Abstract
Background:
A tiered trauma team activation (TTA) system aims to allocate resources proportional to the patient’s need based upon injury burden. The current metrics used to evaluate appropriateness of TTA are the trauma triage matrix (TTM), need for trauma intervention (NFTI), and secondary triage assessment tool (STAT).
Materials and methods:
In this retrospective study, we compared the effectiveness of the need for an emergent intervention within 6 h (NEI-6) with existing definitions. Data from the Michigan Trauma Quality Improvement Program was utilized. The dataset contains information from 31 level 1 and 2 trauma centers from 2011 to 2017. Inclusion criteria were: adult patients (≥16 y) and ISS ≥5.
Results:
73,818 patients were included in the study. Thirty percentage of trauma patients met criteria for STAT, 21% for NFTI, 20% for TTM, and 13% for NEI-6. NEI-6 was associated with the lowest rate of undertriage at 6.5% (STAT 22.3%, NFTI 14.0%, TTM 14.3%). NEI-6 best predicted undertriage mortality, early mortality, in-hospital mortality, and late (>60 h) mortality. Most patients who met criteria for TTM (58%), NFTI (51%), and STAT (62%) did not require emergent intervention. All four methods had similar rates of early mortality for patients who did not meet criteria (0.3%-0.5%).
Conclusions:
NEI-6 performs better than TTM, NFTI, and STAT in terms of undertriage, mortality and need for resource utilization. Other methods resulted in significantly more full TTAs than NEI-6 without identifying patients at risk for early mortality. NEI-6 represents a novel tool to determine trauma activation appropriateness.
Keywords: Activation, Trauma, Triage, Matrix, Emergent, Intervention, Undertriage, Overtriage
Introduction
The goal of trauma team activation (TTA) guidelines is to match the severity of traumatic injury with the appropriate resources needed to treat the patient’s injuries. There is a current lack of consensus as to which patients require a full TTA. In 2010, the Eastern Association for the Surgery of Trauma (EAST) Practice Management Group attempted to answer this question.1 Due to a paucity of high-quality studies, they were unable to provide any level 1 or 2 recommendations.
There is widespread agreement that the current definition of the patient requiring a full trauma activation based on the Cribari matrix defined by Injury Severity Score (ISS) ≥ 15,2 or trauma triage matrix (TTM), suffers from significant limitations. A commonly cited limitation includes the retrospective nature of the ISS (which is typically not available for weeks to months after a patient’s injury), restricting its utility in the prehospital or Emergency Department (ED) setting when determining the need for TTA.3 Multiple other weaknesses exist. The ISS is anatomically based, fails to account for physiologic status, and equally weighs high-grade head and extremity injuries. It is important to point out that the ISS cutoff of ≥ 154,5 is associated with an in-hospital trauma mortality of >10%, and despite much controversy, this definition has persisted since the 1980s. Significant limitations exist with this approach. For example, a patient with hypotension and a grade 3 splenic injury would only receive an ISS of 9; however, the patient clearly benefits from a full TTA, blood transfusion, and an emergent operation.
Given these concerns, the need for trauma intervention (NFTI) and the secondary triage assessment tool (STAT) has recently been proposed to measure TTA appropriateness.6,7 Both definitions suffer from limitations. STAT includes the union of NFTI and TTM and thus suffers from all the same limitations of TTM. NFTI contains only three elements reflecting rapid need for intervention. Furthermore, patients that die within 60 h of admission or require mechanical ventilation within 3 d of admission are included in NFTI. However, there are many subacute disease processes where patients may require mechanical ventilation within 3 d of admission (i.e., trauma patient with multiple rib fractures), which are unlikely to derive additional benefit from the rapid resource utilization employed during a full TTA. Delivering medical resources to patients that are unlikely to need them results in overtriage, trauma activation fatigue, and resource utilization.
Our group recently identified a high association between the American College of Surgeons (ACS) Committee on Trauma (CoT) mandatory minimum full TTA criteria, mortality, and the need for emergent intervention within 6 h (NEI-6).8 Any criteria for trauma activation appropriateness must account for the need for emergent interventions as the rapid delivery of medical resources is the primary benefit facilitated by a full TTA.9
The hypothesis of this study is that trauma activation appropriateness based on emergent interventions, NEI-6, would be associated with less undertriage when compared with existing definitions for trauma activation appropriateness (TTM, NFTI, and STAT) without impacting mortality.
