Abstract
Objectives:
To evaluate whether childhood emotional and behavioral characteristics are associated with soda intake.
Methods:
The study population included 391 Mexico City adolescents enrolled in a birth cohort study. When children were between 6 and 12 years (y) of age, the Behavioral Assessment System for Children (BASC)-II was administered. Non-diet soda intake was measured concurrently and again when participants were of peri-pubertal ages via food frequency questionnaire. Linear regression models were run with soda mL/day (cross-sectional and change in soda over time) as the outcome and BASC composite scores as predictors (in separate models), adjusting for confounders.
Results:
At baseline, children were 8.3 (SD 1.3) years (49% males). Three scales out of 18 examined had statistically-significant associations. Parent-reported Adaptive Skills were inversely associated with concurrent soda intake (β=−2.29 with 95% CI −4.27 to −0.31). Parent-reported Internalizing Problems (higher=more problems) were related to higher change in soda intake from childhood to adolescence (β=5.83 with 95% CI 0.98 to 10.68; N=191). Self-reported School Problems were associated with a higher change in soda intake over time (β=9.46 with 95% CI 2.10 to 16.82; N=122).
Conclusions:
Parent- and self-reported emotional and behavioral difficulties in childhood were associated with soda consumption and changes in soda consumption over time.
Keywords: Mental health, SSB, soda, comfort eating
Introduction
Overconsumption of sugar-sweetened beverages (SSB) in pediatric populations is a critical public health concern, as SSB consumption has been linked with adverse health effects including obesity1, diabetes2, early age at menarche3, asthma4 and cardiometabolic disturbances5. Moreover, early SSB consumption habits may track into adulthood; thus, reducing intake of SSB in childhood may be important not only for prevention of health outcomes in the short-term but also to foster healthy SSB habits throughout life. Currently, one of the populations most at risk for overconsumption of SSB is the Mexican population, where adolescents on average obtain 20% of their energy intake from calorie-containing beverages5.
Multiple contextual factors may play a role in excessive SSB intake, including socioeconomic status (SES)6, parental practices7–10, screen time11–13, self-efficacy14, unreliable drinking water, and school, family, and neighborhood food environments8,10,15–17. One area that remains underexplored is whether emotional and behavioral difficulties could predispose youth to higher SSB intake. An association is plausible, as recent studies in children <6 years have linked internalizing behavior (acting withdrawn, depressed, anxious) and externalizing behaviors (showing aggression, anger, impulsivity) with greater consumption of foods high in added sugar and/or sodium18,19. One potential explanation is through parental behaviors, as parents may use food to calm or pacify children when distressed or when they show disruptive behavior20. Children may also watch parents model the use of food or drink to self-regulate21. As children get older and can obtain foods and drinks high in added sugar or sodium more easily22, children with emotional or behavioral difficulties may seek out such foods and/or SSBs as a way to self-calm when they feel stressed 23,24. Studies in children >6 years have also reported associations between emotional and behavioral difficulties with greater consumption of foods high in sugar, sodium, and fat. For example, a study among Australian adolescents found that higher internalizing and externalizing behaviors associated with lower-quality diets, including a dietary pattern high in soft drinks25.
Overall, while there is substantial evidence of links between certain behavior and intake of unhealthy foods in children and adolescents, few previous studies have considered whether children with emotional and behavioral difficulties have higher SSB intake in particular. It is important to examine SSBs specifically because SSB consumption is a distinct dietary behavior (e.g. not necessarily tied to a particular meal or time of day), and SSBs may be more readily available than other types of so-called junk foods. One cross-sectional Iranian study of children ages 6 to 18 years examined mental health correlates in relation to SSB consumption as well as other junk foods, and found different associations with SSBs versus salty snacks26. They showed that higher SSB consumption was associated with markers of psychiatric distress, while higher salty snack consumption was associated with aggressive behavior. One of the main limitations of this study was its cross-sectional nature, which precludes examining whether behaviors preceded SSB intake or vice versa, and how these associations tracked over time.
