired behavioral, emotional, and developmental outcomes in the children.15–17 Consequently, accessing support and help, starting from pregnancy, functions as a buffer for psychological distress and may contribute to reducing anxiety symptoms after delivery and facilitating women’s transition into safe motherhood.8,18
Prior research has also reported that many postpartum women are troubled by obsessive and intrusive thoughts about the health and safety of their infants and may develop a phobia concerning the new baby, especially if the mothers are unsupported.11,19 Recent evidence has acknowledged that the lack of interpersonal interactions and support within the social network may lead to adverse mental health outcomes, such as feelings of isolation or disorientation, elevated psychological difficulties, and a relapse into depression.20 Perceived social support is defined as “the belief that members of one’s social network will provide resources, such as emotional, informational, and tangible support, when needed”.15 This support can be drawn from a variety of sources, including one’s partner, family, friends, and health care providers.21 Receiving social support and care from others has been found to be strongly associated with enhanced life satisfaction and better emotional well-being among women with preexisting life stresses such as pregnancy.15,21 Supporting mothers also helps with recovery during the postpartum period, benefits the parent–child relationship, helps families meet their physical, emotional, and financial needs, and improves long-term health consequences for both children and parents.21–24
To date, much attention has been given to social support in the postpartum period; however, the importance of giving such support may be even greater during pregnancy.25 Given that social support is not always received before the postnatal period, it remains unclear whether poor social support during pregnancy is related to the PPA state. It is therefore essential to prospectively evaluate the association between social support received during pregnancy and the levels of PPA. Importantly, no previous studies have investigated this relationship using postpartum-specific anxiety measures. The use of specific measures may predict postnatal outcomes more effectively than general measures do. In view of this, this study aimed to examine prospectively whether social support during pregnancy affected the levels of PPA using an anxiety-specific screening instrument.
Methods
Study Design and Procedures
Using a prospective cohort study design, the fieldwork stage of data collection started in June 2018 and ended in October 2019. In the current study, a two-stage methodology was conducted as follows:
Stage One
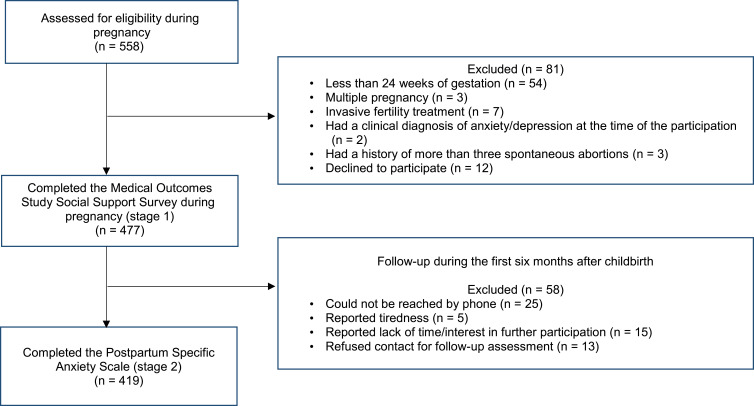
Pregnant women were recruited by word of mouth from obstetrical and gynecological clinics at King Abdullah University Hospital (KAUH) in northern Jordan. A total of 558 pregnant women were screened, and 69 women met exclusion criteria (gestational age <24 weeks, multiple pregnancies, current clinical diagnosis of psychiatric illness, invasive fertility treatment, and history of more than three spontaneous abortions). Additionally, 12 women were declined to participate due to a shortage of time. Overall, 477 women were eligible for the first stage of the current study. Figure 1 shows the full details of participation rates at each stage of the study.
Figure 1.
Participant flowchart.
During the face-to-face interviews, a well-trained female interviewer filled in a standardized questionnaire by requiring the participants to answer the questions relating to mother’s sociodemographic characteristics (ie, age, education, occupation, and income) and their perceptions of receiving specific types of social support from pre-identified sources of social support, including close social networks (ie, partner, first-degree relatives, and close friends); or health care providers (ie, doctors and nurses). At this stage, perceived social support was assessed using the Medical Outcomes Study Social Support Survey (MOS-SSS), which aims at evaluating the extent to which an individual has the support of others to face stressful situations.26 For instance, participants were asked several questions about general feelings of being loved and if there is someone in their close social networks who understands their problems, and they can count on to listen to them when they need to talk or share their most private worries and fears. Further, all participating women were questioned if there was someone in their closed social networks who could help them out when tangible assistance was needed; and if their health care providers gave them information and good advice about issues related to pregnancy and childbirth.26
Stage Two
Upon the participants’ approval, phone numbers were obtained from the mothers themselves during the first stage. Each woman was called to set up an appointment to administer a telephone interview and complete the second stage of the study. To be eligible for participation at this stage, only mothers to a single live birth between 0 and 6 months were included. Out of the 477 expectant mothers who participated in the first stage, 58 mothers (12.2%) were excluded from the final analysis, as they could not be reached by phone, reported tiredness or lack of time or interest in further participation, or refused contact for follow-up assessment. Accordingly, the final sample consisted of 419 mothers who were able to meet the inclusion criteria of the second stage and had completed the MOS-SSS at the preceding time point. At the second stage, mothers reported their perceptions of anxieties related to caring for their infants using a 51-item Postpartum Specific Anxiety Scale (PSAS).3 Information about each infant’s demographic characteristics was also collected, including the timing of birth, birth order and gender, and mode of birth. As the known dates of birth of the infants, their ages were calculated in months based on the date of each month following the month they were born. For instance, if a given baby was born on April 2nd, this baby would be two months old on June 2nd. For this study, the variable “age of the infant” was classified into two categories: less than three months and between three and six months.
The participating women were also asked about the mode of feeding of the infant, sleep patterns, and mood in the last seven days preceding the interview. The variable “mode of feeding” was categorized into exclusive and non-exclusive breastfeeding. In this variable, exclusive breastfeeding means that the infant was fed only breast milk with no solids or other oral intake, except vitamins, mineral supplements, or medication.27 Otherwise, the feeding mode was defined as non-exclusive breastfeeding.
Regarding the sleep-wake patterns of the newborns, the perceptions of the mothers about the nighttime awakenings of their infants were subjectively reported. The infant sleep pattern variable was classified into three categories based on the quality of sleep: sleepless night (ie, if the baby had frequent and prolonged nocturnal awakenings), little sleep (ie, if the baby had frequent nocturnal awakenings), and good sleep (ie, if the baby had uninterrupted sleeping at night). The mood of the infants was also assessed by the mothers participating in the research. It was categorized into quiet, changeable, and anxious moods.
Study Instruments
The Medical Outcomes Study Social Support Scale (MOS-SSS)
The MOS-SSS is a brief, easy-to-administer self-report questionnaire consisting of 19 items rated on a 5-point Likert scale with scores ranging from 1 (none of the time) to 5 (all the time). Higher scores on each 5-point Likert scale item indicate higher levels of perceived support. This instrument has been universally used and recommended for measuring four types of social support among a wide range of populations, including postpartum women.15,20,28 These types include emotional/informational support, tangible support, affectionate support, and positive social interaction. Although the MOS-SSS has proven to have good robust factorial validity and internal consistency,20,26 prior research has illustrated a different factorial structure than the original version of the scale,29,30 showing the existence of three factors with the grouping of items from two types of social support on a single factor. Accordingly, an exploratory factor analysis with oblique promax rotation was conducted on the data set of 419 subjects to identify the distinct factors involved. The assumptions for such an analysis were met with Kaiser-Meyer-Olkin (KMO) test for sampling adequacy (KMO = 0.77 and P < 0.01). Using eigenvalues greater than one, three factors were extracted, which in combination accounted for a cumulative variance of 67.67%. These factors were named as emotional support from closed social networks (eg, concern, comfort, encouragement, care, and love); informational support from health care providers (eg, advice, education, and knowledge sharing); and tangible support from closed social networks (eg, money, time, and other instrumental assistance). The item loadings on each factor are shown in Table 1. All the included items had loadings of >0.5 on their respective factors, reflecting good purification of constructs.31
Table 1.