Materials and methods
Data collection
The Michigan Trauma Quality Improvement Program (MTQIP) is a collaborative quality initiative comprised of 31 ACS-COT verified level 1 and 2 trauma centers in the states of Michigan and Minnesota. MTQIP utilizes a data definitions dictionary, based upon the National Trauma Data Standard (NTDS), which is published online and updated annually.10,11 Trauma data abstractors from participating hospitals undergo training in MTQIP and NTDS data definitions. Data is transmitted from the trauma registry at participating hospitals to the coordinating center at 2-mo intervals. The MTQIP database, instead of the National Trauma Data Bank (NTDB) or American College of Surgeons Trauma Quality Improvement Program (ACS-TQIP), was utilized in this study as MTQIP includes patient TTA level. The inclusion criteria applied to form the MTQIP patient cohort are as follows (Fig. 1):
Fig –
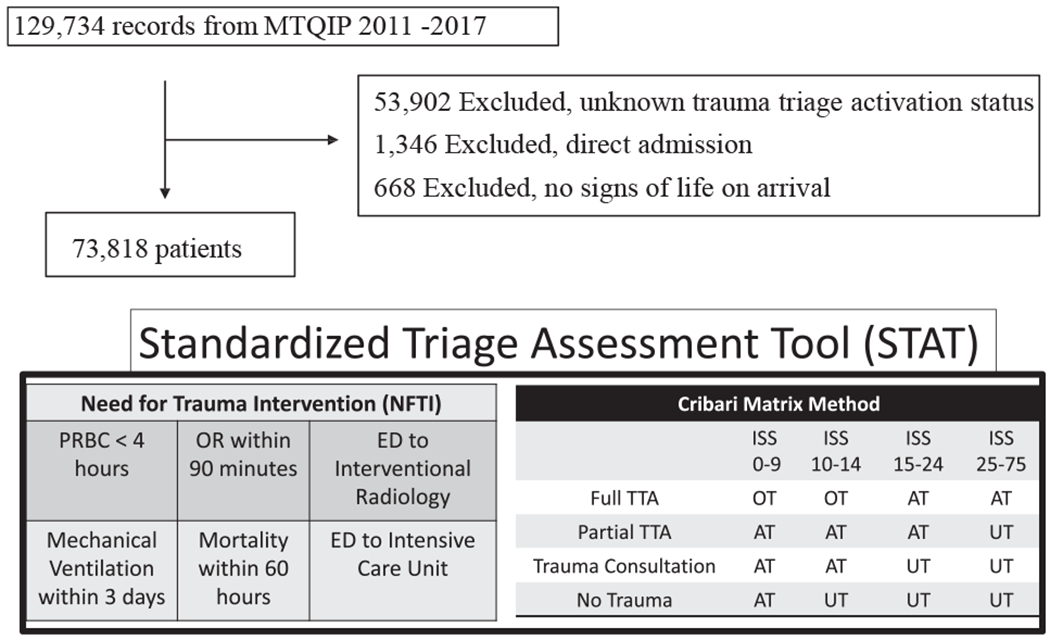
Criteria for trauma activation by method. TTA = trauma team activation; PRBC = packed red blood cells; OR = operating room; ED = emergency department; OT = overtriage; UT = undertriage, AP = appropriate triage.
Age ≥ 16 y
ISS ≥ 5
Primary mechanism of injury classified as either blunt or penetrating:
Blunt was defined as an injury where the primary ICD-9 External Cause Code (E–code) is mapped to the following categories: fall, machinery, motor vehicle traffic, pedestrian, cyclist, and struck by against.
Penetrating was defined as an injury where the primary E-code is mapped to the following categories: cut/pierce and firearm.
All ISS values were derived from registrar abstracted and recorded Abbreviated Injury Scale 2005 codes with 2008 updates (AIS 2005).
Patients directly admitted, missing data, or with no signs of life were excluded.12 After these exclusion criteria, there was an overall low level of missing data elements (<8%).13,14
Trauma triage appropriateness was analyzed based on method. NEI-6 was defined as: receiving ≥5 units of packed red blood cells within the first 4 h, any operation, angiography, chest tube, central line placement, or brain intervention (e.g., placement of an intracranial pressure monitor, craniotomy, etc.) within 6 h of arrival or emergent prehospital or trauma bay intubation. TTM major trauma was defined as: patients with an ISS ≥15 requiring a full TTA.4 NFTI was defined as: receiving ≥5 units of packed red blood cells within the first 4 h, any operation, angiography, chest tube, or central line placement within 6 h of arrival, emergent intubation, or placement of an intracranial pressure monitor.7 The STAT method combined the TTM with NFTI.6
Early mortality was defined as any death occurring within 48 h of ED arrival. Late mortality was defined as any death occurring after 60 h of ED arrival. Undertriage death by TTM included two criteria: (1) Undertriage as defined by ISS ≥15 without a full TTA (2) Inpatient death. For NEI-6, undertriage death was defined as a patient who received an NEI-6 intervention without a full TTA and inpatient death. Major complications were defined as systemic sepsis, pulmonary embolism, pneumonia, acute renal failure, acute respiratory distress syndrome (ARDS), or the presence of a cardiovascular complication (arrest, myocardial infarction, and cerebrovascular accident). These complications were defined as major as they have previously been verified to have the highest attributable mortality among trauma patients.15
Statistical methods
Data were extracted from the MTQIP database. The study cohort consisted of patients admitted to participating trauma centers between 2011 and 2017. Differences in outcomes were explored using univariate analysis. Outcomes of interest included ISS, TTA status, early mortality, in-hospital mortality, late mortality, and undertriage death. Complications were defined based on the MTQIP data dictionary.15,16 Statistical significance was defined as a P-value < 0.05, all tests were two-tailed. Data are expressed as the mean ± standard deviation (SD) for normally distributed continuous descriptive variables with a normal distribution, median ± interquartile range (IQR) for continuous descriptive variables with a skewed distribution, and proportions for categorical variables. We performed Student’s t-test to explore differences in the two groups for continuous variables with a normal distribution and Wilcoxon rank-sum test for continuous variables with a skewed distribution. We used Chi-square test to identify differences in outcomes for categorical variables. Logistic regression analysis was used to investigate the association of each method on mortality. Approval for this study was obtained from the University of Minnesota Institutional Review Board (STUDY00001489).