We sought to examine whether emotional and behavioral difficulties were associated with SSB intake in the context of Mexico, where SSBs are widely available and frequently consumed. In particular, we aimed to evaluate whether emotional and behavioral difficulties measured during childhood (ages 8 to 12 years) were associated with 1) soda intake measured at the same time (henceforth called concurrent intake), and 2) change in soda intake from childhood to adolescence.
Methods
Study Population
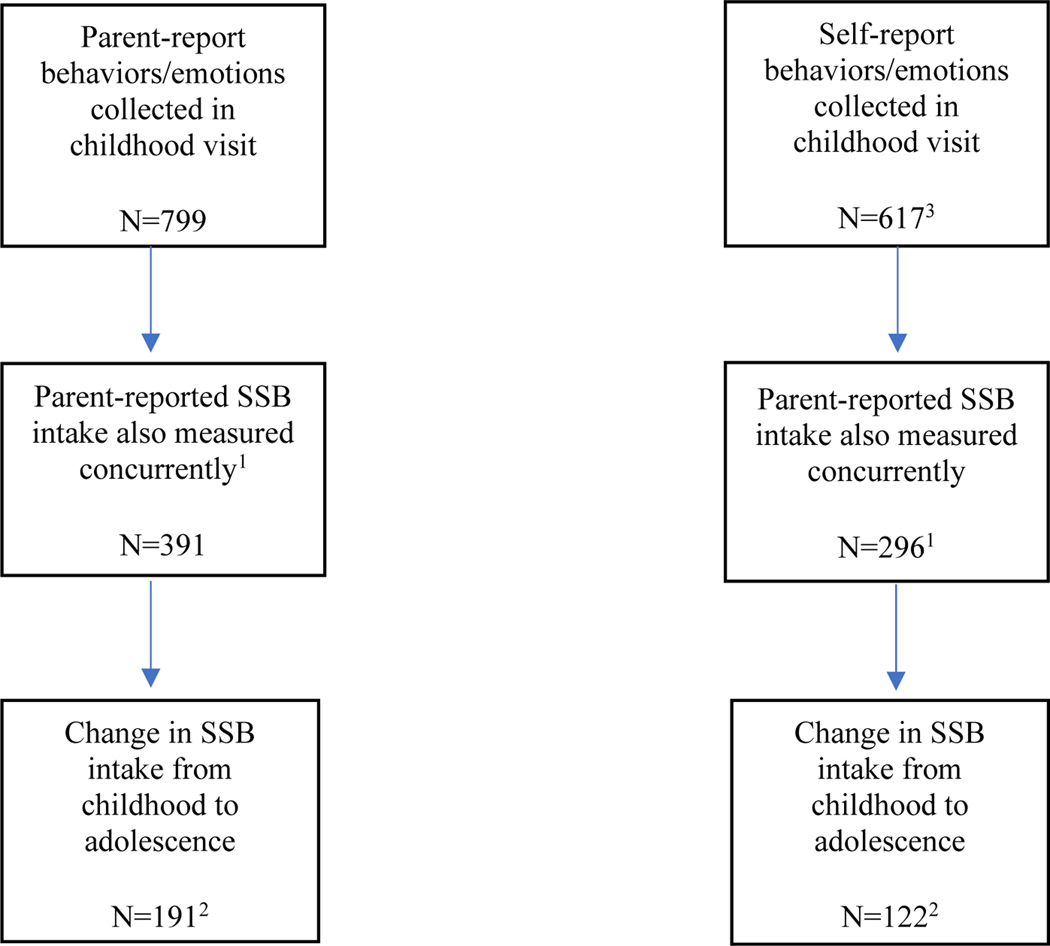
The study population was drawn from two birth cohorts of mother–infant pairs enrolled in Mexico City, Mexico, starting in 1997 and 2001, as part of the Early Life Exposure in Mexico to ENvironmental Toxicants (ELEMENT) study, which is described in greater detail elsewhere27. Briefly, in both cohorts pregnant women were initially recruited from prenatal clinics of the Mexican Social Security Institute in Mexico City, which serves a low- to middle-income population formally employed in the private sector. Throughout the course of the study, researchers have gathered information on the children’s environmental exposures, lifestyle, and dietary factors as well as measures of growth and development. From 2008 to 2012, when children were between 6 and 12 years of age, parental- and self- ratings of children’s emotional and behavioral adjustment were collected for 799 children (hereafter called the childhood visit). During the childhood visit, parents completed a food frequency questionnaire regarding the children’s dietary habits. The food frequency questionnaire was completed by the children themselves (with input from the primary caregivers) in a follow-up visit that occurred starting in 2015 when they were between 9 and 17 years old (hereafter called the adolescent visit; n=550). The present study thus utilized data from the childhood and adolescent follow-up visits, with varying sample sizes (see Figure 1). Sociodemographic characteristics were similar across the various analytic samples.