Factor Loadings For the Rotated Factor Solution for the MOS-SSS Items
| Item description | Component | ||
| 1 | 2 | 3 | |
| Emotional support from your close social network (i.e., husband, first-degree relatives, and close friends) | |||
| Someone in your close social network makes you feel wanted. | 0.01 | 0.92 | 0.04 |
| You can turn to someone in your close social network for suggestions about how to deal with a personal problem. | 0.06 | 0.71 | -0.03 |
| You can share your most private worries and fears with someone in your close social network. | 0.16 | 0.71 | 0.01 |
| Someone in your close social network understands your problems. | -0.07 | 0.69 | 0.08 |
| You can count on someone in your close social network to listen to you when you need to talk. | -0.18 | 0.64 | 0.10 |
| Someone in your close social network shows you love and affection. | 0.22 | 0.62 | -0.13 |
| Informational support from healthcare providers (i.e., doctors and nurses) | |||
| Your healthcare providers offer you advice when you really want it. | 0.91 | 0.07 | -0.08 |
| Your healthcare providers give you information to help you understand a situation related to pregancny and childbirth. | 0.88 | 0.13 | -0.11 |
| Your healthcare providers give you good advice about your worries and fears. | 0.75 | -0.03 | 0.16 |
| Your healthcare providers make you feel confident when you talk to them about yourself or your problems. | 0.72 | 0.06 | 0.12 |
| Tangible support from your social network (i.e., husband, first-degree relatives, and close friends) | |||
| Someone in your close social network spends time with you. | -0.08 | 0.06 | 0.94 |
| Someone in your close social network takes you to the doctor if you need it. | -0.08 | 0.14 | 0.87 |
| Someone in your close social network prepares your meals if you are unable to do it yourself. | 0.18 | -0.06 | 0.76 |
| Someone in your close social network helps you with daily chores if you are sick. | 0.35 | -0.13 | 0.62 |
| Someone in your close social network engages with you to help get your mind off things. | 0.50 | -0.03 | 0.55 |
| Someone in your close social network helps you if you are confined to bed. | 0.49 | -0.02 | 0.54 |
| Someone in your close social network gets together with you to relax. | 0.46 | 0.03 | 0.56 |
| Someone in your close social network does something enjoyable with you. | 0.49 | -0.03 | 0.56 |
| % of variance explained | 44.42 | 15.73 | 7.52 |
| Cumulative % of variance | 44.42 | 60.15 | 67.67 |
| Cronbach’s alpha | 0.82 | 0.89 | 0.92 |
Note: significant loadings in boldAbbreviation: MOS-SSS, medical outcomes study social support survey.
For the purposes of this study, the MOS-SSS was translated into Arabic, the participants’ native language, and subsequently the validity and reliability of the MOS-SSS were retested. Our analyses demonstrated that the three factors had excellent internal consistency (with a Cronbach’s alpha range of 0.82 to 0.92) and low to moderate correlations (r values ranging from 0.26 to 0.39). This indicates that these factors are not derived from a single underlying latent variable. The overall scale also showed excellent reliability (Cronbach’s α = 0.91). The face validity of the tool was determined by giving the MOS-SSS to five experts working in the field of sociology. All experts accepted this tool as appropriate for measuring the different types of social support.
The Postpartum Specific Anxiety Scale (PSAS)
Mothers reported their perceptions of anxiety during the postnatal period using the 51-item PSAS. This valid and reliable tool was developed by Fallon et al3 to measure specific types of anxieties experienced by postpartum women, including maternal competence and attachment anxieties (15 items); infant safety and welfare anxieties (11 items); practical infant care anxieties (7 items); and psychosocial adjustment to motherhood anxieties (18 items). Mothers reported the frequency of experiencing each feeling on a scale ranging from 1 (not at all) to 4 (almost always). Higher scores on each 4-point Likert scale item show higher levels of PPA.
The timeframe for rating the frequency of anxieties was limited to the previous seven-day period. The seven-day cut-off point is congruent with the postpartum-specific anxiety scale suggested by Fallon et al3 and allows mothers to recall their postpartum experiences. Permission to use the PSAS instrument was obtained from the corresponding author in Fallon et al. study.3
In this regard, it is worth mentioning that the PSAS has been translated into several languages,32–34 but not Arabic. In view of that and for the purposes of the current study, the PSAS was translated from English into Arabic by two independent bilingual translators who are experts in perinatal psychology and speak Arabic as their native language. To ensure the accuracy of the translation process, this forward translation was then back-translated from Arabic into English by another two independent translators whose native language was English and second language was Arabic. This forward–backward translation process was conducted twice, and then a final meeting of all forward and backward translators was conducted for fine tuning of the PSAS Arabic version.
Thereafter, three consultants in obstetrics and gynecology and two perinatal psychologists who were not involved in the previous translation were requested to evaluate the content validity of the Arabic version of the PSAS. To this end, the experts, as a panel, were asked to rate the PSAS items for clarity and relevancy to the construct underlying the study on a scale ranging from 1 (not relevant) to 4 (very relevant). To quantify the judgment of content validity across experts, the content validation ratio (CVR) was calculated and displayed a mean of 0.79, indicating a good content validity of the Arabic version of the PSAS.3
To examine the reliability of the Arabic version of the PSAS, test–retest reliability was analyzed through Pearson’s correlation in a period of three weeks for a sub-sample of participants (n = 48). The test–retest correlation coefficients were 0.77 for the total scale, and ranging from 0.68 to 0.89 for the subscales, showing the stability of the measure across time. The Cronbach’s alpha internal consistency coefficients were also computed and showed good internal consistency with α ≥ 0.80 for the overall PSAS scale and for the subscales.
Statistical Analyses
Data processing and analysis were performed using the Statistical Package for the Social Sciences (SPSS) version 21. Descriptive analyses of the study variables included count, percent, skewness, kurtosis, and mean with standard deviation.
Of the four types of postpartum anxieties measured by the PSAS,3 we focused our analysis on two specific types of anxieties experienced by postpartum women in relation to infant health and care. These types are: infant safety and welfare anxieties (ISWAs), which include 11 items related to fears about infant illnesses, accidents, and death; and practical infant care anxieties (PICAs), which involve 7 items covering anxieties that are specific to infant care, such as feeding, sleeping, and general routine.3 Using multivariate linear regression (MLR) analyses, two models were designed to predict the impact of perceived social support during pregnancy on infant-focused anxieties among the 419 postpartum women. The first and second models focused on investigating the ISWAs and the PICAs, respectively. Both ISWAs and PICAs were modeled as the total score across the items included in each subscale and considered as the study outcome variables, with higher scores representing higher levels of PPA. Assumptions for the linear regression models were met, including normality, linearity, and homoscedasticity, as well as the absence of multicollinearity.
Each type of social support was modeled as the total score across the items included in each subscale, with higher scores indicating higher levels of perceived support. Other data from prenatal and postpartum components were also included in the MLR analysis as independent variables. All of these variables were treated as categorical, except for education and age factors. The age of the women and their education were measured in years as continuous variables. All variables demonstrating a p-value of less than 0.05 were considered statistically significant. Each factor showing a statistically significant association with the response variable was interpreted after controlling for the effects of other explanatory variables included in the model. R-squared was used to assess the goodness of fit of the MLR models.
Ethical Approval
The Institutional Review Board (IRB) of the Jordan University of Science and Technology and the Ethics Committee at the KAUH approved the study protocol (protocol # 16/2016). The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all the study participants.
Results
Descriptive Analysis
Summary statistics for the sample population are presented in Table 2. In this study, the ages of recruited pregnant women were between 18 and 46 years, with a median age of 29 years old. The participants had completed an average of 12 years of education. The participants were also predominately unemployed (76.6%), had multiple children (69.7%), and had inadequate financial resources (77.1%). The percentages of women who reported that their pregnancy was unplanned and that they had a previous pregnancy loss or death of an infant were 56.6% and 19.1%, respectively.
Table 2.