Results
From 2011 to 2017, 73,818 patients were identified at level 1 and 2 trauma centers (Fig. 1). Of these patients, 9436 (13%) had a full activation, 64,382 (87%) had a limited or no activation, and 60,896 met activation criteria by NFTI, NEI-6, STAT, or TTM. The overall rate of mortality for all trauma patients was 4.1%. Patients who were evaluated by the NEI-6 criteria were similarly injured to those evaluated by NFTI, STAT, and TTM with the exception of penetrating injuries, which was higher in the NEI-6 group, and AIS head/neck ≥2, which was higher in the ISS ≥15. Most aberrant ED vitals and Glasgow Coma Scale (GCS) were also similar between groups. Patients who needed an emergent intervention were more likely to be younger, black, tachycardic, and hypotensive. Patients with an ISS ≥15 made up 20% (14,430) of the study population. NFTI positive patients made up 21% (15,402) of the study population. STAT-positive patients made up 29.2% (21,539) of the study population, and 13% (9525) of patients were NEI-6 positive. Despite more abnormal physiologic criteria in NEI-6 group, the median ISS was only 19 (IQR 10.0, 26.0), compared with a median ISS of 21 (IQR 17.0, 26.0) in the TTM group (Table 1).
Table 1 –
Demographics.
| ISS ≥15 | NFTI | STAT | NEI-6 | |
|---|---|---|---|---|
| N | 14,430 (20%) | 15,402 (21%) | 21,539 (29.2%) | 9525 (13%) |
| Age, median (IQR) | 54 (33, 72) | 54 (33, 74) | 55 (34, 74) | 50 (29, 65) |
| Private insurance | 7069 (49.0%) | 6953 (45.1%) | 9856 (45.8%) | 4597 (48.3%) |
| Race | ||||
| White | 11,310 (78.4%) | 11,860 (77.0%) | 16,852 (78.2%) | 6886 (72.3%) |
| Black | 2494 (17.3%) | 2946 (19.1%) | 3815 (17.7%) | 2235 (23.5%) |
| Other | 626 (4.3%) | 596 (3.9%) | 872 (4.0%) | 404 (4.2%) |
| Female gender | 4744 (32.9%) | 5098 (33.1%) | 7357 (34.2%) | 2676 (28.1%) |
| SBP, mmHg | ||||
| >90 | 13,101 (90.8%) | 13,807 (89.6%) | 19,692 (91.4%) | 8346 (87.6%) |
| 61-90 | 764 (5.3%) | 960 (6.2%) | 1056 (4.9%) | 721 (7.6%) |
| <61 | 161 (1.1%) | 203 (1.3%) | 209 (1.0%) | 177 (1.9%) |
| Missing | 404 (2.8%) | 432 (2.8%) | 582 (2.7%) | 281 (3.0%) |
| Pulse, BPM | ||||
| 51-120 | 12,480 (86.5%) | 13,124 (85.2%) | 18,834 (87.4%) | 7735 (81.2%) |
| >120 | 1365 (9.5%) | 1658 (10.8%) | 1891 (8.8%) | 1369 (14.4%) |
| ≤50 | 231 (1.6%) | 259 (1.7%) | 303 (1.4%) | 195 (2.0%) |
| Missing | 354 (2.5%) | 361 (2.3%) | 511 (2.4%) | 226 (2.4%) |
| ED GCS, median (IQR) | 15.0 (12.0, 15.0) | 15.0 (10.0, 15.0) | 15.0 (13.0, 15.0) | 14.0 (5.0, 15.0) |
| ISS, median (IQR) | 21.0 (17.0, 26.0) | 17.0 (9.0, 25.0) | 17.0 (11.0, 25.0) | 19.0 (10.0, 26.0) |
| Penetrating mechanism | 1244 (8.6%) | 2005 (13.0%) | 2206 (10.2%) | 1798 (18.9%) |
| AIS Head/Neck ≥ 2 | 8934 (61.9%) | 7085 (46.0%) | 10,644 (49.4%) | 4527 (47.5%) |
| AIS chest ≥ 2 | 5909 (40.9%) | 4766 (30.9%) | 7061 (32.8%) | 3871 (40.6%) |
| AIS abdomen ≥ 2 | 2275 (15.8%) | 1998 (13.0%) | 2674 (12.4%) | 1388 (14.6%) |
| AIS extremity ≥ 2 | 2942 (20.4%) | 3213 (20.9%) | 4360 (20.2%) | 1760 (18.5%) |
SBP = systolic blood pressure; ISS = injury severity score; STAT = secondary triage assessment tool; NFTI = need for trauma intervention; NEI-6 = need for an emergent intervention within 6 h; IQR = interquartile range; BMP = beats per minutes; ED = emergency department; GCS = Glascow Coma Score; AIS = abbreviated injury scale.
