Abstract
Background
The impact of telehealth on cardiovascular care during the COVID-19 pandemic on patient satisfaction and factors associated with satisfaction are not well characterized.
Methods
We conducted a nonrandomized, prospective cross-sectional survey study for outpatient telehealth cardiovascular visits over a 169-day period utilizing a validated telehealth usability questionnaire. For each variable, patients were divided into 2 groups—1 with scores above the median, labeled “greater satisfaction,” and the other with scores below the median, labeled “less satisfaction.”
Results
A total of 13,913 outpatient telehealth encounters were successfully completed during the study period. A total of 7327 unique patients were identified and received a survey invitation; 5993 (81.8%) patients opened the invitation, and 1034 (14.1%) patients consented and completed the survey. Overall mean and median scores were 3.15 (standard deviation 0.74) and 3.37 (interquartile range 2.73–3.68) (maximum score 4.00). Greater satisfaction was noted among younger patients (mean age 63.3 ± 14.0 years, P = .005), female gender (46.3%, P = .007), non-White ethnicity (24.2% P = .006), self-identified early adopters and innovators of new technology (49.8%, P < .001), 1-way travel time greater than 1 hour (22.3%, P < .001), 1-way travel distance greater than 10 miles (49.0%, P < .001), patients needing child care arrangement (16.4%, P < .001), and history of orthotopic heart transplant (OHT) (5.1%, P = .04).
Conclusion
Patients reported overall satisfaction with telehealth during the COVID-19 pandemic. Factors associated with patient convenience, along with female gender, younger age, and non-White ethnicity, correlated with greater satisfaction. Cardiovascular comorbidities did not correlate with greater satisfaction except for OHT. Further research into the impact of telehealth on patient satisfaction, safety, and clinical outcomes is needed.
Keywords: Cardiology, Cardiovascular disease, COVID-19, Patient satisfaction, Telehealth, Telemedicine
Key Findings.
-
•
Telehealth in Cardiovascular care during the COVID-19 pandemic is overall highly satisfactory and well-received.
-
•
Factors that are associated with even greater satisfaction include younger patients, female gender, non-white ethnicity, self-identified early adopters and innovators of new technology. Factors improving patient convenience such as one-way travel time greater than 1 hour, one-way travel distance greater than 10 miles and patients needing child care arrangement were also to improve satisfaction.
-
•
Among the most relevant cardiovascular comorbidities, only a history of orthotopic heart transplant was found to be associated with greater satisfaction. This finding is likely driven by the longer distance of travel required from their home. No difference was seen between patients with 0 co-morbidities and 1 or more co-morbidities.
Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), responsible for coronavirus disease 2019 (COVID-19), was declared a global pandemic on March 11, 2020.1 COVID-19 upended the entire healthcare system, as the priority to slow the transmission of SARS-CoV-2 initially halted the traditional model of office- and facility-based healthcare delivery. Providers adjusted their practices accordingly to continue providing care for patients. In response to the necessary social distancing and shelter-in-place orders, telehealth found widespread appeal and adoption as an essential tool to mitigate the transmission of SARS-CoV-2.2
Telehealth, also referred to as telemedicine, had mixed results prior to the COVID-19 pandemic when implemented to support the care of cardiovascular diseases such as heart failure.3, 4, 5 The Centers for Medicare and Medicaid Services (CMS) defines telehealth as “the exchange of medical information from one site to another through electronic communication to improve a patient’s health.”6 This broad definition includes video encounters that utilize synchronous, 2-way audio-video communication between a patient and healthcare provider. Traditionally, telehealth lacked widespread adoption for several reasons, including lower reimbursements, geographic restrictions, inadequate technological capabilities by healthcare providers and institutions, and variation in policies and licensure by individual states.7 In recent years, barriers to adopting telehealth have been incrementally lowered through broader telehealth reimbursement codes enacted by CMS, as well as legislation passed by several states granting telehealth parity of reimbursement with traditional in-person visits. Owing to the COVID-19 pandemic, CMS and the Department of Health and Human Services removed most of the financial and geographic barriers previously limiting this technology, and swift adoption by healthcare providers soon followed.8 In April 2020, nearly half (43.5%) of all outpatient primary care encounters were conducted through telehealth, compared to less than 1% of all primary care encounters in February 2020.9 Telehealth has also been shown to correlate with high patient satisfaction during the COVID-19 pandemic for other medical specialties.10 In previous infectious public health emergencies, telehealth has also been shown to be helpful in promoting social distancing while maintaining healthcare delivery, including SARS-CoV-1, Middle East Respiratory Syndrome coronavirus, and Ebola and Zika viruses.11,12
Patients with underlying cardiovascular comorbidities are at high risk for adverse outcomes if infected with SARS-CoV-2. The importance of utilizing telehealth to protect vulnerable patients with cardiovascular disease cannot be overstated.13 Our outpatient cardiology program rapidly transitioned to a practice with a significant proportion of visits conducted virtually, and continues to support patient care with a blend of in-person and telehealth visits. A transition to a distributive model of care delivery, with clinicians meeting patients at the point of care, rather than the traditional centralized office or facility-based model, is an ongoing trend that is likely to accelerate. Understanding how patients interact with the tools such as telehealth in their healthcare journey to maximize their satisfaction and outcomes in disease management is attracting increasing attention from health systems, clinicians, start-up companies, employers, brokers, and payors.14 Given the unclear impact of the virtual clinic on patient care, we performed a prospective survey study to evaluate patients’ perspectives with telehealth, as well as factors associated with greater satisfaction.
Methods
Study design and setting
This study was a nonrandomized, prospective, single-site cross-sectional survey study evaluating patient satisfaction with telehealth visits during the COVID-19 pandemic. Telehealth visits provided outpatient virtual care by cardiovascular clinicians at UCLA Health during a consecutive 169-day period from March 13, 2020, through August 31, 2020. For reference, initial Los Angeles city and California state safer-at-home orders were issued on March 17, 2020 and March 19, 2020, respectively. Telehealth visits were defined as a synchronous, 2-way visual and audio encounter between the patient and clinician through a mobile smartphone or tablet application (Epic Systems Corporation, Verona, WI) available on iOS (Apple, Inc, Cupertino, CA) and Android (Google, LLC, Mountain View, CA), that interfaced with an electronic health record client (Epic Systems Corporation). The study was designed by the principal investigators, who had unrestricted access to the data, maintained the database, prepared all drafts of the manuscript, made the decision to submit the manuscript for publication, and vouch for the integrity of the study. The study was reviewed and approved by the institutional review board. No internal or external funding sources were utilized for the design, implementation, or analysis of this study.