Baseline Characteristics of the Sample Population (N = 419)
| Variable | n (%) | Mean; SD |
|---|---|---|
| Mother age (years) | ||
| ≤ 23 | 110 (26.3) |
29.44; 6.84 |
| 24–31 | 154 (36.8) | |
| 32–39 | 118 (28.1) | |
| ≥40 | 37 (8.8) | |
| Education (years) | ||
| ≤6 | 10 (2.4) |
12.06; 2.68 |
| 7–9 | 60 (14.3) | |
| 10–12 | 218 (52) | |
| >12 | 131 (31.3) | |
| Employment status | ||
| Unemployed | 321 (76.6) | – |
| Employed | 98 (23.4) | |
| Adequate financial resources | ||
| No | 323 (77.1) | – |
| Yes | 96 (22.9) | |
| Parity | ||
| First child | 127 (30.3) | – |
| Multiple children | 292 (69.7) | |
| Intention of pregnancy | ||
| Unplanned | 237 (56.6) | – |
| Planned | 182 (43.4) | |
| Previous pregnancy loss or death of an infant | ||
| No | 339 (80.9) | – |
| Yes | 80 (19.1) | |
| Mode of birth | ||
| Normal | 288 (68.7) | – |
| Caesarian | 131 (31.3) | |
| Infant gender | ||
| Male | 180 (43) | – |
| Female | 239 (57) | |
| Mode of feedinga | ||
| Non-exclusive breastfeeding | 304 (72.6) | – |
| Exclusive breastfeeding | 115 (27.4) | |
| Infant ageb | ||
| <3 months | 186 (44.4) | – |
| 3–6 months | 233 (55.6) | |
| Infant mood | ||
| Quiet | 100 (23.9) | – |
| Changeable | 130 (31.0) | |
| Anxious | 189 (45.1) | |
| Infant sleep patternc | ||
| Sleepless night | 105 (25) | – |
| Little sleep | 95 (22.7) | |
| Good sleep | 219 (52.3) | |
Note: aInfant age was calculated in months based on the date of each month following the month the baby was born. bExclusive breastfeeding means that the infant was fed only breast milk with no solids or other oral intake, except vitamins, mineral supplements, or medication. Otherwise, the feeding mode was defined as non-exclusive breastfeeding. cThe infant sleep pattern variable was classified based on the quality of sleep: sleepless night (i.e., if the baby had frequent and prolonged nocturnal awakenings), little sleep (i.e., if the baby had frequent nocturnal awakenings), and good sleep (i.e., if the baby had uninterrupted sleeping at night).
Of the 419 infants born alive, 55.6% were aged between 3 and 6 months, 57% were females, 68.7% were delivered vaginally, and 27.4% were exclusively breastfed. In terms of the newborns’ mood and sleep-wake patterns, the participating mothers stated that 45.1% of the babies had anxious moods, while 52.3% of the infants showed good sleep patterns.
The total scores of the items in each subscale of the MOS-SSS ranged from 4 to 18 points for informational support, from 10 to 26 points for emotional support, and from 8 to 38 points for tangible support. The means and standard deviations of the total scores for the emotional, tangible, and informational subscales were as follows: 9.70 ± 2.84; 18.51 ± 3.85; and 19.52 ± 3.60, respectively.
As per the statistical descriptive analysis of the PSAS, the total scores of the ISWA subscale ranged from 17 to 40 points and 9 to 26 points for the PICA subscale. The means and standard deviations of the total scores for the ISWA and PICA subscales were as follows: 31.32 ± 3.83; and 15.51 ± 3.91, respectively. A numerical summary of the items in each subscale of the PSAS, across the 419 participating women, is shown in Table 3.
Table 3.
Numerical Summary of Anxiety Scores Across the 419 Postpartum Women
| Scale Item | Mean | Standard deviation | Skewness | Kurtosis |
|---|---|---|---|---|
| Infant Safety and Welfare Anxieties | ||||
| I have felt frightened when my baby is not with me | 3.51 | 0.68 | -1.40 | 2.03 |
| I have repeatedly checked on my sleeping baby | 3.49 | 0.65 | -1.35 | 2.28 |
| I have worried that my baby will stop breathing while sleeping | 2.97 | 0.93 | -0.77 | -0.16 |
| I have worried about my baby being accidentally harmed by someone or something else | 2.13 | 0.89 | 0.10 | -1.10 |
| I have worried about leaving my baby in a childcare setting | 2.89 | 0.56 | -0.62 | 2.95 |
| I have worried about accidentally harming my baby | 2.13 | 0.90 | 0.16 | -0.95 |
| I have thought of ways to avoid exposing my baby to germs | 2.99 | 0.50 | -0.14 | 3.32 |
| I have not taken part in an everyday activity with my baby because I fear they may come to harm | 2.72 | 0.72 | -0.04 | -0.33 |
| I have worried about my baby’s health even after reassurance from others | 2.75 | 0.76 | -0.72 | 0.62 |
| I have worried that I will become too ill to care for my baby | 2.82 | 0.45 | -1.04 | 2.88 |
| I have felt a greater need to do things in a certain way or order than before my baby was born | 2.93 | 0.54 | -0.43 | 1.61 |
| Practical Infant Care Anxieties | ||||
| I have worried about my baby’s milk intake | 2.75 | 0.71 | -0.05 | -0.30 |
| I have worried about my baby’s weight | 2.87 | 0.54 | -0.92 | 2.49 |
| I have worried about getting my baby into a routine | 2.75 | 0.71 | -0.05 | -0.30 |
| I have worried about the way that I feed my baby | 1.43 | 0.79 | 1.91 | 2.92 |
| I have worried about the length of time that my baby sleeps | 2.38 | 0.90 | 0.17 | -0.71 |
| I have used the internet for reassurance about my baby’s health | 1.70 | 1.09 | 1.25 | 0.01 |
| I have worried that my baby is not developing as quickly as other babies | 1.62 | 1.02 | 1.43 | 0.62 |
Note: Mothers reported the frequency of experiencing each feeling on a scale ranging from 1 (not at all) to 4 (almost always). Higher scores on each four-point Likert scale item show higher levels of postpartum infant-focused anxieties.
Predictors of the Infant Safety and Welfare Anxieties
As shown in Table 4, the results of the first model identified several significant predictors for postnatal anxiety concerning infant safety and welfare. Our analysis revealed that numerous infant factors were found to be inversely proportional to the ISWA scores. For instance, mothers of exclusively breastfed babies (β = −0.07, p = 0.03) and infants aged 3–6 months (β = −0.08, p = 0.01) had significantly lower levels of perceived ISWAs.
Table 4.
Estimated MLR Coefficients for the Total Scores of Infant Safety and Welfare Anxieties
| Variable | B | Standard error | β | p-Value |
| Sociodemographic Characteristics | ||||
| Mother age in years | 0.02 | 0.02 | 0.03 | .38 |
| Years of education | 0.05 | 0.06 | 0.03 | .43 |
| Employment status: (Unemployed) Employed |
0.09 |
0.34 |
0.01 |
.80 |
| Adequate Financial Resources: (No) Yes |
-0.22 |
0.26 |
-0.02 |
.41 |
| Obstetric Characteristics | ||||
| Parity: (First child) Multiple children |
0.02 |
0.30 |
0.003 |
.94 |
| Intention of pregnancy: (Unplanned) Planned |
-0.09 |
0.24 |
-0.01 |
.72 |
| Previous pregnancy loss or death of an infant: (No) Yes |
0.70 |
0.34 |
0.07 |
.04 |
| Mode of birth: (Normal) Caesarian |
0.30 |
0.23 |
0.04 |
.20 |
| Infant Factors | ||||
| Infant gender: (male) Female |
0.13 |
0.21 |
0.02 |
.54 |
| Mode of feeding: (Non-exclusive breastfeeding) Exclusive breastfeeding |
-0.58 |
0.27 |
-0.07 |
.03 |
| Infant age: (<3 months) 3-6 months |
-0.60 |
0.23 |
-0.08 |
.01 |
| Infant mood: (Quiet) | ||||
| Changeable | 0.64 | 0.29 | 0.08 | .03 |
| Anxious | 1.43 | 0.30 | 0.19 | <.01 |
| Infant sleep pattern: (sleepless night) | ||||
| Little sleep | -0.53 | 0.35 | -0.06 | .13 |
| Good sleep | -0.29 | 0.33 | -0.04 | .39 |
| Social Support Factors | ||||
| Total score of tangible support received from close social networks |
0.04 |
0.04 |
0.06 |
.26 |
| Total score of informational support received from health care providers |
-0.96 |
0.08 |
-0.71 |
<.01 |
| Total score of emotional support received from close social networks |
-0.08 |
0.03 |
-0.08 |
.01 |
| Model summary | ||||
| R Square | .71 | |||
| Adjusted R Square | .70 | |||
Note: The reference category is in parentheses.Abbreviation: MLR, multivariate linear regression
Alternatively, having an infant with a changeable or anxious mood was associated with a higher score of ISWAs (β = 0.08, p = 0.03, and β = 0.19, p < 0.01, respectively). Likewise, a history of difficult emotional experiences, such as a previous miscarriage or the death of an infant, was also found to be a significant predictor correlating with a higher score of ISWAs (β = 0.07, p = 0.04).