We evaluated undertriage, early, in-hospital, and late mortality at initial patient presentation by each activation appropriateness model. This determines if the historic trauma activation was classified as overtriage or undertriage based on TTM, NFTI, STAT, and NEI-6. The NEI-6 system was associated with the highest odds of undertriage death (OR 3.7, CI 3.36-4.11, P < 0.001), early mortality (OR 31.0, CI 27.1-35.3, P < 0.001), in-hospital mortality (OR 15.7, CI 14.5-17.0, P < 0.001), and late mortality (OR 8.5, CI 7.7-9.4, P < 0.001). The NFTI system was less associated with undertriage death (OR 3.15, CI 2.9-3.4, P < 0.001), early mortality (OR 16.1, CI 14.2-18.4, P < 0.001), in-hospital mortality (OR 10.9, CI 10.1-11.8, P < 0.001), and late mortality (OR 7.3, CI 6.6-8.1, P < 0.001). STAT and TTM had even less association with undertriage death, early mortality, in-hospital mortality, and late mortality than NFTI (Table 2).
Table 2 .
NEI-6 associated with mortality.
| Undertriage death |
Early (<48 h) Mortality |
In-hospital mortality |
Late (>60 h) mortality |
|
|---|---|---|---|---|
| OR (95% CI) P | OR (95% CI) P | OR (95% CI) P | OR (95% CI) P | |
| TTM | 1.96 (1.79-2.14) <0.001 | 19.1 (16.7-21.9) <0.001 | 10.3 (9.5-11.2) <0.001 | 6.2 (5.6-6.8) <0.001 |
|
| ||||
| NEI-6 | 3.72 (3.36-4.11) <0.001 | 31.0 (27.1-35.3) <0.001 | 15.7 (14.5-17.0) <0.001 | 8.5 (7.7-9.4) <0.001 |
|
| ||||
| NFTI | 3.15 (2.9-3.4) <0.001 | 16.1 (14.2-18.4)* <0.001 | 10.9 (10.1-11.8)* <0.001 | 7.3 (6.6-28.1) <0.001 |
|
| ||||
| STAT | 2.07 (1.9-2.24) <0.001 | 21.7 (18.3-25.7)* <0.001 | 11.2 (10.2-12.3)* <0.001 | 7.1 (6.4-7.9) <0.001 |
STAT = secondary triage assessment tool; NFTI = need for trauma intervention; NEI-6 = need for an emergent intervention within 6 h; TTM = trauma triage matrix; CI = confidence interval; OR = odds ratio.
Mortality < 60, an element of NFTI excluded from analysis.
Trauma activation appropriateness was then evaluated within MTQIP using each method. During the study period, 9436 (12.8%) received a full TTA. If activation appropriateness were gauged based on TTM, 14.27% of patients would have been deemed an undertriage, compared with 13.98% using NFTI, 22.3% using STAT, and 6.5% using NEI-6. Similarly, using the TTM, 44.5% of patients would have been deemed an overtriage, compared with 32.15% using NFTI, 22.88% using STAT, and 42.23% using NEI-6 (Table 3).
Table 3 –
Undertriage and overtriage by triage method.
| TTM | ISS 0-14 | ISS ≥15 | ||
| Full TTA | 4195 | 5241 | Overtriage | 44.45% |
| Limited or none | 55,193 | 9189 | Undertriage | 14.27% |
| NEI-6 | No NEI-6 | NEI-6 | ||
| Full TTA | 4079 | 5357 | Overtriage | 42.23% |
| Limited or none | 60,214 | 4168 | Undertriage | 6.47% |
| NFTI | No NFTI | NFTI | ||
| Full TTA | 3034 | 6402 | Overtriage | 32.15% |
| Limited or none | 55,382 | 9000 | Undertriage | 13.98% |
| STAT | No STAT | STAT | ||
| Full TTA | 2253 | 7183 | Overtriage | 22.88% |
| Limited or none | 50,026 | 14,356 | Undertriage | 22.30% |
STAT = secondary triage assessment tool; NFTI = need for trauma intervention; NEI-6 = need for an emergent intervention within 6 h; TTM = trauma triage matrix; ISS = injury severity score; TTA = trauma team activation.