Selection of participants
Eligible patients were identified as individuals greater than 18 years of age who completed a scheduled telehealth (video) visit with an outpatient cardiology clinician during the study period.
Patients meeting eligibility criteria were electronically recruited through a secure messaging platform by the study investigators after their telehealth visit. Each eligible patient was sent an anonymous hyperlink to an online questionnaire administered via Qualtrics, Inc (Seattle, WA). Patients who consented to participate completed the survey questionnaire electronically. Since some patients had multiple visits with providers during the study period and thus received multiple survey invitations, we identified the total number of unique patients seen. For duplicate survey responses, only the first survey response was utilized in the analysis to standardize the experience of telehealth across the study population. Survey responses included in the analysis were collected until the end of the data collection period, which ended December 31, 2020.
Materials and measurements
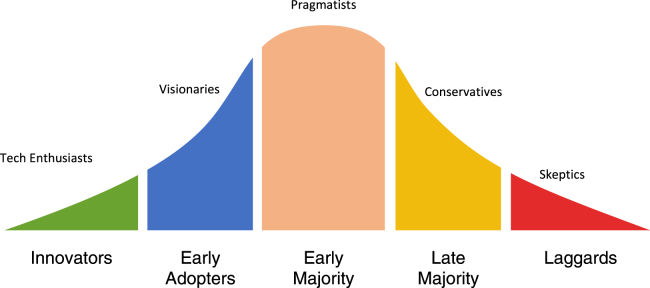
A previously validated telehealth usability questionnaire (TUQ) was utilized for this research study, which evaluates 6 domains: usefulness, ease of use, interface quality, interaction quality, reliability, and satisfaction.15 The TUQ questionnaire was utilized for both its validated comprehensive assessment of patients’ and clinicians’ perspectives on telehealth and its high frequency of use in telehealth research.16 There were 32 questions in the questionnaire: 20 questions were utilized from the TUQ, and 12 questions collected self-reported patient data regarding demographics, cardiovascular comorbidities, geography, insurance payor, commute distance, travel time, need for childcare, income, and self-reported technology adoption traits (Figure 1).17 Qualtrics, Inc was utilized to administer, collect, and store survey data.
Figure 1.
Technology adoption curve.
Statistical methods
Average patient satisfaction scores were calculated for each patient by assigning the survey responses with the following values: 0 = “Strongly Disagree,” 1 = “Somewhat Disagree,” 2 = “Neither Agree nor Disagree,” 3 = “Somewhat Agree,” and 4 = “Strongly Agree.” Patient and telehealth visit characteristics were summarized using means and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables. To evaluate differences for a given variable, patients were divided into 2 groups—1 with mean TUQ scores greater than median, labeled “greater satisfaction,” and the other with mean TUQ scores less than median, labeled “less satisfaction.” Student t test (for continuous variables) and χ2 test, or Fisher’s exact test, where appropriate (for categorical variables), were used to determine if the variables were different between the 2 groups. SAS version 9.4 (SAS Institute, Cary, NC) was used for all statistical analyses. A P value < .05 is considered statistically significant.
Results
Descriptive characteristics of the sample
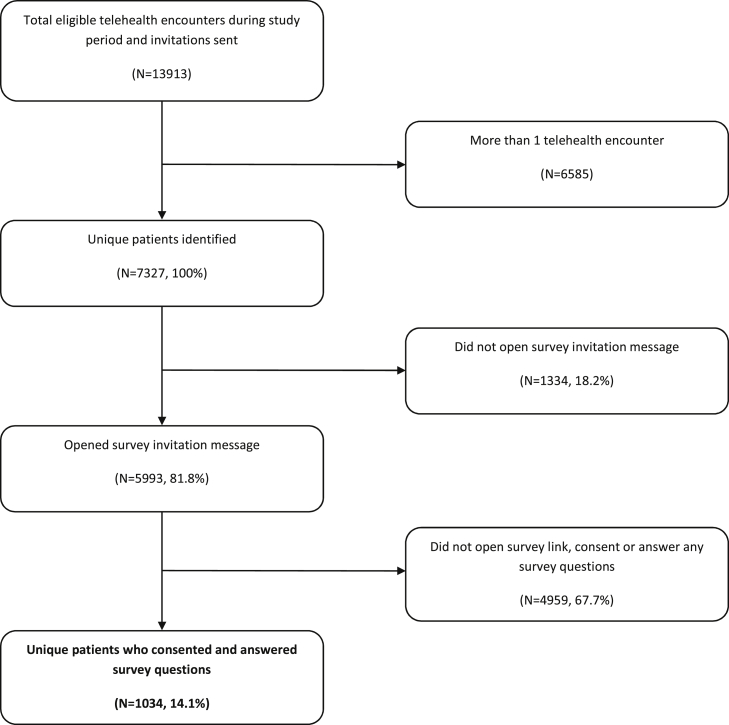
A total of 13,913 telehealth encounters were successfully completed for an outpatient video visit during the study period, and 7327 unique patients received a survey invitation. Of the unique patients identified, 5993 (81.8%) patients opened the invitation, and 1034 (14.1%) patients consented and completed the survey (Figure 2). As some patients had multiple telehealth visits during the study period and responded to the survey request more than once, subsequent survey responses by the same individual were excluded, as detailed in the Methods section. A total of 95 duplicate survey responses were excluded from analysis.
Figure 2.
Patient eligibility and selection.