Figure 1. Flow chart of sample sizes in analytic samples.
1 Administration of the food frequency questionnaire began in the latter half of the 2008 visit
2 Only 550 of the original 799 children were followed up during the 2015 visit. These children did not differ with respect to sex, age, BMI, mother’s marital status, or mother’s education.
3 All children who filled out the self-reported BASC-2 except for 7 also had parental BASC-2 reports. Children had to be 8 years old or older to fill out the self-reported BASC-2.
Exposure: Parental and Self-rated Emotional and Behavioral Difficulties during Childhood (2008–2012)
Emotional and behavioral difficulties were measured during the childhood visit by the Behavior Assessment Scale for Children-2 (BASC-2), which has been adapted for Spanish speakers28. The BASC-2 is a multidimensional behavior rating system to assess clinical and adaptive features of emotional and behavioral adjustment in children, and includes questions concerning typical behaviors (e.g., trouble sitting still) and emotions (e.g., worry about what is going to happen). We administered the parent questionnaire as well as the child questionnaire (only for children aged ≥8 years during the visit). Responses were either based on a 4-point frequency scale (ranging from “never” to “almost always”) or were true/false. From the parental responses, age and sex-standardized T-scores (ranging from 0–100, with a score>60 typically indicating some difficulties) are provided for nine clinical scales, five adaptive scales, and four composite scores that combine particular clinical or adaptive scales (see Table 1). We examined four composite scores as our primary exposures: Externalizing Problems, Internalizing Problems, Behavioral Symptoms Index, and Adaptive skills. From child responses, age and sex-standardized T-scores (ranging from 0–100, with a score>60 typically indicating some difficulties) are provided for ten clinical scales, four adaptive scales, and five composite scores that combine particular clinical or adaptive scales (see Table 1). For the present analysis, we examined the five composite scores: School Problems, Internalizing Problems, Inattention/Hyperactivity, Emotional Problems, and Personal Adjustment. In each of the parent and child composites, higher scores indicate greater emotional or behavioral difficulties, except for Adaptive Skills and Personal Adjustment (higher scores=more adaptive behavior). While the BASC-2 composite scores were our primary exposure, in supplemental analysis we also examined the parental and child individual scales. See Supplemental Table 1 for Spearman correlations of scales that were similar across parent and child-reported scales. In general, correlations were positive but fairly weak magnitude.
Table 1.