To investigate if NEI-6 suffers from poor sensitivity for patients that are more likely to benefit from a full TTA, we investigated the early mortality for patients that did not meet each method’s criteria. Early mortality was similar across all methods. Furthermore, over 50% of TTM-, NFTI-, and STAT-positive patients did not require an emergent intervention suggesting they are unlikely to benefit from a full TTA (Table 4).
Table 4 –
Overtriage without associated mortality benefit.
| N | Emergency intervention |
Early mortality* |
|
|---|---|---|---|
| TTM | 14,430 | 41.73% | 8.04% |
| No TTM | 59,388 | 5.90% | 0.045% |
| NEI-6 | 9525 | N/A | 12.04% |
| No NEI-6 | 64,293 | N/A | 0.44% |
| NFTI | 15,402 | 48.73% | 7.38% |
| No NFTI | 58,416 | 3.46% | 0.50% |
| STAT | 21,539 | 38.10% | 5.93% |
| No STAT | 50,279 | 2.62% | 0.30% |
STAT = secondary triage assessment tool; NFTI = need for trauma intervention; TTM = trauma triage matrix.
Excluded NFTI criteria of mortality within 60 h.
Finally, the association of each NEI-6 element to clinical outcomes was assessed. All of the NEI-6 elements (blood transfusion, operation, angiography, chest tube, central line, TBI intervention, and emergent intubation) were associated with adverse events. For example, blood transfusion and emergent intubation are highly associated with early mortality (OR 31.9, P < 0.001; OR 44.2, P < 0.001), any mortality (OR 19.4, P < 0.001; OR 24.1, P < 0.001), development of a major complication (OR 11.9, P < 0.001; OR 11.5; P < 0.001), and ICU admission (OR 9.6, P < 0.001; OR 19.6, P < 0.001). The presence of any NEI-6 element was associated with a 30.9-fold increased mortality (OR 30.9, P < 0.001) (Table 5).
Table 5 –
NEI-6 components and associated complications.
| NEI-6 element | Early mortality, OR (P-value) | Any mortality, OR (P-value) | Any complication OR (P-value) | Major complication, OR (P-value) | ICU admission, OR (P-value) |
|---|---|---|---|---|---|
| Blood transfusion | 31.9 (<0.001) | 19.4 (<0.001) | 9.9 (<0.001) | 11.9 (<0.001) | 9.6 (<0.001) |
| Operation | 12.1 (<0.001) | 7.1 (<0.001) | 6.8 (<0.001) | 7.5 (<0.001) | 11.1 (<0.001) |
| Angiography | 2.1 (<0.001) | 2.2 (<0.001) | 3.6 (<0.001) | 3.9 (<0.001) | 6.9 (<0.001) |
| Chest tube | 8.2 (<0.001) | 5.3 (<0.001) | 4.3 (<0.001) | 5.6 (<0.001) | 3.9 (<0.001) |
| Central line | 13.9 (<0.001) | 13.0 (<0.001) | 8.6 (<0.001) | 11.1 (<0.001) | 15.2 (<0.001) |
| TBI intervention | 4.0 (<0.001) | 8.2 (<0.001) | 8.4 (<0.001) | 9.8 (<0.001) | 57.0 (<0.001) |
| Emergent intubation | 44.2 (<0.001) | 24.1 (<0.001) | 7.2 (<0.001) | 11.5 (<0.001) | 19.6 (<0.001) |
| Any NEI-6 | 30.9 (<0.001) | 15.7 (<0.001) | 6.9 (<0.001) | 9.9 (<0.001) | 12.0 (<0.001) |
NEI-6 = need for an emergent intervention within 6 h; ICU = intensive care unit; OR = odds ratio; TBI = traumatic brain injury.
Discussion
This study compares the performance of NEI-6 with TTM, NFTI, and STAT on TTA appropriateness and trauma mortality. While TTM, NFTI, and STAT use a broad definition for trauma activation appropriateness, NEI-6 is more narrow without an associated increase in mortality. For example, TTM, NFTI, and STAT defined an additional 5000-10,000 patients as needing a trauma activation. However, the majority of these patients did not require emergent interventions, thus reducing the potential benefit that is offered by a full TTA. NEI-6 identified patients at highest risk of mortality from their traumatic injury. Unnecessary full TTAs result in wasted hospital resources and trauma activation fatigue. It is imperative to ensure that any definition of trauma activation appropriateness identifies the severely injured patient. The findings in this study suggest that NEI-6 appropriately identified severely injured trauma patients.