The coefficients estimated from the MLR analysis identified two social support aspects as significant protective factors for reducing the levels of perceived ISWAs. In particular, our findings demonstrated that mothers who perceived high levels of informational support from health care providers (β = −0.71, p < 0.01) and emotional support from close social networks (β = −0.08, p = 0.01) had significantly lower levels of PPA concerning infant safety and welfare. In the first model, approximately 71% (r2 = 0.71) of the variation in the response variable (women’s perceived ISWAs) could be explained by the explanatory variables (ie, sociodemographic and obstetric characteristics, infant factors, and social support factors).
Predictors of the Practical Infant Care Anxieties
As the figures in Table 5 show, mothers who were more educated (β = 0.10, p = 0.02), had a cesarean delivery (β = 0.07, p = 0.02), and exclusively breastfed their babies (β = 0.27, p < 0.01) had higher levels of PICAs. A previous pregnancy loss or the death of an infant was also noted as a significant risk factor for increasing the level of PICAs in the second model (β = 0.21, p < 0.01).
Table 5.
Estimated MLR Coefficients for the Total Scores of Practical Infant Care Anxieties
| Variable | B | Standard error | β | p-Value |
| Sociodemographic Characteristics | ||||
| Mother age in years | -0.05 | 0.02 | -0.10 | .01 |
| Years of education | 0.15 | 0.06 | 0.10 | .02 |
| Employment status: (Unemployed) Employed |
-0.67 |
0.37 |
-0.07 |
.07 |
| Adequate Financial Resources: (No) Yes |
0.27 |
0.28 |
0.03 |
.34 |
| Obstetric Characteristics | ||||
| Parity: (First child) Multiple children |
-0.81 |
0.32 |
-0.10 |
.01 |
| Intention of pregnancy: (Unplanned) Planned |
-0.86 |
0.26 |
-0.11 |
<.01 |
| Previous pregnancy loss or death of an infant: (No) Yes |
2.05 |
0.37 |
0.21 |
<.01 |
| Mode of birth: (Normal) Caesarian |
0.57 |
0.25 |
0.07 |
.02 |
| Infant Factors | ||||
| Infant gender: (male) Female |
0.28 |
0.23 |
0.04 |
.22 |
| Mode of feeding: (Non-exclusive breastfeeding) Exclusive breastfeeding |
2.40 |
0.29 |
0.27 |
<.01 |
| Infant age: (<3 months) 3-6 months |
-1.16 |
0.25 |
-0.15 |
<.01 |
| Infant mood: (Quiet) | ||||
| Changeable | 0.01 | 0.32 | 0.001 | .97 |
| Anxious | -0.20 | 0.33 | -0.03 | .55 |
| Infant sleep pattern: (sleepless night) | ||||
| Little sleep | -0.42 | 0.39 | -0.05 | .27 |
| Good sleep | -2.47 | 0.37 | -0.32 | <.01 |
| Social Support Factors | ||||
| Total score of tangible support received from close social networks | 0.09 | 0.04 | 0.13 | .02 |
| Total score of informational support received from health care providers |
-0.28 |
0.09 |
-0.20 |
<.01 |
| Total score of emotional support received from close social networks |
-0.03 |
0.03 |
-0.03 |
.30 |
| Model summary | ||||
| Square | .67 | |||
| Adjusted R Square | .65 | |||
Note: The reference category is in parentheses.Abbreviation: MLR, multivariate linear regression
Conversely, older maternal age (β = −0.10, p = 0.01), being a multiparous mother (β = −0.10, p = 0.01), and having a planned pregnancy (β = −0.11, p < 0.01) were significantly negatively correlated with higher scores of PICAs. Mothers of infants aged 3–6 months (β = −0.15, p < 0.01) and those who had babies with a good sleep pattern (β = −0.32, p < 0.01) were also found to have lower levels of PICAs.
In terms of perceived social support, the results of the MLR analysis in the second model demonstrated that obtaining high informational support from health care providers was significantly associated with a lower level of PPA regarding practical infant care (β = −0.20, p < 0.01). In contrast, receiving high tangible support from close social networks during pregnancy was a significant risk factor for increasing the level of PICAs after delivery (β = 0.13, p = 0.02). In the second model, the explanatory variables (ie, sociodemographic and obstetric characteristics, infant factors, and social support factors) accounted for 67% (r2 = 0.67) of the variation in the response variable (women’s perceived PICAs).
Discussion
Sociodemographic and Obstetric Characteristics
It is widely acknowledged that more educated mothers usually seek to provide their infants with the best maternity practices. This in turn makes them feel more anxious about how they will implement appropriate feeding practices, meet infant nutritional needs, and support an infant’s optimal weight and proper development.35–37 However, being an older mother was found to be a protective factor against developing anxieties related to practical infant care. One possible interpretation is that older women tend to have a better understanding of infant needs, better caregiving experiences, and fewer difficulties in adjusting to new childcare arrangements. This finding is consistent with previous studies demonstrating that postpartum women with higher levels of perceived anxiety were observed to be younger.36,38
In line with the fact that primiparous women face many challenges, including the novelty, uncertainty, and difficulties of being a first-time mother, our study found that the levels of perceived PICAs appeared to be lower among multiparous women. Being unprepared for what motherhood requires may have detrimental effects on women’s ability to perform the new tasks involved in caring for a baby. Consequently, our study emphasizes the need to provide new mothers with knowledge, adequate preparation, and basic skills for infant care to feel more competent in their parental role.
Prior research has reported that one of the most common stressful events that has adverse impacts on women’s emotional health is pregnancy intendedness.39,40 This assertion is supported by our findings, which show that planned pregnancy is a protective factor against anxieties related to practical infant care. Other studies conducted in Jordan also demonstrated that unplanned pregnancies are associated with postnatal depression.41,42 Interestingly, the summary statistics indicate that 56.6% of women had unplanned pregnancies, reflecting gaps in family planning (FP) services in Jordan. The findings of the 2017/2018 Jordanian Population and Family Health Survey demonstrated that 52% of currently married women use a method of FP and that the use of both modern and traditional contraception declined from 42% to 37%, and from 19% to 14% between 2012 and 2017, respectively.40 Accordingly, strengthening the dissemination of knowledge on the advantages of FP and contraceptive use would be an effective approach to promote welfare and stability of Jordanian families.
A woman’s experience around the birth was also found to be related to the PPA, including the mode of delivery. In particular, anxious feelings about practical infant care were observed to be present if a mother had experienced a cesarean delivery. A study by Paul et al10 revealed that mothers delivering via cesarean section (C-section) were significantly more likely to screen positively for PPA compared with those who had vaginal births. Similar findings were also reported elsewhere.37,43 One possible explanation for the association between experiencing a C-section and having a higher level of perceived PICAs is that C-sections can negatively affect breastfeeding initiation, duration, and milk supply. Given that breast milk provides the ideal nutrition for infants, women who suffer from shortened breastfeeding duration, insufficient milk production, or problems with latching and positioning due to C-section deliveries may feel more anxious about their infants’ weight and development.44 This, in turn, may lead to early breastfeeding cessation. According to a study by Hobbs et al,45 higher proportions of women who delivered by planned C-sections had no intention to breastfeed or did not initiate breastfeeding (7.4% and 4.3% respectively), compared to those who delivered vaginally (3.4% and 1.8% respectively). Hobbs et al45 also reported that mothers of babies born via C-section were significantly more likely to discontinue breastfeeding in the first four postpartum months compared to those who had a vaginal delivery.