Individual scales included in BASC-2 composites
| Composites | Individual scales that make up composite | Cronbach’s Alpha1 |
|---|---|---|
|
| ||
| Parent-reported | ||
| Adaptive Skills | Adaptability, Activities of Daily Living, Functional Communication, Social Skills, Leadership | 0.89 |
| Behavioral Symptoms Index | Hyperactivity, Aggression, Depression, Attention Problems, Atypicality, Withdrawal | 0.84 |
| Externalizing Problems | Hyperactivity, Aggression, Conduct Problems | 0.86 |
| Internalizing Problems | Anxiety, Depression, Somatization | 0.68 |
| Self-reported | ||
| School Problems | Attitude to School, Attitude to Teachers, Sensation Seeking2 | 0.52 |
| Internalizing | Atypicality, Locus of Control, Social Stress, Anxiety, Depression, Sense of Inadequacy, Somatization2 | 0.89 |
| Inattention | Inattention, Hyperactivity | 0.93 |
| Personal Adjustment | Relations with Parents, Interpersonal Relations, Self-Esteem, Self-Reliance | 0.25 |
| Emotional Symptoms | Social Stress, Anxiety, Depression, Sense of Inadequacy, Self-Esteem, Self-Reliance | 0.51 |
Using the data from this study
Only included in composite scores for children 12 years or older
Outcome: Soda intake during childhood and adolescence
Information on usual soda consumption was obtained from a food frequency questionnaire validated for the Mexican population29 during the childhood visit as well as the adolescent visit. Participants or their caregivers were asked how often they typically consumed one standard serving size of regular soda (non-diet) in the past month (childhood visit) or in the previous seven days (adolescent visit). The response options included the number of days per week (from 0 to 7), times per day (1 to 6), serving size (1 glass of 240 per each serving), and number of servings consumed of soda. The number of servings/week was then multiplied by the standard serving size (240mL) item, and then divided by seven to obtain average daily intakes (beverages, mL/d). For analysis, soda intake was treated as a continuous variable. We decided a priori to use soda intake rather than total SSB in the diet. The other SSB most commonly consumed in this population is fresh fruit juice with added sugar (commonly called “aguas frescas”), which is typically hand-made and thus harder to recall accurately (and the added sugar content is not uniform). In addition, the health risks and benefits are not as well understood as bottled soda, as these juice drinks usually contain fresh fruit.
Potential confounders
During the original recruitment visit, mothers provided information on highest education received and marital status. During the childhood visit, child anthropometric measurements (height in cm and weight in kg) were taken by a trained research assistant using calibrated instruments, and BMI-for-age z scores were calculated using the WHO reference30. Covariates were categorized as shown in Table 2.
Table 2.
Mean soda consumption at baseline, according to sociodemographic characteristics of 391 Mexican children
| Daily soda consumption at baseline | ||||
|---|---|---|---|---|
| Baseline Characteristics | All n(%) | Mean(mL) | SD | P-value |
|
| ||||
| Total | 391 | 176.39 | 198.75 | |
| Sex | 0.0008 | |||
| Male | 197 | 209.63 | 223.25 | |
| Female | 194 | 142.64 | 164.11 | |
| Age | 0.001 | |||
| 6 to <8 y | 103 | 136.73 | 152.64 | |
| 8 to <10 y | 122 | 158.22 | 188.92 | |
| 10 to <12 y | 166 | 214.36 | 223.86 | |
| BMI-for age z scores | 0.52 | |||
| <−1 | 23 | 160.99 | 138.09 | |
| −1 to 0 | 80 | 181.07 | 209.72 | |
| 0 to <1 | 115 | 172.29 | 188.65 | |
| >1 | 156 | 190.11 | 214.31 | |
| Mother’s marital status | 0.37 | |||
| Married or civil union | 337 | 180.98 | 203.53 | |
| Single, separated, divorced, or widowed | 32 | 148.66 | 179.61 | |
| Mother’s education | 0.04 | |||
| Did not complete secondary (<9) | 61 | 238.10 | 226.53 | |
| Completed some high school (9 to <12) | 154 | 157.40 | 169.65 | |
| Completed high school (12) | 108 | 192.38 | 235.38 | |
| Higher education (>12) | 44 | 121.56 | 145.08 | |
Data analysis
To describe the study population and to assess potential confounders, we first calculated average ± SD SSB intake at baseline and at the follow-up visit, stratified by categories of baseline sociodemographic and anthropometric characteristics.