The American College of Surgeons (ACS) Committee on Trauma states that overtriage rates should range from 25% to 35%, while the undertriage rates should be less than 5%.5 Undertriage is a priority as it may result in preventable morbidity or mortality due to delay in care.16 Overtriage results in unnecessary resource utilization and can result in staff fatigue.16 The goal is to limit trauma-related mortality at nontrauma centers as risk of death is significantly lower when care is provided in a trauma center versus a nontrauma center.17,18 However, level 1 and level 2 trauma centers are limited by capacity and not able to care for all trauma-related injuries.19 To achieve 5% undertriage, trauma centers would need to increase their capacity fivefold,20 highlighting the need for an undertriage definition that consistently improves patient mortality. A previous study showed that decreasing undertriage rates using TTM increases overtriage.21 By NEI-6 criteria, 42% of patients received a full TTA without need for emergent intervention.
ISS ≥15 is suggested as a potential definition of major trauma.4 The ISS model resulted in higher rates of overtriage without associated mortality benefit and is incompletely correlated with the resource requirements of injured patients.3 ISS was the first widely used standardized severity of traumatic injury based on the three worst injuries in six body systems (head and neck, face, chest, abdomen, extremity, and external) squared then added together to produce the ISS score.22 The three highest AIS codes must be from three different regions.22 ISS gives equal weight to extremity and neurologic injuries despite the great differences in potential treatment options. Specifically, ISS gives equal weight to extremity and neurologic injuries despite the great differences in potential treatment options and patient outcomes. Previous studies have shown patients with limited versus full activation are dissimilar despite having an ISS of 16 or greater.23 The TTM 2014 version is a simple method for calculating overtriage and undertriage rates based on the ISS and the level of trauma team activation.24
Due to the deficiencies of the TTM method, NFTI and STAT were developed. The NFTI is an alternate indicator of major trauma based on need for therapeutic or diagnostic intervention. NFTI uses six commonly recorded registry fields to form a binary, resource consumption-based indicator of major trauma that performed at least as well as TTM.7 NFTI automatically assesses many of the variables likely to be considered in case reviews but does so in a reproducible way that is applicable between centers. The STAT method combines the TTM with NFTI.6 However, timely classification balancing resource consumption and injury severity is still needed. NFTI and STAT have significant drawbacks as they both miss important emergent interventions and include other patients unnecessarily based on delayed outcomes. First, NFTI and STAT only contain three elements reflecting rapid need for intervention (OR within 90 min, transfusion of PRBCs within 4 h, and transfer from the ED to Interventional Radiology). Significant urgent interventions such as chest tube, central line placement, or brain intervention are missed even though they are associated with increased mortality and adverse events in this study.8 Other patients meeting the criteria “mortality within 60 h or mechanical ventilation within 3 d” included in NFTI and STAT may not benefit from a full TTA as the outcome is delayed from initial presentation to the trauma bay. In our study, over 50% of patients meeting TTM, NFTI, and STAT criteria do not require an emergent intervention and did not have higher early mortality rates.
STAT is able to accurately identify patients who would benefit from a full TTA, but also includes many additional patients indiscriminately who would not benefit from a full TTA. However, in 21,539 STAT full TTAs, only 39.1% required an emergent intervention, the lowest any method examined. In contrast, 48.7% NFTI-positive patients required an emergent intervention, but overtriage rates were significantly higher. A similar number of patients (4195 patients with ISS < 15 versus 5241 patients with ISS ≥15) actually underwent a full TTA. The patients with ISS <15 may have been triaged to full TTA based on physician discretion in anticipation of quickly needing mobilize resources to provide an urgent therapy. These limitations highlight the need for a system that adequately balances undertriage and the need for emergent interventions.
NEI-6 has a low rate of undertriage (6.5%), and these patients did not have a higher mortality rate. The mortality rates of all patients who did not meet NEI-6, STAT, NFTI, and TTM criteria were examined. NEI-6-negative patients that would have been considered undertriage by other methods did not have an higher 48 h mortality (0.44%). In contrast, 12.04% of patients who met NEI-6 criteria suffered early mortality. All methods had a similar mortality (0.5%) for patients not meeting full TTA activation criteria. Thus, there was not an increase in mortality for NEI-6-negative patients who underwent partial TTA instead of full TTA.