Not surprisingly, we found that excessive worries about infant health and practical care are a common feature of mothers with previous traumatic life experiences, such as a previous miscarriage or the death of an infant. It is important to note that losing a baby during pregnancy through miscarriage or stillbirth may lead women to be more cautious in protecting their babies from potential harm and providing them with the best maternity care practices. Prior research has reported that miscarriage and fetal death are significant factors in reducing women’s quality of life scores and raising their anxiety level during subsequent pregnancies.46 Studies demonstrated that negative perceptions of the pregnancy experience are associated with the mothers’ excessive involvement in checking behaviors and compulsive cleaning, without aggressive urges to harm the infant.2,46 Researchers have reported that some postpartum women took their infants for frequent medical checkups to be assured that their babies were developing as quickly as others, while others did not allow anyone to hold their infants due to feelings that this would expose the babies to germs or the fear that something bad would happen to the babies.46
Infant Factors
Mothers’ ability to understand the demands of newborns, provide them with appropriate responses, and predict their behaviors improve as the infant age increases. This argument explains our results, which show that the risk of ISWAs and PICAs increased during the first three-month postpartum. In view of that, our study highlights the need for the initial assessment of mothers’ anxiety symptoms as early as possible in the postpartum period. Similar findings were also reported elsewhere.47,48 For instance, in a population-based study of 522 Canadian mothers by Dennis et al,47 anxiety scores declined from 22.6% at one week to 17.2% at four weeks and 14.8% at eight-week postpartum.
We also found that a mother’s ability to overcome anxiety is affected by whether the baby is restless, weepy, or easily irritated and a difficult child. It is widely acknowledged that infant crying is an important signal for their need for safety, protection, and comfort, and accordingly, if this increases, a mother’s worries about infant safety and welfare will increase as well. Evidence suggests that maternal emotional reactions to infant crying range from empathy and sadness, to mild irritation or anxiety, to extreme hostility.49,50 Mothers need to realize that excessive infant crying and irritability might be a response to maternal anxiety, and thus newborns cry presumably because of negative emotions transmitted by their mothers. A study by Leerkes et al50 reported that maternal anxiety in response to crying affects the quality of the parenting they provide during times of infant distress and poses a risk for subsequent attachment insecurities, such as resistant and avoidant behaviors.
A significant link was also noted between exclusive breastfeeding and lower levels of ISWAs among the participating women. It is well known that breastfeeding provides the best nutrition, enhances immune protection, and increases physical growth and mental development for the infant.51 Mothers of exclusively breastfed babies may perceive breastfeeding as essential for better infant health outcomes, which in turn makes them feel less anxious about infant safety and welfare compared to those who use supplemental bottles of formula or stop breastfeeding altogether. This assertion is supported by a large Norwegian study of 42,225 women, wherein breastfeeding cessation was found to be a risk factor for increased PPA and PPD.17 In another context, a systematic review on PPA and breastfeeding has reported that women with a high level of anxiety were less likely to initiate or sustain breastfeeding and more often used bottle-feeding and mixed patterns of breastfeeding.52 Further, anxious mothers had greater breastfeeding difficulties,53 and they were more likely to terminate breastfeeding earlier.52
Contrary to these findings, exclusive breastfeeding was found to be related to higher levels of PICAs. One possible explanation is that if the infant’s predominant source of nutrition is breast milk, then mothers may have worries about the quantity of the milk supply.54 In a study of over 1000 mothers, postpartum women cited many concerns about breastfeeding, including lactation insufficiency, infant nutrition and weight gain, and difficulties with pumping breast milk.55 The lack of women’s knowledge of how infants are supposed to behave when they are hungry and how to know that their babies are getting enough at each feeding has consistently emerged among the most common issues leading to maternal anxiety.
Given that many women realize the impact of good sleeping habits on infant growth and development and how these habits reflect overall health and wellness, mothers of infants with good sleep patterns may feel less anxious compared to those who have poor infant sleep. A growing body of the literature also shows that infants with sleep disruption tend to be more tired, weepy, and irritable, resulting in adverse maternal health outcomes, including mood swings, crying spells, and anxiety.56,57 It is critical for mothers, especially new ones, to recognize that sleep quantity (ie, the number of hours slept) is affected by several factors related to the sleep environment, such as exposure to light and noise, mattress comfort, and room temperature.58 An effective intervention that can assist mothers in managing infant sleep problems is therefore a key component of reducing PPA.
Social Support Factors
Our study suggests that having emotional support at earlier time points (eg, during pregnancy) is a protective factor against developing PPA related to infant welfare and safety among Jordanian women. In prior research, perceptions of concern, care, and love for women during the perinatal period were found to be associated with increased feelings of maternal competence and a reduction in the potentially adverse effects of stressful events (eg, the birth of a new baby).18,59,60 It is common for postpartum mothers to experience feelings of loss of confidence, inadequacy, frustration, or anxiety;58 thus, it matters that they receive emotional support, starting from pregnancy, that makes them feel “safe” in talking openly about their future worries and fears. Active listening, showing affection, and accepting a mother’s feelings within the context of a warm and non-judgmental relationship are considered effective strategies to improve women’s emotional well-being and help achieve subsequent changes in perceived anxiety. More appreciation is therefore required for the role of receiving continuous and regular informal support in creating a health-promoting environment for pregnant women. This has a key implication for practice and service development in that the mothers’ normal social circle needs to be targeted. Establishing education programs that aim at enhancing the role of social support in the perinatal period may be a preferred action to empower women to cope effectively with PPA.
As social support is a multidimensional construct, our study pointed out that tangible support has less of a role in mitigating women’s feelings of anxiety about practical infant care. Although many Jordanian women continued to rely on their closed social networks for tangible support, others recognize receiving more support than desired as being potentially worse than receiving little or no support. For instance, providing women with unwanted help or taking on most or all of their responsibilities may act as stressors for a segment of women, wherein they consider such support as an invasion of their personal lives.61 A mother’s needs for help depend on the particular individual, and thus each one has a different reaction to the tangible support. In some cases, mothers want to be independent and on their own, with no or little family support, while in other cases they may feel that they do not need any help. In a study by DeVito,62 providing pregnant women with tangible support from their own mothers seemed to undermine their sense of parenting ability and independence. Given that, our study emphasizes the need for close social networks to understand the various ways they can be supportive, and to communicate with women to see what type of support is really needed and when to provide it.
Caregivers in health care institutions can also play a key role in alleviating feelings of anxiety among postpartum women through the provision of information-focused strategies. Low preparedness for the postnatal period, including a lack of reliable and realistic information about infant care and insufficient supports to express feelings of emotional distress, may lead to the development of mood and anxiety disorders.63 It has been observed that pregnant women and providers usually show an additional focus on birth rather than the postpartum period, given that this period is too far removed to be of immediate concern.6 Researchers have reported that the effectiveness of social support depends on the relationship between support givers and receivers,64 and thus ensuring an open and safe environment for sharing the experiences of emotional distress is imperative for connectedness and well-being. The inability of women to express feelings comfortably with health care providers may result from the fear of being perceived as a “bad mother” or as negligent, which may inhibit help-seeking behavior.65,66 A need for more informational support and appropriate advice from health care providers has been identified in several studies as a coping strategy to decrease PPA.63,67,68
Implications for Interventions
The significant relationship between previous informational support received and perceptions of anxieties in the early postpartum period highlights the importance of health care providers’ role in reducing the effects of infant care stressors. Educating pregnant mothers regarding infant safety and practical care needs to be incorporated into routine practice during antenatal visits. The opportunity for open discussion, along with increased awareness and clarification of common misconceptions about infant care, is necessary. Steps should be taken within health care organizations to assess the informational needs of pregnant mothers continuously, even by well-trained non-specialist health providers.