To test the first aim, we used linear regression models with continuous soda intake at baseline as the outcome and concurrent BASC composite T-scores (Externalizing Problems, Internalizing Problems, and Adaptive skills for parent-report and School Problems, Internalizing Problems, Inattention/Hyperactivity, and Personal Adjustment for child-report) as continuous predictors, each in separate models. To evaluate non-linear relations, we categorized each of the composite scores into quintiles and entered them into regression models as indicator variables. Because there was evidence of linear trends, we show all results with continuous composite T-scores. To account for potential confounding, we adjusted for maternal education, maternal marital status, and sex and age (although the composite T-scores were standardized for sex and age, these variables were still associated with the T-scores) in all linear regression models. Inclusion of baseline child BMI-for-age z scores did not alter estimates and were thus not included in final models.
The analytic strategy of the second aim was identical except for the outcome which was continuous change in soda intake from childhood to adolescence (positive values indicating higher soda intake in adolescence compared to childhood). Exclusion of 2 participants who were <10 years (9.8 and 9.9 years) in the adolescent visit did not alter findings; thus, these participants were retained. To further interpret results from the composite scores, additional analyses using the individual clinical scores were also conducted for each aim (both parent and self-reported BASC-2 measures) and provided in supplementary material. Sensitivity analyses using a square root transformation of baseline soda intake were conducted. Analyses were conducted in SAS version 9.4, and P-values <0.05 were considered statistically significant.
Results
Mean age of children at baseline was 8.3 y (SD 1.3), and 49% were male. The average length of follow-up from the childhood visit to the adolescent visit was 6.4 ± 1.2 years. The mean (SD) soda consumption at baseline was 176.39 ml (198.75) with a mean change of 111.90 (355.48) mL from baseline to follow-up. Males tended to consume more soda than females, older adolescents drank more soda than younger adolescents, and adolescents whose mother had lower education had higher consumption of soda (Table 2). BMI for age z scores were not associated with soda intake.
Mean scores for the parent-reported composite scores were 49.4 (SD 9.7), 52.3 (SD 9.6), and 47.0 (SD 10.7) for Externalizing Problems, Internalizing Problems, and Adaptive Skills, respectively. For self-reported composite scores, they were 50.6 (SD 9.7), 50.3 (SD 8.9), 53.1 (SD 10.4), and 49.1 (SD 8.9) for School Problems, Internalizing Problems, Inattention/Hyperactivity, and Personal Adjustment, respectively.
Concurrent Soda Intake
For parent-reported composite scores, Adaptive Skills was statistically significantly related to soda intake, such that each point higher parent-rated Adaptive Skills was associated with 2.29 mL lower soda intake in childhood (95% CI −4.27 to −0.31, p-value=0.02; Table 3). In addition, some individual factors - Aggression and Somatization- were positively associated with concurrent soda intake (Supplemental Table 2). To highlight, each point higher Aggression T-score was related to 2.57 mL/day higher soda intake (95% CI 0.34 to 4.80; p value=0.02), and each point higher Somatization score was associated with 1.79 mL/day higher soda intake (95% CI 0.03 to 3.54; p value=0.046).
Table 3.