Emergency intervention based on NEI-6 criteria may help with adherence to trauma activation criteria. The ACS mandatory criteria for highest level of trauma activation include: hypotension (<90), gunshot to neck, chest, or abdomen, GCS < 9 from trauma, transfer patients receiving blood to maintain vital signs, intubation or respiratory compromise, and ED physician discretion. Noncompliance with ACS minimum criteria is associated with increased mortality.8 A study in 2009 evaluated overtriage and undertriage based on trauma team activation after guideline introduction noted significant overtriage (74%) based on ISS, mechanism of injury, ICU admission, need for intubation, and death within 30 d.25 There was a twofold increased odds ratio of mortality (adjusted for ISS) in undertriaged patients.25 One of the reasons for poor compliance is likely that end points of activation criteria, better defined by NEI-6, are currently poorly described.
The current study reveals that NEI-6 is an improved method of evaluating trauma activation appropriateness, because it is available within 6 h, reflects the need for urgent intervention, and is easy to calculate. The ACS-COT highest level trauma activation criteria (such as hypotension and ongoing transfusion) logically lead to the need for intervention as defined by NEI-6 as they reflect risk of potential bleeding needing additional transfusion, operative intervention, and/or interventional radiology. Less injured patients are cared for without full TTA without added mortality or resource utilization. An imperative first step to develop evidenced-based activation criteria is to develop an appropriate definition of trauma activation appropriateness. Following validation of NEI-6 in a large prospective study, predictive algorithms could be developed to identify field criteria that are associated with NEI-6-positive patients, such as hypotension, respiratory distress, or depressed GCS reflecting the need for blood transfusion, chest tube/intubation, or brain injury intervention. Eight predictors were recently identified based on ISS to predict the need for full TTA: age; systolic blood pressure; Glasgow Coma Scale score; mechanism criteria; penetrating injury to the head, thorax, or abdomen; signs and/or symptoms of head or neck injury; expected injury in the AIS thorax region; and expected injury in two or more AIS regions.26 The majority of the predictors suggest need for emergent intervention. These criteria have the potential to establish evidence-based trauma activation criteria for a full TTA and verified appropriately with NEI-6.
This study is limited by its retrospective nature. However, all current methods included in the study are retrospective. Therefore, this limitation does not likely reflect an error in the study’s design. In addition, we are unable to effectively compare early mortality with NFTI due to 48 h mortality being a component of the NFTI criteria and, therefore, accurately detect differences in early mortality between NEI-6 and NFTI. An additional limitation is the use of MTQIP, which only includes Level 1 and 2 trauma centers in the states of Michigan and Minnesota and may not account for regional variation. It is unknown if NEI-6 will work as well in pediatric settings or at other trauma centers. Additionally, there was a selection bias for those patients who received a full TTA. 4168 patients were NEI-6-negative but received a full TTA. The mortality of those patients without undergoing full TTA is unknown.
Conclusions
NEI-6 is a novel tool to analyze the performance of trauma team activation appropriateness. When compared to TTM, NFTI, and STAT, it resulted in significantly less undertriage. Additionally, TTM, NFTI, and STAT resulted in significantly more full TTAs than NEI-6 without the added benefit of identifying additional patients at risk for early mortality. NEI-6 represents a novel and effective tool to determine trauma activation appropriateness. This method should be considered to define activation appropriateness in the future.
Acknowledgment
Mark R. Hemmila receives support from Blue Cross Blue Shield of Michigan and Blue Care Network (a nonprofit mutual company) for conduct of The Michigan Trauma Quality Improvement Program with a Collaborative Quality Initiatives grant.
Footnotes
Disclosure
The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in this article.
There are no other conflicts of interest or sources of funding.
This study was presented as an oral presentation at the Academic Surgical Congress (ASC) Annual Scientific Meeting on February 6, 2019 in Houston, TX.
REFERENCES
- 1.Eastern Association for the Surgery of Trauma. Triage of the trauma patient. 2010. Available at: https://www.east.org/education/practice-management-guidelines/triage-of-the-trauma-patient. Accessed March 5, 2019.
- 2.Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 3.Baxt WG, Upenieks V. The lack of full correlation between the Injury Severity Score and the resource needs of injured patients. Ann Emerg Med. 1990;19:1396–1400. [DOI] [PubMed] [Google Scholar]
- 4.Cribari C, Gujral I. The Cribari matrix: a key component for trauma performance improvement.. Annual Meeting of the American Association for the Surgery of Trauma.; 2006. Available at: https://www.researchgate.net/publication/322711160_Avoiding_Cribari_gridlock_the_Standardized_Triage_Assessment_Tool_improves_the_accuracy_of_the_Cribari_Matrix_Method_in_identifying_potential_over-_and_undertriage. Accessed December 9, 2016.
- 5.Cribari C, Martin ER, Bonta MJ, Dean BC. Consequences of over and undertriage. Annual meeting of the American association for the Surgery of trauma; 2006. Available at: http://www.aast.org/asset.axd?id=1f51f1c3-f99b-4120-a4e6751236c7a94c&t=633851644561770000. Accessed December 9, 2016.