Of the 7327 eligible patients who had a telehealth encounter during the study period, the mean age was 61.3 years (SD 16.2), the majority were female (3754, 51.2%), and they were predominantly White (4777, 65.2%). Non-White patients (2151, 29.4%) were noted to have the following demographics: Hispanic (430, 5.9%), Asian (644, 8.8%), Black (528, 7.2%), Pacific Islander (11, 0.2%), Native American or Alaskan (30, 0.4%), other (508, 6.8%). Patients who declined to specify or had missing race comprised 399 (5.4%) of eligible patients (Table 1).
Table 1.
Descriptive patient characteristics: Overall, study responders, and study nonresponders
| Statistic or category | Total eligible patients† (N = 7327) | Study responders‡ (N = 1034) | Study nonresponders‡ (N = 6293) |
|---|---|---|---|
| Age mean (SD), years | 61.3 (SD, 16.2) | 64.5 (SD, 13.7) | 59.9 (SD, 16.5) |
| Gender | |||
| Female | 3754 (51.2%) | 479 (46.3%) | 3275 (52.0%) |
| Male | 3571 (48.7%) | 553 (53.5%) | 3018 (48.0%) |
| Prefer not to say | 2 (0.1%) | 2 (0.2%) | . |
| Ethnicity | |||
| White | 4777 (65.2%) | 777 (75.1%) | 4000 (63.6%) |
| Non-White | 2151 (29.4%) | 250 (24.2%) | 1901 (30.2%) |
| Hispanic | 430 (5.9%) | 74 (7.2%) | 356 (5.7%) |
| Asian | 644 (8.8%) | 66 (6.4%) | 578 (9.2%) |
| Black | 528 (7.2%) | 62 (6.0%) | 466 (7.4%) |
| Pacific Islander | 11 (0.2%) | 6 (0.6%) | 5 (0.1%) |
| Native American or Alaskan | 30 (0.4%) | 4 (0.4%) | 26 (0.4%) |
| Other | 508 (6.9%) | 38 (3.7%) | 470 (7.5%) |
| Declined to specify or missing | 399 (5.4%) | 7 (0.7%) | 392 (6.2%) |
Percentages in the overall column are out of the total number of study participants (excluding missing patients).
Percentages in the study responders and study nonresponders columns are out of the total number of participants for each column.
Of the 1034 patients who consented and completed the survey, overall mean and median TUQ scores were 3.15 (SD ± 0.74) and 3.37 (interquartile range 2.73–3.68), respectively, out of a maximum possible score of 4.00. Overall mean age was 64.5 years (SD 13.7). The majority were male (553, 53.5%), were predominantly White (777, 75.7%), and did not have previous experience with telehealth (701, 67.8%) (Table 2). Among non-White patients (250, 24.2%), the following representation was noted: Hispanic (74, 7.2%), Asian (66, 6.4%), Black (62, 6.0%), Pacific Islander (6, 0.6%), Native American or Alaskan (4, 0.4%), other (38, 3.7%); 7 (0.7%) respondents did not select a race (Table 1). Additionally, the majority of patients commuted less than or equal to 1 hour each way for clinic visits (800, 77.7%), did not require childcare arrangement (83.0%), and were relatively evenly split between 1-way travel distances of less than or equal to 10 miles (527, 51.0%) and 10 miles or greater (507, 49.0%). Visits were also largely routine follow-up visits for established patients (831, 80.4%) (Table 3). The mean number of comorbidities was 1.80 (SD 1.37, maximum number 10) (Table 4).
Table 2.
Descriptive characteristics of study cohort: Overall and stratified by satisfaction score
| Statistic or category | Overall† (N = 1034) | Less satisfaction‡ (mean score <3.37) (N = 531) |
Greater satisfaction‡ (mean score ≥3.37) (N = 503) |
P value |
|---|---|---|---|---|
| Mean age (SD) | 64.5 (SD, 13.7) | 65.7 (SD, 13.4) | 63.3 (SD, 14.0) | .005 |
| Gender | ||||
| Female | 479 (46.3%) | 224 (46.8%) | 255 (53.2%) | .007 |
| Male | 553 (53.5%) | 307 (55.5%) | 246 (44.5%) | . |
| Prefer not to say | 2 (0.2%) | 0 (0.0%) | 2 (100.0%) | . |
| Ethnicity | ||||
| Non-White | 250 (24.3%) | 109 (43.6%) | 141 (56.4%) | .006 |
| White | 777 (75.7%) | 417 (53.7%) | 360 (46.3%) | . |
| Missing | 7 | 5 | 2 | . |
| Previous experience with telehealth visits | ||||
| No | 701 (72.2%) | 363 (51.8%) | 338 (48.2%) | .48 |
| Yes | 270 (27.8%) | 133 (49.3%) | 137 (50.7%) | . |
| Missing | 63 | 35 | 28 | . |
| Adoption of new technology | ||||
| Innovators / early adopters | 515 (50.9%) | 231 (44.9%) | 284 (55.1%) | <.001 |
| Early majority | 318 (31.5%) | 172 (54.1%) | 146 (45.9%) | . |
| Late majority / laggards | 178 (17.6%) | 120 (67.4%) | 58 (32.6%) | . |
| Missing | 23 | 8 | 15 | . |
| Health insurance | ||||
| Medicaid | 28 (2.7%) | 9 (32.1%) | 19 (67.9%) | .09 |
| Medicare | 509 (49.7%) | 271 (53.2%) | 238 (46.8%) | . |
| Private insurance | 487 (47.6%) | 247 (50.7%) | 240 (49.3%) | . |
| Missing | 10 | 4 | 6 | . |
Percentages in the overall column are out of the total number of study participants (excluding missing patients).
Percentages in the less and greater satisfaction columns are out of the total number of participants for each category.
Table 3.