Mothers’ concerns about the amount of milk that their babies need and whether the baby is growing enough are among the most common reasons that may lead mothers to feel anxious.54 Establishing “baby-training” programs and educating Jordanian mothers about how a normal breastfed infant behaves, and what the typical mood and sleep-wake patterns of a newborn are really like, are considered essential components of a successful strategy for improving mothers’ childbirth experiences. The lack of availability of qualified and competent breastfeeding support often causes mothers to perceive insufficient milk and start unnecessary supplementation, which may then be followed by a real decrease in milk production. Without being taught about how long a normal baby can go between feedings and the length of time a healthy baby sleeps, mothers may perceive problems that are not present. Incomplete or absent education about normal infant behaviors may contribute to worsening the woman’s psychological state, especially if she is anxious about her ability to care for the infant. In Jordan, health care providers need to ensure effective breastfeeding support for women before their babies are born. Prenatal breastfeeding classes should teach mothers how to obtain consistent help, recognize when breastfeeding is going well, and identify what to do if they have actual lactation problems. Such classes can make a huge difference in improving infant care, especially if a woman’s worries are the result of inaccurate information about normal newborn behavior. Posting informational videos on hospital websites about infant feeding, care of the infant, and the necessity for postpartum follow-up may assist in preventing the incidence of new cases of PPA.
In Jordan, screening for anxiety disorders is not routinely implemented as a part of postpartum care. This paper suggests developing early targeted interventions aimed at emphasizing the role of health care providers in addressing psychological problems that affect new mothers and solving issues related to under-detection and poor management of PPA. Raising women’s awareness about the importance of seeking appropriate care, either at a primary care level or through timely referral to obstetrical mental health professionals, is also beneficial. Nurses and childbirth educators are in a prominent position to screen postpartum women against the symptoms of anxiety and ensure appropriate referral sources. The nurse should assess the mother’s worries about infant care during the prenatal and postnatal periods to dispel the numerous fears and misconceptions surrounding the care of a new baby. For instance, nurses should ask mothers if they have ever had mental health problems in the past and whether they have been bothered lately by feelings of dread, anxiety, or repetitive behaviors. The collaboration between mothers and health caregivers would contribute to building maternal confidence, removing feelings of stress and anxiety, and consequently improving neonatal and maternal emotional well-being.
Assessing women’s social circumstances and life events experienced during pregnancy can help in understanding the interaction between emotional health and receiving social support. Collecting information about what sort of social support is required, who best provides the support, and when support is most useful is needed to identify potentially modifiable risk factors for PPA and build an evidence base for newly developed social support interventions.
More targeted interventions toward promoting FP education and increasing the use of effective contraceptives need to be an integrated part of the characteristics of FP services. Whenever appropriate, health care providers need to explain the benefits of birth spacing and encourage the adoption of modern contraceptives associated with the lowest probability of discontinuation (eg, intrauterine contraceptive device).
One possible strategy that health care providers should consider is to target women planning C-section deliveries. Mothers delivering via C-section require additional lactation consultation and other breastfeeding supports in the early postpartum period. Such supports could be made available immediately after childbirth (ie, within one-hour post-delivery). Ensuring successful breastfeeding within the first 24 hours is highly recommended by the WHO Baby-Friendly Hospital Initiative as an effective intervention for long-term breastfeeding success.45 Encouraging women to attend postnatal care visits presents an important chance to focus on the physical aspects of care, including conducting breastfeeding assessments and providing much-needed support to overcome any lactation difficulties.
Strengths and Limitations
A major strength of our research is that, to the best of our knowledge, this is the first study exploring the relationship between perceived social support during pregnancy and the feelings of PPA using an anxiety-specific screening instrument. The use of such a tool may help predict postnatal outcomes more effectively than general measures do. Importantly, there is a current lack of longitudinal studies beyond the early postpartum period examining whether perceived social support in the prenatal period is associated with lower levels of anxiety following childbirth. Because of this, our longitudinal observational study design is robust in predicting the correlation between receiving social support at earlier time points (eg, during pregnancy) and the development of anxiety over time (ie, after delivery).
Another strength of this study was its targeting of several types of social support, including informational support delivered by health care providers. Including this type of support in our study represents an opportunity to find areas that can be improved by policy formulation and implementation, unlike women’s sociodemographic and obstetric characteristics, which are difficult to alter.
Some limitations of the study should be acknowledged. First, we evaluated PPA using a self-administered PSAS questionnaire; therefore, future longitudinal studies using a rigorous diagnostic clinical tool are needed to confirm the state of anxiety throughout the postpartum period. Another limitation is that the study sample was recruited from obstetrical and gynecological clinics at one university hospital, which may limit the generalizability of our results in the community-based postpartum population. Additionally, the impact of perceived social support on infant-focused anxieties was assessed among postpartum women residing in northern Jordan, which does not allow generalizability to the greater Jordanian population or women in other countries. There is consequently a need to broaden the study of PPA to include a more diverse sample. Future qualitative studies of women’s experiences are also essential for the effective recognition of PPA. Further analysis needs to take into consideration some confounding factors related to the obstetric characteristics, including the complications during labor and delivery.
Conclusion
Our findings provide an evidence that receiving social supports during pregnancy is significantly associated with postpartum women’s mental health. The usual management of PPA related to caring for an infant may not be effective if different types of social supports are not addressed. Coordinated and integrated prenatal care that considers the “right time and the right type” of support that may be of particular importance may lead to improvements in women’s emotional well-being following childbirth. Assessing how pregnant women perceive their level of support may prove valuable in identifying specific indicators toward developing anxiety symptoms in the postnatal period. The lack of several types of social support is a potentially modifiable risk factor, and thus conducting an adequate assessment of the postpartum mother’s social situation may be most effective if conducted at preceding points (ie, during pregnancy). A need for increased informational support to be provided by professionals has been identified in the current research as an effective strategy for reducing ISWAs as well as PICAs. Supporting and reassuring women by informal talk therapies in which they do not feel judged by health care providers is expected to be vitally important in understanding what mothers may be experiencing and, as a result, helping them deal with feelings of anxiety. Implementing psychosocial interventions that involve important sources of emotional support are promising strategies that may help prevent the incidence of new cases of anxiety disorders among postpartum women. Our research also suggests that increasing the quantity of tangible support may have the potential to negatively influence maternal psychological well-being, and thus, building bridges between women, their families, and providers serves as a preferred action to distinguish the specific type and amount of support that should be provided to mothers during pregnancy.
Acknowledgments
We are extremely grateful to all women for their willingness to participate in this study. Special thanks is directed to the deanship of research at Jordan University of Science and Technology in providing funding and support.
Funding Statement
The research was supported by grant number 20160089 from the Deanship of Research at Jordan University of Science and Technology, Irbid, Jordan. The funder had no role in designing the study; in collecting, analyzing, and interpreting data; or in preparing and writing the manuscript.