- 6.Roden-Foreman JW, Rapier NR, Yelverton L, Foreman ML. Avoiding Cribari gridlock: the standardized triage assessment tool improves the accuracy of the Cribari matrix method in identifying potential overtriage and undertriage. J Trauma Acute Care Surg. 2018;84:718–726. [DOI] [PubMed] [Google Scholar]
- 7.Roden-Foreman JW, Rapier NR, Yelverton L, Foreman ML. Asking a better question: development and evaluation of the need for trauma intervention (NFTI) metric as a novel indicator of major trauma. J Trauma Nurs. 2017;24:150–157. [DOI] [PubMed] [Google Scholar]
- 8.Tignanelli CJ, Vander Kolk WE, Mikhail JN, Delano MJ, Hemmila MR. Non-compliance with ACS-COT recommended criteria for full trauma team activation is associated with undertriage deaths. J Trauma Acute Care Surg. 2018;84:287–294. [DOI] [PubMed] [Google Scholar]
- 9.Tominaga GT, Dandan IS, Schaffer KB, Nasrallah F, Gawlik RNM, Kraus JF. Trauma resource designation: an innovative approach to improving trauma system overtriage. Trauma Surg Acute Care Open. 2017;2:e000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hemmila MR, Jakubus JL. Trauma quality improvement. Crit Care Clin. 2017;33:193–212. [DOI] [PubMed] [Google Scholar]
- 11.Hemmila MR, Jakubus JL, Crain-Nielsen AH, et al. The Michigan trauma quality improvement program: results from a collaborative quality initiative. J Trauma Acute Care Surg. 2017;82:867–876. [DOI] [PubMed] [Google Scholar]
- 12.Calland JF, Nathens AB, Young JS, et al. The effect of dead-on-arrival and emergency department death classification on risk-adjusted performance in the American College of Surgeons Trauma Quality Improvement Program. J Trauma Acute Care Surg. 2012;73:1086–1091 [discussion 1091-1092]. [DOI] [PubMed] [Google Scholar]
- 13.Bennett DA. How can I deal with missing data in my study? Aust N Z J Public Health. 2001;25:464–469. [PubMed] [Google Scholar]
- 14.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8:3–15. [DOI] [PubMed] [Google Scholar]
- 15.Ingraham AM, Xiong W, Hemmila MR, et al. The attributable mortality and length of stay of trauma-related complications: a matched cohort study. Ann Surg. 2010;252:358–362. [DOI] [PubMed] [Google Scholar]
- 16.MTQIP Data Dictionary. Available at: https://www.mtqip.org/node/32/#data-dictionary. Accessed March 18, 2009.
- 17.Adzemovic T, Murray T, Jenkins P, et al. Should they stay or should they go? Who benefits from interfacility transfer to a higher level trauma center following initial presentation at a lower level trauma center. J Trauma Acute Care Surg. 2019;86:952–960. [DOI] [PubMed] [Google Scholar]
- 18.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. [DOI] [PubMed] [Google Scholar]
- 19.Zocchi MS, Hsia RY, Carr BG, Sarani B, Pines JM. Comparison of mortality and costs at trauma and Nontrauma centers for minor and moderately severe injuries in California. Ann Emerg Med. 2016;67:56–67.e5. [DOI] [PubMed] [Google Scholar]
- 20.Mohan D, Rosengart MR, Farris C, Cohen E, Angus DC, Barnato AE. Assessing the feasibility of the American College of Surgeons’ benchmarks for the triage of trauma patients. Arch Surg. 2011;146:786–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferguson EJ, Brown M. Concurrent case review and retrospective review using the matrix method are complementary methods for tracking and improving timeliness of care in a level I trauma center. Am Surg. 2016;82:319–324. [PubMed] [Google Scholar]
- 22.Association for the Advancement of Automotive Medicine. A specialized course on injury scaling: uses and techniques; 2015. Available at: https://www.aaam.org/abbreviated-injury-scale-ais/Revised. Accessed April 21, 2019.
- 23.Davis JW, Dirks RC, Sue LP, Kaups KL. Attempting to validate the overtriage/undertriage matrix at a Level I trauma center. J Trauma Acute Care Surg. 2017;83:1173–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Committee on Trauma, American College of Surgeon. Resources for Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2014. [Google Scholar]
- 25.Rehn M, Eken T, Krüger AJ, Steen PA, Skaga NO, Lossius HM. Precision of field triage in patients brought to a trauma centre after introducing trauma team activation guidelines. Scand J Trauma Resusc Emerg Med. 2009;17:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Rein EAJ, van der Sluijs R, Voskens FJ, et al. Development and validation of a prediction model for prehospital triage of trauma patients. JAMA Surg. 2019;154:421–429. [DOI] [PMC free article] [PubMed] [Google Scholar]