Summary of convenience and visit characteristics
| Statistic or category | Overall† (N = 1034) | Less satisfaction‡ (mean score <3.37) (N = 531) |
Greater satisfaction‡ (mean score ≥3.37) (N = 503) |
P value |
|---|---|---|---|---|
| One-way travel distance to clinic | ||||
| Less than or equal to 10 miles | 527 (51.0%) | 309 (58.6%) | 218 (41.4%) | <.0001 |
| More than 10 miles | 507 (49.0%) | 222 (43.8%) | 285 (56.2%) | . |
| One-way travel time to clinic | ||||
| Less than or equal to 1 hour | 800 (77.7%) | 439 (54.9%) | 361 (45.1%) | <.001 |
| Greater than 1 hour | 230 (22.3%) | 89 (38.7%) | 141 (61.3%) | |
| Missing | 4 | 3 | 1 | . |
| Telehealth obviated arrangement for childcare | ||||
| No | 828 (83.0%) | 456 (55.1%) | 372 (44.9%) | <.0001 |
| Yes | 170 (17.0%) | 58 (34.1%) | 112 (65.9%) | . |
| Missing | 36 | 17 | 19 | . |
| Annual estimated household income | ||||
| Less than or equal to $75,000 | 346 (35.4%) | 175 (50.6%) | 171 (49.4%) | .99 |
| $75,000–$150,000 | 349 (35.7%) | 177 (50.7%) | 171 (49.3%) | . |
| Greater than $150,000 | 282 (28.9%) | 144 (51.1%) | 138 (48.9%) | . |
| Missing | 57 | 35 | 22 | . |
| Reason for visit | ||||
| New symptom (established patient) | 63 (6.1%) | 36 (57.1%) | 27 (42.9%) | .19 |
| Routine follow-up (established patient) | 831 (80.4%) | 428 (51.5%) | 403 (48.5%) | . |
| New patient visit | 90 (8.7%) | 38 (42.2%) | 52 (57.8%) | . |
| Other | 50 (4.8%) | 29 (58.0%) | 21 (42.0%) | . |
Percentages in the overall column are out of the total number of study participants (excluding missing patients).
Percentages in the less and greater satisfaction columns are out of the total number of participants for each category.
Table 4.
Medical comorbidities descriptive summary
| Statistic or category | Overall† (N = 1034) | Less satisfaction‡ (mean score <3.37) (N = 531) |
Greater satisfaction‡ (mean score ≥3.37) (N = 503) |
P value |
|---|---|---|---|---|
| Comorbidity sum | ||||
| N | 1027 | 526 | 501 | .93 |
| Mean (SD) | 1.8 (1.37) | 1.8 (1.40) | 1.8 (1.35) | . |
| Missing | 7 | 5 | 2 | . |
| History of OHT | ||||
| No | 974 (94.8%) | 506 (52.0%) | 468 (48.0%) | .04 |
| Yes | 53 (5.2%) | 20 (37.7%) | 33 (62.3%) | . |
| Missing | 7 | 5 | 2 | . |
| Hypercholesterolemia | ||||
| No | 574 (55.9%) | 288 (50.2%) | 286 (49.8%) | .45 |
| Yes | 453 (44.1%) | 238 (52.5%) | 215 (47.5%) | . |
| Missing | 7 | 5 | 2 | . |
| Hypertension | ||||
| No | 518 (50.4%) | 255 (49.2%) | 263 (50.8%) | .20 |
| Yes | 509 (49.6%) | 271 (53.2%) | 238 (46.8%) | . |
| Missing | 7 | 5 | 2 | . |
| History of MI, PCI, or CABG | ||||
| No | 827 (80.5%) | 424 (51.3%) | 403 (48.7%) | .95 |
| Yes | 200 (19.5%) | 102 (51.0%) | 98 (49.0%) | . |
| Missing | 7 | 5 | 2 | . |
| Current or former smoking history | ||||
| No | 890 (86.7%) | 457 (51.3%) | 433 (48.7%) | .83 |
| Yes | 137 (13.3%) | 69 (50.4%) | 68 (49.6%) | . |
| Missing | 7 | 5 | 2 | . |
| Pacemaker or ICD present | ||||
| No | 899 (87.5%) | 459 (51.1%) | 440 (48.9%) | .79 |
| Yes | 128 (12.5%) | 67 (52.3%) | 61 (47.7%) | . |
| Missing | 7 | 5 | 2 | . |
| LVAD present | ||||
| No | 1014 (98.7%) | 521 (51.4%) | 493 (48.6%) | .36 |
| Yes | 13 (1.3%) | 5 (38.5%) | 8 (61.5%) | . |
| Missing | 7 | 5 | 2 | . |
| Chronic kidney disease | ||||
| No | 936 (91.1%) | 480 (51.3%) | 456 (48.7%) | .89 |
| Yes | 91 (8.9%) | 46 (50.5%) | 45 (49.5%) | . |
| Missing | 7 | 5 | 2 | . |
| Liver disease | ||||
| No | 985 (95.9%) | 508 (51.6%) | 477 (48.4%) | .27 |
| Yes | 42 (4.1%) | 18 (42.9%) | 24 (57.1%) | . |
| Missing | 7 | 5 | 2 | . |
| 1 or more cardiac comorbidity present | ||||
| No | 194 (18.9%) | 100 (51.5%) | 94 (48.5%) | .92 |
| Yes | 833 (81.1%) | 426 (51.1%) | 407 (48.9%) | . |
| Missing | 7 | 5 | 2 | . |
CABG = coronary artery bypass surgery; ICD = implantable cardioverter-defibrillator; LVAD = left ventricular assist device; MI = myocardial infarction; OHT = orthotopic heart transplantation; PCI = percutaneous coronary intervention.
Percentages in the overall column are out of the total number of study participants (excluding missing patients).
Percentages in the less and greater satisfaction columns are out of the total number of participants for each category.