Abbreviations
C-sections, cesarean sections; CVR, content validation ratio; FP, Family Planning; ISWAs, Infant Safety and Welfare Anxieties; KAUH, King Abdullah University Hospital; KMO, Kaiser-Meyer-Olkin; MLR, Multivariate Linear Regression; MOS-SSS, Medical Outcomes Study Social Support Survey; PICAs, Practical Infant Care Anxieties; PPA, Postpartum Anxiety; PPD, Postpartum Depression; PSAS, Postpartum Specific Anxiety Scale; SPSS, Statistical Package for the Social Sciences; WHO, World Health Organization.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval for the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
- 1.Leight KL, Fitelson EM, Weston CA, Wisner KL. Childbirth and mental disorders. Int Rev Psychiatry. 2010;22(5):453–471. doi: 10.3109/09540261.2010.514600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ali E. Women experiences with postpartum anxiety disorders: a narrative literature review. Int J Womens Health. 2018;10:237–249. doi: 10.2147/IJWH.S158621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fallon V, Halford JCG, Bennett KM, Harrold JA. The Postpartum Specific Anxiety Scale: development and preliminary validation. Arch Womens Ment Health. 2016;19(6):1079–1090. doi: 10.1007/s00737-016-0658-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fairbrother N, Janssen P, Antony MM, Tucker E, Young AH. Perinatal anxiety disorder prevalence and incidence. J Affect Disord. 2016;200:148–155. doi: 10.1016/j.jad.2015.12.082 [DOI] [PubMed] [Google Scholar]
- 5.Martini J, Petzoldt J, Einsle F, Beesdo-Baum K, Höfler M, Wittchen H-U. Risk factors and course patterns of anxiety and depressive disorders during pregnancy and after delivery: a prospective-longitudinal study. J Affect Disord. 2015;175:385–395. doi: 10.1016/j.jad.2015.01.012 [DOI] [PubMed] [Google Scholar]
- 6.Razurel C, Bruchon-Schweitzer M, Dupanloup A, Irion O, Epiney M. Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery. 2011;27(2):237–242. doi: 10.1016/j.midw.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 7.Highet N, Stevenson AL, Purtell C, Coo S. Qualitative insights into women’s personal experiences of perinatal depression and anxiety. Women Birth. 2014;27(3):179–184. doi: 10.1016/j.wombi.2014.05.003 [DOI] [PubMed] [Google Scholar]
- 8.Corrigan CP, Kwasky AN, Groh CJ. Social support, postpartum depression, and professional assistance: a survey of mothers in the Midwestern United States. J Perinat Educ. 2015;24(1):48–60. doi: 10.1891/1058-1243.24.1.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fallon V, Davies SM, Silverio SA, Jackson L, De Pascalis L, Harrold JA. Psychosocial experiences of postnatal women during the COVID-19 pandemic. A UK-wide study of prevalence rates and risk factors for clinically relevant depression and anxiety. J Psychiatr Res. 2021;136:157–166. doi: 10.1016/j.jpsychires.2021.01.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paul IM, Downs DS, Schaefer EW, Beiler JS, Weisman CS. Postpartum anxiety and maternal-infant health outcomes. Pediatrics. 2013;131(4):e1218–e1224. doi: 10.1542/peds.2012-2147 [DOI] [PubMed] [Google Scholar]
- 11.Brockington IF, Macdonald E, Wainscott G. Anxiety, obsessions and morbid preoccupations in pregnancy and the puerperium. Arch Womens Ment Health. 2006;9(5):253–263. doi: 10.1007/s00737-006-0134-z [DOI] [PubMed] [Google Scholar]
- 12.Romano M, Cacciatore A, Giordano R, La Rosa B. Postpartum period: three distinct but continuous phases. J Prenat Med. 2010;4(2):22–25. [PMC free article] [PubMed] [Google Scholar]
- 13.Manurung S, Setyowati S. Development and validation of the maternal blues scale through bonding attachments in predicting postpartum blues. Malays Fam Physician. 2021;16(1):64–74. doi: 10.51866/oa1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davies SM, Silverio SA, Christiansen P, Fallon V. Maternal-infant bonding and perceptions of infant temperament: the mediating role of maternal mental health. J Affect Disord. 2021;282:1323–1329. doi: 10.1016/j.jad.2021.01.023 [DOI] [PubMed] [Google Scholar]
- 15.Schwab-Reese LM, Schafer EJ, Ashida S. Associations of social support and stress with postpartum maternal mental health symptoms: main effects, moderation, and mediation. Women Health. 2017;57(6):723–740. doi: 10.1080/03630242.2016.1181140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morikawa M, Okada T, Ando M, et al. Relationship between social support during pregnancy and postpartum depressive state: a prospective cohort study. Sci Rep. 2015;5(1):10520. doi: 10.1038/srep10520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ystrom E. Breastfeeding cessation and symptoms of anxiety and depression: a longitudinal cohort study. BMC Pregnancy Childbirth. 2012;12(1):36. doi: 10.1186/1471-2393-12-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stapleton LRT, Schetter CD, Westling E, et al. Perceived partner support in pregnancy predicts lower maternal and infant distress. J Fam Psychol. 2012;26(3):453–463. doi: 10.1037/a0028332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abramowitz JS, Meltzer-Brody S, Leserman J, et al. Obsessional thoughts and compulsive behaviors in a sample of women with postpartum mood symptoms. Arch Womens Ment Health. 2010;13(6):523–530. doi: 10.1007/s00737-010-0172-4 [DOI] [PubMed] [Google Scholar]
- 20.Wongpakaran T, Wongpakaran N, Ruktrakul R. Reliability and validity of the Multidimensional Scale of Perceived Social Support (MSPSS): Thai version. Clin Pract Epidemiol Ment Health. 2011;7(1):161–166. doi: 10.2174/1745017901107010161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified medical outcomes study social support survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–1116. doi: 10.1016/j.jclinepi.2012.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sedigheh A, Keramat A. The relationship between perceived social support from family and postpartum empowerment with maternal wellbeing in the postpartum period. J Midwifery Reprod Health. 2016;4(4):779–787. doi: 10.22038/jmrh.2016.7612 [DOI] [Google Scholar]
- 23.Gan Y, Xiong R, Song J, et al. The effect of perceived social support during early pregnancy on depressive symptoms at 6 weeks postpartum: a prospective study. BMC Psychiatry. 2019;19(1):232. doi: 10.1186/s12888-019-2188-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siedlecki KL, Salthouse TA, Oishi S, Jeswani S. The relationship between social support and subjective well-being across age. Soc Indic Res. 2014;117(2):561–576. doi: 10.1007/s11205-013-0361-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phoosuwan N, Manasatchakun P, Eriksson L, Lundberg PC. Life situation and support during pregnancy among Thai expectant mothers with depressive symptoms and their partners: a qualitative study. BMC Pregnancy Childbirth. 2020;20(1):207. doi: 10.1186/s12884-020-02914-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- 27.Karmaus W, Soto-Ramírez N, Zhang H. Infant feeding pattern in the first six months of age in USA: a follow-up study. Int Breastfeed J. 2017;12(1):48. doi: 10.1186/s13006-017-0139-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zanini DS, Peixoto EM, Nakano TC. The Social Support Scale (MOS-SSS): standardizing with item references. Temas Em Psicol. 2018;26(1):401–412. doi: 10.9788/TP2018.1-15En [DOI] [Google Scholar]
- 29.Griep RH, Chor D, Faerstein E, Werneck GL, Lopes CS. Construct validity of the medical outcomes study’s social support scale adapted to Portuguese in the Pró-Saúde Study. Cad Saude Publica. 2005;21(3):703–714. doi: 10.1590/S0102-311X2005000300004 [DOI] [PubMed] [Google Scholar]
- 30.Zanini DS, Peixoto EM. Social Support Scale (MOS-SSS): analysis of the psychometric properties via item response theory. Paid Ribeirão Preto. 2016;26(65):359–368. doi: 10.1590/1982-43272665201612 [DOI] [Google Scholar]
- 31.Hair J, Black W, Babin B and Anderson R. (2010) Multivariate Data Analysis: A Global Perspective. 7th Edition, Pearson Education, Upper Saddle River. [Google Scholar]
- 32.Silverio SA, Davies SM, Christiansen P, et al. A validation of the postpartum specific anxiety scale 12-item research short-form for use during global crises with five translations. BMC Pregnancy Childbirth. 2021;21(1):112. doi: 10.1186/s12884-021-03597-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Infante‐Gil L, Silverio SA, Fallon V, Wendland J. Postpartum specific anxiety in a French population: validation of the French version of the Postpartum Specific Anxiety Scale [PSAS‐FR]. Perspect Psychiatr Care. 2021;ppc.12808. doi: 10.1111/ppc.12808 [DOI] [PubMed] [Google Scholar]