Associations between concurrent childhood BASC composite scores and soda intake of Mexican youth aged 6–12 years
| Unadjusted model | Adjusted Model1 | |||||
|---|---|---|---|---|---|---|
| β | 95% CI | P value | β | 95% CI | P value | |
|
| ||||||
| Parent-reported behavior (N=391) | ||||||
| Externalizing Problems | 1.97 | −0.06, 4.00 | 0.06 | 1.13 | −0.99, 3.27 | 0.30 |
| Internalizing Problems | 0.72 | −1.12, 2.57 | 0.44 | 0.72 | −1.20, 2.63 | 0.46 |
| Behavioral Symptoms Index | 2.37 | 0.40, 4.34 | 0.018 | 1.72 | −0.34, 3.78 | 0.10 |
| Adaptive skills2 | −3.09 | −4.93, −1.26 | 0.001 | −2.29 | −4.27, −0.31 | 0.02 |
| Self-reported behavior (N=296) | ||||||
| School problems | 0.88 | −1.62, 3.39 | 0.49 | 1.12 | −1.38, 3.62 | 0.38 |
| Internalizing problems | −1.77 | −4.48, 0.94 | 0.2 | −1.73 | −4.47, 1.01 | 0.21 |
| Inattention/Hyperactivity | 0.07 | −2.26, 2.40 | 0.95 | 0.06 | −2.24, 2.35 | 0.96 |
| Emotional symptoms index | −2.33 | −4.99, 0.34 | 0.09 | −2.38 | −5.09, 0.38 | 0.09 |
| Personal adjustment2 | 2.44 | −0.27, 5.15 | 0.08 | 2.22 | −0.55, 4.99 | 0.12 |
Adjusted analysis for child sex, child age, mother’s marital status and mother’s education
Higher scores indicate more adaptive behavior
Of the self-reported emotion and behavior measures, none were statistically significantly related to concurrent soda intake in either unadjusted or adjusted models. Square root transformation of the soda intake outcome did not substantially alter the direction or statistical significance of the findings.
Change in soda intake over time
Table 4 shows the associations between parent-reported behaviors and emotions with change in soda intake from childhood to adolescence. Of the composite scores, Internalizing Problems was the only statistically significant predictor. Each point higher Internalizing Problems was associated with 5.83 mL/day higher soda intake (95% CI 0.98 to 10.68; p value= 0.02). Of the individual factors that make up Internalizing Problems, the two with the highest magnitude were Somatization- with 5.80 mL/day higher soda intake per each Somatization point (95% CI 1.30 to 10.30; p value=0.01; Supplemental Table 3)- and Anxiety- with 4.64 mL/day higher soda intake per point (95% CI −0.12 to 9.40; p value= 0.056). Aggression was also associated with change in soda intake, such that every higher point on the Aggression scale was associated with 6.02 mL/day greater intake (95% CI 0.10 to 11.95; p value=0.046).
Table 4.
Associations between childhood BASC composite scores and change in soda intake over time (from ages 6–12 to ages 9–17) of Mexican youth
| Change in soda intake, Unadjusted | Change in soda intake, Adjusted1 | |||||
|---|---|---|---|---|---|---|
| β | 95% CI | P value | β | 95% CI | P value | |
|
| ||||||
| Parent-reported behavior (N=191) | ||||||
| Externalizing Problems | 4.21 | −1.03, 9.45 | 0.11 | 3.17 | −2.18, 8.52 | 0.24 |
| Internalizing Problems | 5.32 | 0.53, 10.11 | 0.03 | 5.83 | 0.98, 10.68 | 0.02 |
| Behavioral Symptoms Index | 2.90 | −2.21, 8.02 | 0.26 | 2.34 | −2.83, 7.52 | 0.37 |
| Adaptive skills2 | −2.49 | −7.25, 2.26 | 0.30 | −2.28 | −7.14, 2.58 | 0.36 |
| Self-reported behavior (N=122) | ||||||
| School problems | 10.14 | 2.51, 17.77 | 0.01 | 9.46 | 2.10, 16.82 | 0.01 |
| Internalizing problems | 9.00 | −0.06, 18.07 | 0.052 | 6.95 | −2.16, 16.06 | 0.13 |
| Inattention/Hyperactivity | 4.29 | −2.91, 11.50 | 0.24 | 5.70 | −1.35, 12.75 | 0.11 |
| Emotional symptoms index | 7.93 | −0.84, 16.71 | 0.076 | 7.31 | −1.42, 16.04 | 0.10 |
| Personal adjustment2 | −7.27 | −15.84, 1.30 | 0.096 | −4.22 | −12.81, 4.37 | 0.33 |
Adjusted analysis for child sex, child age, mother’s marital status and mother’s education
Higher scores indicate more positive behavior
Among self-reported measures, there was one significant composite score, School Problems. Each point higher School Problems score was related to 9.46 mL/day higher soda intake (95% CI 2.10 to 16.82; p value=0.01). The individual factors Attitude to School and Attitude to Teacher were also associated with change in soda intake (Supplemental Table 3). Each point higher Attitude to School was associated with 11.30 mL/day higher soda intake (β=11.30 with 95% CI 2.23 to 20.36; p value=0.015), while each point higher Attitude to Teacher was associated with 5.85 mL/day higher soda intake (95% CI −0.15 to 11.85; p value=0.056).