Factors associated with greater satisfaction
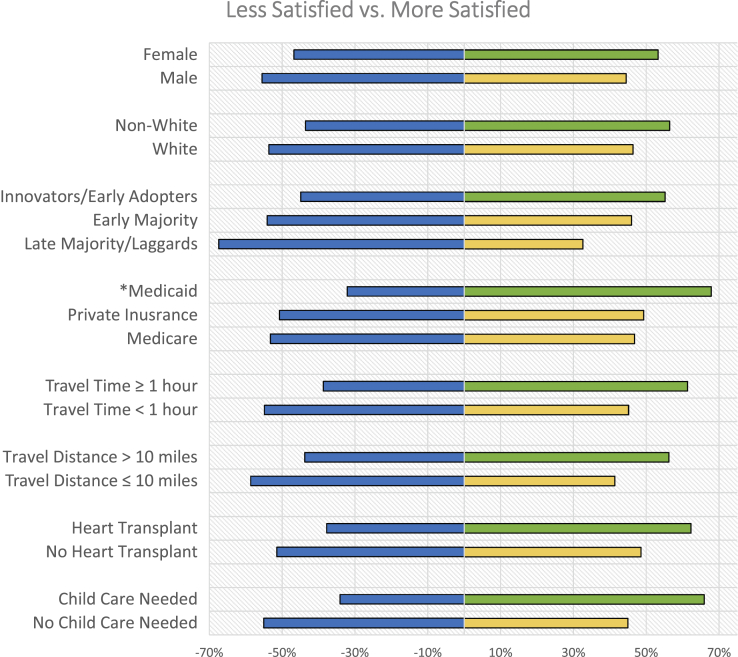
Greater satisfaction with telehealth was noted among younger patients (mean age 63.3 (SD 14.0) years, P = .005), patients of female gender (479, 46.3%, P = .007), patients of non-White ethnicity (250, 24.3%, P = .006), self-identified early adopters and innovators of new technology (515, 50.9%, P < .001), those with 1-way travel time greater than 1 hour (230, 22.3%, P < .001), those with 1-way travel distance greater than 10 miles (507, 49.0%, P < .001), and patients needing childcare arrangement (170, 17.0%, P < .001). While not found to be statistically significant, there was a markedly higher proportion of patients with greater satisfaction with Medicaid insurance (67.9% vs 32.1%), though they represented only a small percentage of the overall study population (28, 2.7%, P = .08). No significant differences between groups were noted with other factors such as prior telehealth experience, type of visit (established or new patients), or household income (Table 2, Table 3). Among patients needing childcare arrangement (170, 16.4%), no statistically significant difference was noted between genders or among ethnicity and annual estimated income. Females and males were evenly represented, with 85 (50%) patients each in this subgroup (Table 5). Figure 3 provides a graphical representation of the percentages of patients with greater and less satisfaction for given factors that were found to be statistically significant or near statistical significance.
Table 5.
Descriptive summary of satisfaction for patients requiring childcare
| Statistic or category | Overall† (N = 170) | Less satisfaction‡ (mean score <3.37) (N = 58) |
Greater satisfaction‡ (mean score ≥3.37) (N = 112) |
P value |
|---|---|---|---|---|
| Gender | ||||
| Female | 85 (50.0%) | 27 (31.8%) | 58 (68.2%) | .52 |
| Male | 85 (50.0%) | 31 (36.5%) | 54 (63.5%) | . |
| Ethnicity | . | |||
| Non-White | 81 (47.9%) | 23 (28.4%) | 58 (71.6%) | .16 |
| White | 88 (52.1%) | 34 (38.6%) | 54 (61.4%) | . |
| Missing | 1 | 1 | . | . |
| Annual income estimate | ||||
| Less than or equal to $75,000 | 67 (40.4%) | 16 (28.1%) | 41 (71.9%) | .10 |
| $75,000–$150,000 | 57 (34.3%) | 21 (31.3%) | 46 (68.7%) | . |
| Greater than $150,000 | 42 (25.3%) | 20 (47.6%) | 22 (52.4%) | . |
| Missing | 4 | 1 | 3 | . |
Percentages in the overall column are out of the total number of study participants (excluding missing patients).
Percentages in the less and greater satisfaction columns are out of the total number of participants for each category.
Figure 3.
Factors associated with greater satisfaction. Percentages are out of the total number of participants for each category. Negative percentage signifies patient group with less satisfaction. Positive percentage signifies patient group with greater satisfaction. ∗P value > .05. All other variables listed with P value ≤ .05. Green: Greater than 50% of participants for a study variable had greater satisfaction. Yellow: Less than 50% of participants for a study variable had greater satisfaction. Blue: Less satisfied participants.
Cardiovascular comorbidities
The effect of underlying cardiovascular comorbidities on satisfaction was evaluated as well. Only patients with a history of OHT demonstrated greater satisfaction with telehealth (n = 53, 5.2%, P = .04). Even when underlying comorbidities were aggregated and mean scores compared between patients with zero comorbidities and 1 or more comorbidities, no significant differences in patient satisfaction were identified (Table 5). Among the patients with OHT, the majority lived more than 30 miles away from their usual site of care (34, 64.2%, P < .0001) (Table 6).
Table 6.
Orthotopic heart transplant and distance traveled
| One-way travel distance to clinic | Orthotopic heart transplant present (N = 53) | Orthotopic heart transplant absent (N = 974) | P value |
|---|---|---|---|
| Less than or equal to 30 miles | 19 (35.8%) | 787 (80.8%) | <.0001 |
| More than 30 miles | 34 (64.2%) | 187 (19.2%) | . |
Discussion
While telehealth was rapidly adopted by healthcare systems during the COVID-19 pandemic, its impact and long-term integration into clinical practice is just beginning. The major stakeholders of healthcare—clinicians, patients, health systems, and payors—were aligned during the pandemic, which accelerated widespread adoption. As a postpandemic world emerges, these stakeholders’ interests may diverge, but telehealth is likely to remain a major component of healthcare delivery.14 To our knowledge, our study is unique in that we evaluated perspectives of a large sample of patients regarding satisfaction with their virtual cardiovascular care during the COVID-19 pandemic in a major metropolitan area. Beyond identifying that overall satisfaction with telehealth was high, we believe our study is one of the earliest to objectively measure characteristics associated with greater satisfaction using a previously validated telehealth survey. Our focus on the patients’ perspective of adapting to virtual-based cardiovascular care during the COVID-19 pandemic reveals new insights into a topic that has not yet been well characterized.