- 34.Duran S. Postpartum Specific Anxiety Scale (PSAS): reliability and validity of the Turkish version. Perspect Psychiatr Care. 2020;56(1):95–101. doi: 10.1111/ppc.12385 [DOI] [PubMed] [Google Scholar]
- 35.Wassif OM, Abdo AS, Elawady MA, Abd Elmaksoud AE, Eldesouky R. Assessment of postpartum depression and anxiety among females attending primary health care facilities in Qaliubeya Governorate, Egypt. J Environ Public Health. 2019;2019:1–9. doi: 10.1155/2019/3691752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bener A, Sheikh J, Gerber L. Prevalence of psychiatric disorders and associated risk factors in women during their postpartum period: a major public health problem and global comparison. Int J Womens Health. 2012;4:191. doi: 10.2147/IJWH.S29380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Field T. Postnatal anxiety prevalence, predictors and effects on development: a narrative review. Infant Behav Dev. 2018;51:24–32. doi: 10.1016/j.infbeh.2018.02.005 [DOI] [PubMed] [Google Scholar]
- 38.Lau Y, Yin L. Maternal, obstetric variables, perceived stress and health-related quality of life among pregnant women in Macao, China. Midwifery. 2011;27(5):668–673. doi: 10.1016/j.midw.2010.02.008 [DOI] [PubMed] [Google Scholar]
- 39.Hijazi HH, Alyahya MS, Sindiani AM, Saqan RS, Okour AM. Determinants of antenatal care attendance among women residing in highly disadvantaged communities in northern Jordan: a cross-sectional study. Reprod Health. 2018;15(1):106. doi: 10.1186/s12978-018-0542-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alyahya MS, Hijazi HH, Alshraideh HA, et al. Do modern family planning methods impact women’s quality of life? Jordanian women’s perspective. Health Qual Life Outcomes. 2019;17(1):154. doi: 10.1186/s12955-019-1226-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mohammad KI, Gamble J, Creedy DK. Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery. 2011;27(6):e238–e245. doi: 10.1016/j.midw.2010.10.008 [DOI] [PubMed] [Google Scholar]
- 42.Taybeh EO. A focus on postpartum depression among Jordanian mothers. Int J Soc Psychiatry. 2021:002076402110001. doi: 10.1177/00207640211000100 [DOI] [PubMed] [Google Scholar]
- 43.Clout D, Brown R. Sociodemographic, pregnancy, obstetric, and postnatal predictors of postpartum stress, anxiety and depression in new mothers. J Affect Disord. 2015;188:60–67. doi: 10.1016/j.jad.2015.08.054 [DOI] [PubMed] [Google Scholar]
- 44.Brown A, Jordan S. Impact of birth complications on breastfeeding duration: an internet survey. J Adv Nurs. 2013;69(4):828–839. doi: 10.1111/j.1365-2648.2012.06067.x [DOI] [PubMed] [Google Scholar]
- 45.Hobbs AJ, Mannion CA, McDonald SW, Brockway M, Tough SC. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth. 2016;16(1):90. doi: 10.1186/s12884-016-0876-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.House SJ, Tripathi SP, Knight BT, Morris N, Newport DJ, Stowe ZN. Obsessive-compulsive disorder in pregnancy and the postpartum period: course of illness and obstetrical outcome. Arch Womens Ment Health. 2016;19(1):3–10. doi: 10.1007/s00737-015-0542-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dennis C-L, Coghlan M, Vigod S. Can we identify mothers at-risk for postpartum anxiety in the immediate postpartum period using the state-trait anxiety inventory? J Affect Disord. 2013;150(3):1217–1220. doi: 10.1016/j.jad.2013.05.049 [DOI] [PubMed] [Google Scholar]
- 48.Vismara L, Rollè L, Agostini F, et al. Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: a 3- to 6-months postpartum follow-up study. Front Psychol. 2016;7. doi: 10.3389/fpsyg.2016.00938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Del Vecchio T, Walter A, O’Leary SG. Affective and physiological factors predicting maternal response to infant crying. Infant Behav Dev. 2009;32(1):117–122. doi: 10.1016/j.infbeh.2008.10.005 [DOI] [PubMed] [Google Scholar]
- 50.Leerkes EM, Parade SH, Gudmundson JA. Mothers’ emotional reactions to crying pose risk for subsequent attachment insecurity. J Fam Psychol. 2011;25(5):635–643. doi: 10.1037/a0023654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dieterich CM, Felice JP, O’Sullivan E, Rasmussen KM. Breastfeeding and health outcomes for the mother-infant dyad. Pediatr Clin North Am. 2013;60(1):31–48. doi: 10.1016/j.pcl.2012.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fallon V, Groves R, Halford JCG, Bennett KM, Harrold JA. Postpartum anxiety and infant-feeding outcomes: a systematic review. J Hum Lact. 2016;32(4):740–758. doi: 10.1177/0890334416662241 [DOI] [PubMed] [Google Scholar]
- 53.Fallon V, Halford JCG, Bennett KM, Harrold JA. Postpartum-specific anxiety as a predictor of infant-feeding outcomes and perceptions of infant-feeding behaviours: new evidence for childbearing specific measures of mood. Arch Womens Ment Health. 2017:21(2):181–191. doi: 10.1007/s00737-017-0775-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Davie P, Chilcot J, Jones L, Bick D, Silverio SA. Indicators of ‘good’ feeding, breastfeeding latch, and feeding experiences among healthy women with healthy infants: a qualitative pathway analysis using grounded theory. Women Birth. 2021;34(4):e357–e367. doi: 10.1016/j.wombi.2020.08.004 [DOI] [PubMed] [Google Scholar]
- 55.Odom EC, Li R, Scanlon KS, Perrine CG, Grummer-Strawn L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics. 2013;131(3):e726–e732. doi: 10.1542/peds.2012-1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tham E, Schneider N, Broekman B. Infant sleep and its relation with cognition and growth: a narrative review. Nat Sci Sleep. 2017;9:135–149. doi: 10.2147/NSS.S125992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Symon B, Bammann M, Crichton G, Lowings C, Tucsok J. Reducing postnatal depression, anxiety and stress using an infant sleep intervention. BMJ Open. 2012;2(5):e001662. doi: 10.1136/bmjopen-2012-001662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Doering JJ. The physical and social environment of sleep in socioeconomically disadvantaged postpartum women. J Obstet Gynecol Neonatal Nurs. 2013;42(1):E33–E43. doi: 10.1111/j.1552-6909.2012.01421.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Navarrete LE, Lara-Cantú MA, Navarro C, Gómez ME, Morales F. Psychosocial factors predicting postnatal anxiety symptoms and their relation to symptoms of postpartum depression. Rev Investig Clin Organo Hosp Enfermedades Nutr. 2012;64(6 Pt 2):625–633. [PubMed] [Google Scholar]
- 60.Ponomartchouk D, Bouchard G. New mothers’ sense of competence: predictors and outcomes. J Child Fam Stud. 2015;24(7):1977–1986. doi: 10.1007/s10826-014-9997-1 [DOI] [Google Scholar]
- 61.Brock RL, Lawrence E. Too much of a good thing: underprovision versus overprovision of partner support. J Fam Psychol. 2009;23(2):181–192. doi: 10.1037/a0015402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.DeVito J. How adolescent mothers feel about becoming a parent. J Perinat Educ. 2010;19(2):25–34. doi: 10.1624/105812410X495523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Slomian J, Emonts P, Vigneron L, et al. Identifying maternal needs following childbirth: a qualitative study among mothers, fathers and professionals. BMC Pregnancy Childbirth. 2017;17(1):213. doi: 10.1186/s12884-017-1398-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.De Sousa Machado T, Chur-Hansen A, Due C. First-time mothers’ perceptions of social support: recommendations for best practice. Health Psychol Open. 2020;7(1):205510291989861. doi: 10.1177/2055102919898611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Law KH, Jackson B, Guelfi K, Nguyen T, Dimmock JA. Understanding and alleviating maternal postpartum distress: perspectives from first-time mothers in Australia. Soc Sci Med. 2018;204:59–66. doi: 10.1016/j.socscimed.2018.03.022 [DOI] [PubMed] [Google Scholar]
- 66.Negron R, Martin A, Almog M, Balbierz A, Howell EA. Social support during the postpartum period: mothers’ views on needs, expectations, and mobilization of support. Matern Child Health J. 2013;17(4):616–623. doi: 10.1007/s10995-012-1037-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Manuel JI, Martinson ML, Bledsoe-Mansori SE, Bellamy JL. The influence of stress and social support on depressive symptoms in mothers with young children. Soc Sci Med. 2012;75(11):2013–2020. doi: 10.1016/j.socscimed.2012.07.034 [DOI] [PubMed] [Google Scholar]
- 68.Razurel C, Kaiser B. The role of satisfaction with social support on the psychological health of primiparous mothers in the perinatal period. Women Health. 2015;55(2):167–186. doi: 10.1080/03630242.2014.979969 [DOI] [PubMed] [Google Scholar]