Discussion
In this prospective study of Mexico City youth, we found that childhood emotional and behavioral difficulties predicted concurrent soda consumption, as well as change in soda consumption over a 6-year time frame. Specifically, parent-reported Adaptive Skills were related to concurrent soda intake, while parent-reported Internalizing Problems and self-reported School Problems were associated with higher change in soda intake over time. Of the individual scales, parent-reported aggression was also associated with both concurrent soda and change in soda intake. The magnitude of several of these findings were of public health relevance; in particular, a child with a 10 points higher School Problems T-score would be expected to consume 2.5 more servings of soda per week in adolescence compared to the childhood visit.
Overall, these findings are in line with prior studies that link emotional and behavioral difficulties with consumption of highly palatable foods (“comfort foods” or junk food) or with particular nutrients like sodium or added sugar18,19,25,26. A study of Michigan preschoolers found that boys with higher externalizing behavior (marked by aggressive behavior) had higher intake of added sugar one year later, while girls with higher externalizing behavior had higher intake of sodium18. Other prospective studies in Norwegian preschoolers and Australian adolescents have linked internalizing and externalizing symptoms with higher sugar intake or less-healthy dietary patterns19,25. Our study extends previous work for a few reasons: first, most prior studies have not specifically examined soda or SSB intake. Focusing on SSB intake is salient from a public health perspective because SSB intake is a distinct dietary behavior, and many interventions specifically target it. In addition, few studies have used a prospective study design18,19, and we are aware of no studies that assessed change in soda intake over time.
There are a few potential mechanisms to explain the findings for internalizing problems and aggressive behavior. The first is that children may manage their negative emotions and stress through consumption of sweet beverages. Sugar has been hypothesized to reduce distress, and been shown to be physiologically calming in prior work32. Other studies support a link between emotional difficulties and overall emotional eating, although not sugar per se. One study among 170 pre-school children showed that maternal and child internalizing symptoms were reported to predict adolescent emotional eating33. Another potential mechanism may be related to poor sleep, since emotional and behavioral difficulties are often comorbid with (or follow) sleep problems in children and adolescents35, and short sleep duration and lower quality sleep are associated with higher SSB intake among children and adolescents36.
Self-reported school problems arose as an important composite score predictor of change in soda intake over time. This finding aligns with a study from Taiwan, where it was reported that children with unfavorable school performance were more likely to eat sweets and fried foods and were less likely to eat foods rich in protein, vitamins, and minerals37. In addition, internalizing problems, such as depression38,39 and anxiety40,41 have been reported to have an impact on school performance. Thus, one possible explanation is that self-reports of school problems, which may be more concrete, are also capturing some aspect of internalizing difficulties, which can be difficult to assess in children42. School problems could also reflect inattention and hyperactivity issues. In work that examined this construct in relation to diet and eating, attention deficit hyperactivity disorder symptoms were associated with uncontrolled eating habits43, food responsiveness44, and emotional overeating44 in children.