The impact of demographics
Early studies during the pandemic have demonstrated that potential inequities for access to telehealth exist, with notable but inconsistent differences that vary based on age, race, gender, and primary language. One health system identified that older patients, Asian patients, and non-English-speaking patients had fewer successfully completed telemedicine visits (which included video and telephone encounters). Additionally, older patients, women, individuals identifying as Black or Hispanic, and those with lower household incomes were less likely to have completed a video visit during the pandemic.18,19 However, another health system studied the frequency of telemedicine utilization during the pandemic and noted that patients who were Asian, Black, or Hispanic had higher rates of telemedicine use during the pandemic.20 These inconsistent differences among differing racial groups in telehealth may have geographic or other unknown variables with differences that were not accounted for. The study results reported by Eberly and colleagues19 consisted of patients from the Greater Philadelphia, Pennsylvania, metropolitan area, whereas the results reported by Yuan and colleagues20 were composed of patients in the Los Angeles, California, metropolitan area. Additionally, how the health system operationalized access to telehealth and which technology platforms were utilized were not specified, and we speculate that these factors may also be potential variables affecting telehealth utilization.19,20 It also demonstrates that the impacts of telehealth on potential inequities in healthcare are currently unclear.
Our study demonstrates that non-White patients had a higher proportion of individuals with greater telehealth satisfaction than White patients. However, a large majority of our eligible patients and patients who participated in the study were White (65.2% and 75.1%, respectively), and the underlying reason for this large representation by a single group is unclear. Comparison with the demographics of office-based cardiology visits pre-pandemic was not evaluated in the scope of this study and is an additional limitation of this study. Thus, whether the patient demographics described in this study mirror the overall pre-pandemic demographics served by cardiology within UCLA Health is unclear, though this seems less likely with our study location in a diverse, metropolitan area. Additionally, it may reflect certain racial inequities with a widening digital divide in the access to healthcare, or it could reflect a propensity for individuals of certain racial backgrounds to be more likely to participate in online studies and share their experience. One study evaluated racial or ethnic and socioeconomic differences in the rates of online survey consent and partial and complete survey completion, and found that compared with Black participants, White and Asian participants were more likely to consent to participate, and White participants were more likely to complete the survey fully.21 Our study potentially identifies a similar finding in studying the telehealth experience; possible reasons could include greater familiarity, trust, and motivation to engage with the healthcare system or clinician; greater healthcare literacy (traditional and electronic); a higher baseline of technical proficiency (including improved navigation of the electronic health record portal); or better access to the necessary tools for telehealth (broadband technology, computers, and smartphones). Furthermore, our findings also might suggest that telehealth utilization among non-White ethnicities is lower, though when telehealth is utilized for this population, it may be a more satisfying experience. Underutilization of telehealth by underserved or at-risk populations may reflect another facet of the digital divide that could further widen disparities in healthcare, and clinicians should focus on utilizing telehealth to promote health equity through convenient and easy access to healthcare. Several studies have identified barriers to telehealth adoption, such as limited English proficiency, lack of access to broadband internet, and higher technical proficiency required to successfully integrate telehealth into clinical practice, and it is possible that these barriers may also have limited a more diverse racial representation of patient perspectives in our study.22, 23, 24 Additional research into the magnitude of these disparate findings in telehealth feedback and utilization among different racial groups, and how these differences change over time, is needed.
Our study also demonstrated a consistent finding of younger age correlating with greater satisfaction for survey responders. We identified that patients with greater satisfaction were 2.8 years younger than less satisfied patients and nearly 1.4 years younger than the overall average age of study participants. A younger age could reflect a higher level of technological proficiency, as the use of synchronous 2-way audiovisual platforms requires higher digital literacy than simple telephone calls. However, our study did not evaluate technological proficiency directly, instead using self-reported rates of new technology adoption as a surrogate marker, which also demonstrated that patients who adopted technology earlier in the lifecycle demonstrated a higher proportion of patients with greater satisfaction. Our study population, however, was noted to have an older mean age compared to the eligible patient population, which could reflect that older individuals were also more likely to respond to our survey invitation and participate in the study. Age as a likelihood to respond to a satisfaction survey with telehealth was not assessed for this study, and possible reasons for older patients participating in the survey may reflect greater availability, interest in telehealth satisfaction research, or other unknown variables.25
Regarding gender, while a previous study demonstrated lower odds of females successfully completing a video visit compared to males, our results demonstrate the opposite finding, and females comprised 51.2% of successfully completed telehealth encounters during the study period.19 While more males ultimately went on to consent and participate in the survey study, females who responded to the survey were noted to have a higher proportion of patients with greater satisfaction with their telehealth experience. Our study findings suggest that females utilized telehealth more frequently and reported greater satisfaction as well. With concerns that the pandemic disproportionately affected women trying to balance childcare, family care, and work responsibilities, we discovered that among patients in whom telehealth obviated arranging for childcare, the group was evenly divided between males and females (Table 4). While this group represented only a small population within our study, it suggests that the convenience of telehealth simplifying logistical issues likely plays a significant role in affecting patients’ overall satisfaction with telehealth.
The impact of descriptive patient characteristics
Patients’ overall scores with telehealth were favorable, with high mean and median TUQ scores greater than 3.00, the minimum score to identify as satisfied. This is consistent with other studies utilizing the TUQ with a Likert scale, with mean scores above the threshold for overall satisfaction.26,27 Additionally, factors that correlated with greater satisfaction, defined as a TUQ score greater than the overall median score, were identified based upon age, gender, ethnicity, technology adoption rates, childcare arrangement needs, travel distance, and commute time. Surprisingly, underlying comorbidities other than a history of OHT were not associated with significant differences in satisfaction among patients, even comparing between groups with zero comorbidities and 1 or more comorbidities. A higher frequency of patients with OHT were noted to reside more than 30 miles from their medical office (Table 4), which could contribute to their higher satisfaction rates with a more convenient healthcare option. Previous telehealth studies have also largely described overall satisfaction with telehealth, but our study is unique in that we utilized an objective and validated measure of patient satisfaction with telehealth to quantify the degree of satisfaction during the COVID-19 pandemic. Additionally, our study is strengthened by its larger sample size over a long time period during the beginning and middle phases of the COVID-19 pandemic. Our study, however, had a moderate survey response rate, as 14.1% of eligible patients completed the study survey. Several possibilities might explain this finding. Invitations to participate in the study were delivered via secure electronic messaging through the patient health portal. However, patients first receive a generic e-mail from UCLA Health notifying them that a new message is available for review. The patient must then log into the health portal and open the message to find the link to the study survey within the body of the text, and click again to open the survey in a browser on their computer or smartphone. These cumbersome steps to access the study might have contributed to a lower response rate and may explain why 18.2% of eligible patients did not even open the invitation message. Follow-up reminder e-mails were also not sent to eligible patients, which also may have lowered the survey response rate. Lastly, we did not offer compensation for study participation, which may have lowered our response rate, as participation was purely on a volunteer basis.
While other studies utilizing the TUQ questionnaire have been used in other specialties such as general surgery, otolaryngology, and dermatology during the COVID-19 pandemic, our study explored perspectives on satisfaction with telehealth in patients with a wide breadth of cardiovascular diseases with a large sample size. Our study also demonstrated consistent results of high satisfaction among patients with telehealth, similar to previously published studies during the COVID-19 pandemic, which is important for the broad applicability of telehealth utilization to treat and diagnose a wide range of medical diseases.27, 28, 29 Furthermore, we identified different factors associated with higher satisfaction among an already satisfied patient population. Our findings suggest that factors increasing patient convenience contribute significantly to greater satisfaction with telehealth, consistent with prior studies.30,31 Additionally, although data did not meet statistical significance, Medicaid patients comprised only a small percentage of the study cohort and had a very high proportion of patients with greater satisfaction. We surmise that this higher satisfaction may be related to factors such as improved access to healthcare or less time taken off from hourly-wage work, though further study—and with a larger patient population in a broader geographic region—is needed to explore this finding.
Limitations
Our study has several limitations. Despite the larger sample size, it may not have been adequately powered to detect statistically significant differences among groups utilizing telehealth. Additionally, given the high proportion of White patients participating in the study, satisfaction (or dissatisfaction) with telehealth for other races may be underrepresented in our study and may not be truly representative of patient demographics of the population at large. Given that our study was voluntary, with a lower response rate, it may be subject to participation (nonresponse) bias. While surveys with low response rates have historically been associated with a higher risk for nonresponse error, identifying when nonresponse introduces significant error that affects the results has been difficult to evaluate.25 It is possible that a voluntary survey may self-select for patients who generally are more technology savvy, satisfied with telehealth, or interested in the topic, and thus more likely to participate, but whether this alone is responsible for the differences among racial groups is unclear. Furthermore, our study findings may be incomplete, as other variables associated with greater satisfaction with telehealth might not have been identified. A recent study found that in rural Virginia, health literacy and access to internet were factors associated with satisfaction in telehealth, though they did not differentiate between synchronous 2-way audio-only or synchronous 2-way audio-video encounters.32 Our study required internet access to participate in both the telehealth encounter and follow-up satisfaction survey, and we did not formally assess health literacy in our trial. Additionally, our study population was in an urban metropolitan area, which may reflect different preferences that tie to a subjective variable such as satisfaction compared to other regions in the United States. Differences in satisfaction based on geographic location as well as the time point during the COVID-19 pandemic also require further study.
As telehealth became regularly adopted into clinical workflows, changes in satisfaction over time as telehealth experience deepened were not evaluated. The impact of telehealth during the early phase of the COVID-19 pandemic noted decreased utilization of procedures such as electrocardiogram, echocardiography, and stress testing, as well as emergency room visits during the pandemic, but utilization of these procedures has likely since increased; and whether satisfaction with telehealth changes over time with increasing familiarity or fatigue with the technology is presently unknown.33,34 Telehealth usage has cooled as the pandemic has continued. As of August 2020, telehealth has a general utilization rate of 21% of patient encounters in the ambulatory setting, compared to its peak in April 2020 at 69% of patient encounters, and long-term utilization rates of telehealth have not been established.35 Our study only utilized 1 telehealth platform among a broad range of telehealth options, and it was not designed to evaluate satisfaction across multiple platforms, where user interface, reliability, and experience can vary widely. Finally, the effect of telehealth on clinical outcomes compared to traditional in-office or facility-based medical care remains unknown.
Conclusion
Telehealth remains an integral component of healthcare delivery during the ongoing COVID-19 pandemic, and the widespread adoption of telehealth across multiple cardiovascular disease service lines will likely continue after the pandemic concludes. We have identified several factors in the telehealth experience that are associated with greater satisfaction, which include factors associated with patient convenience, along with female gender, younger age, non-White ethnicity, and history of OHT. Patient satisfaction is a traditional quality standard that will be important to continue prioritizing for improvement as telehealth transitions into standard of care. Further research into identifying and mitigating disparities in care, optimizing telehealth clinical workflows, developing methods to maximize patient and provider satisfaction, and measuring clinical outcomes will provide insight into how telehealth should integrate into the future of healthcare delivery. In its current iteration, it appears to be a safe, convenient, and highly satisfactory adjunct to the traditional model of in-person care.
Acknowledgments
The authors would like to thank the University of California, Los Angeles (UCLA) Clinical Translational Science Institute (CTSI), who provided statistical analysis supported by NIH/NCATS/UCLA CTSI Grant UL1TR001881
Data Statement
The data from this study are available upon request.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures
The authors have no conflicts to disclose.
Authorship
All authors attest they meet the current ICMJE criteria for authorship.
Patient Consent
All patients provided electronically signed informed consent.
Ethics Statement
The authors designed the study and gathered and analyzed the data according to the Helsinki Declaration guidelines on human research. The research protocol used in this study was reviewed and approved by the institutional review board.
References
- 1.WHO.int World Health Organization: Rolling updates on coronavirus disease (COVID-19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen Accessed September 16, 2020.
- 2.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 3.Dansky K.H., Vasey J., Bowles K. Impact of telehealth on clinical outcomes in patients with heart failure. Clin Nurs Res. 2008;17:182–199. doi: 10.1177/1054773808320837. [DOI] [PubMed] [Google Scholar]
- 4.Koehler F., Koehler K., Deckwart O., et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392:1047–1057. doi: 10.1016/S0140-6736(18)31880-4. [DOI] [PubMed] [Google Scholar]
- 5.Ong M.K., Romano P.S., Edgington S., et al. Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure. JAMA Intern Med. 2016;176:310. doi: 10.1001/jamainternmed.2015.7712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Medicare Telemedicine Health Care Provider Fact Sheet. CMS.gov. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Published 2020. Accessed September 16, 2020.
- 7.Adler-Milstein J., Kvedar J., Bates D.W. Telehealth among US hospitals: several factors, including state reimbursement and licensure policies, influence adoption. Health Aff (Millwood) 2014;33:207–215. doi: 10.1377/hlthaff.2013.1054. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Medicare and Medcaid Services COVID19 Emergency Blanket Waivers for Healthcare Providers. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf Accessed September 16, 2020.
- 9.Department of Health and Human Services Medicare Beneficiary Use of Telehealth Visits: Early Data from the Start of the COVID-19 Pandemic. https://aspe.hhs.gov/reports/aspe-issue-brief-medicare-beneficiary-use-telehealth-visits-early-data-start-covid-19-pandemic Accessed September 17, 2020.
- 10.Ramaswamy A., Yu M., Drangsholt S., et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22 doi: 10.2196/20786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohannessian R. Telemedicine: potential applications in epidemic situations. Eur Res Telemed / La Rech Eur en Télémédecine. 2015;4:95–98. [Google Scholar]
- 12.Ohannessian R., Duong T.A., Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6 doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gorodeski E.Z., Goyal P., Cox Z.L., et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020;26:448–456. doi: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bestsenny O., Gilbert G., Harrix A., Rost J. Telehealth: a quarter-trillion-dollar post-COVID-19 reality? McKinsey and Company, Healthcare Systems and Services. https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality# Accessed July 22, 2021.
- 15.Parmanto B., Lewis A.N., Jr., Graham K.M., Bertolet M.H. Development of the Telehealth Usability Questionnaire (TUQ) Int J Telerehabil. 2016;8:3–10. doi: 10.5195/ijt.2016.6196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hajesmaeel-Gohari S., Bahaadinbeigy K. The most used questionnaires for evaluating telemedicine services. BMC Med Inform Decis Mak. 2021;21:36. doi: 10.1186/s12911-021-01407-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iowa State College The Diffusion Process. 1957. Special Report 24. http://lib.dr.iastate.edu/specialreports/24
- 18.Eberly L.A., Khatana S.A.M., Nathan A.S., et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic. Circulation. 2020;142:510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eberly L.A., Kallan M.J., Julien H.M., et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yuan N., Pevnick J.M., Botting P.G., et al. Patient use and clinical practice patterns of remote cardiology clinic visits in the era of COVID-19. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jang M., Vorderstrasse A. Socioeconomic status and racial or ethnic differences in participation: web-based survey. JMIR Res Protoc. 2019;8 doi: 10.2196/11865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fischer S.H., Ray K.N., Mehrotra A., Bloom E.L., Uscher-Pines L. Prevalence and characteristics of telehealth utilization in the United States. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.22302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drake C., Zhang Y., Chaiyachati K.H., Polsky D. The limitations of poor broadband internet access for telemedicine use in rural America: an observational study. Ann Intern Med. 2019;171:382. doi: 10.7326/M19-0283. [DOI] [PubMed] [Google Scholar]
- 24.Rodriguez J.A., Saadi A., Schwamm L.H., Bates D.W., Samal L. Disparities in telehealth use among California patients with limited english proficiency. Health Aff. 2021;40:487–495. doi: 10.1377/hlthaff.2020.00823. [DOI] [PubMed] [Google Scholar]
- 25.Groves R.M., Presser S., Dipko S. The role of topic interest in survey participation decisions. Public Opin Q. 2004;68:2–31. [Google Scholar]
- 26.Xu J, Hamadi H, Hicks-Roof K, Zeglin R, Bailey C, Zhao M. Healthcare professionals and telehealth usability during COVID-19. Telehealth Med Today. Published online July 30, 2021. https://doi.org/10.30953/tmt.v6.270
- 27.Layfield E., Triantafillou V., Prasad A., et al. Telemedicine for head and neck ambulatory visits during COVID-19: evaluating usability and patient satisfaction. Head Neck. 2020;42:1681–1689. doi: 10.1002/hed.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mostafa PIN, Hegazy AA. Dermatological consultations in the COVID-19 era: is teledermatology the key to social distancing? An Egyptian experience. J Dermatolog Treat. Published online July 7, 2020. https://doi.org/10.1080/09546634.2020.1789046 [DOI] [PubMed]
- 29.Zhu C., Williamson J., Lin A., et al. Implications for telemedicine for surgery patients after COVID-19: survey of patient and provider experiences. Am Surg. 2020;86:907–915. doi: 10.1177/0003134820945196. [DOI] [PubMed] [Google Scholar]
- 30.Kruse C.S., Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Donelan K., Barreto E.A., Sossong S., et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25:40–44. [PubMed] [Google Scholar]
- 32.Thomson M.D., Mariani A.C., Williams A.R., Sutton A.L., Sheppard V.B. Factors associated with use of and satisfaction with telehealth by adults in rural Virginia during the COVID-19 pandemic. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.19530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wosik J., Clowse M.E.B., Overton R., et al. Impact of the COVID-19 pandemic on patterns of outpatient cardiovascular care. Am Heart J. 2021;231:1–5. doi: 10.1016/j.ahj.2020.10.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cox C., Amin K., Kamal R. How have health spending and utilization changed during the coronavirus pandemic? Peterson-KFF Health System Tracker. https://www.healthsystemtracker.org/chart-collection/how-have-healthcare-utilization-and-spending-changed-so-far-during-the-coronavirus-pandemic/#item-covidcostsuse_marchupdate_5 Published 2021. Accessed August 18, 2021.
- 35.Fox B., Sizemore J.O. Telehealth: Fad or the Future. Epic Health Research Network. https://www.ehrn.org/wp-content/uploads/telehealth-fad-future.pdf Published 2020.