The concurrent behavior-soda associations were different from the relationships between behavior and change in soda over time, with the exception of parent-reported aggression. One explanation is that associations become more apparent in adolescence as youth gain greater autonomy over food choices. Indeed, the overall intake of soda increased on average from the adolescent visit compared to the childhood visit. Further, emotional stress and pressure tends to increase around the time of puberty45; this could also help to explain why certain relationships only appeared later on. It is important to note that we did not have repeated measures of behavior and emotions. Thus, although we know that baseline BASC measures predicted change in soda intake, we cannot assume that behavioral and emotional symptoms remained constant over the follow-up period. Future analyses that examine whether particular trajectories of behavioral and emotional symptoms over time (e.g. continually increasing symptoms over childhood and adolescence) are more highly predictive of changes in soda intake would be especially informative.
The directionality of these associations is also worth mentioning. Although we explored whether emotional and behavioral symptoms during childhood were prospectively related to soda intake change, we cannot preclude the possibility that soda intake could predict changes in behavioral or emotional symptoms. Bidirectional relationships between emotional and behavioral characteristics and soda intake could also exist, such that behavioral/emotional symptoms cause an increase in soda consumption, and the higher soda consumption leads to more emotional/behavioral symptoms. Future research that measures both emotional/behavioral symptoms and soda intake on a repeated basis is needed to uncover these nuances.
There are multiple strengths of this study. One important strength of this study is connecting emotional and behavioral factors specifically to soda intake, which provides a new perspective to reduce SSB intake among children and adolescents. The longitudinal nature of the study is another strength. However, there are several limitations. First of all, sample sizes were fairly small for the change in soda intake analyses. Second, we did not have measurements of BASC at follow-up to assess change in emotional and behavioral difficulties over time, or to evaluate possible bidirectional associations between soda and BASC composite measures. Third, the fact that the dietary data and over half of the BASC measures were self-reported means that there could be recall bias. Of note, prospective associations with internalizing problems (the two constructs most closely aligned between parent and self-reports) were in the same direction for both the parent-reported measure and self-reported measure. Given that these constructs were measured independently, the consistent findings speak to the internal validity of the measures. Fourth, there were some missing data for maternal education, one of the confounders; thus, the fully adjusted analysis had slightly smaller sample sizes. Fifth, Cronbach’s alpha levels were fairly low for three of the BASC scale- Personal Adjustment, Emotional Symptoms, and School Problems- indicating low reliability. Finally, the range of ages present in the adolescent visit could mean there was variability in the ability to accurately report dietary intake; yet, the younger adolescents were often aided by a parent.
In summary, this study examined whether emotional and behavioral factors were associated with cross-sectional and prospectively-assessed changes in soda intake in Mexican youth. Parent-reported Adaptive skills were associated with lower soda intake concurrently, while the constructs School Problems, Internalizing Problems, and aggression were associated with greater change in soda intake from childhood to adolescence. Findings from this study provide new perspectives on factors that could predispose adolescents to excessive SSB intake, and may suggest that targeted interventions are needed to help children with emotional and behavioral difficulties to reduce their SSB consumption. This may be particularly relevant within the contexts of environments where SSBs are widely accessible, such as in Latin America and in lower SES neighborhoods in the US.
Supplementary Material
Acknowledgements:
We gratefully acknowledge the American British Cowdray (ABC) Medical Center for the use of their research facilities.
Conflict of Interest: The authors report grants from NIEHS/EPA (R01ES0007821 and P01ES022844/RD83543601) during the conduct of the study. Dr. Jansen reports postdoctoral support from the NIDDK (T32DK071212). The funders had no role in the present work.
References
- 1.Massougbodji J, Le Bodo Y, Fratu R, De Wals P. Reviews examining sugar-sweetened beverages and body weight: Correlates of their quality and conclusions. Vol. 99, American Journal of Clinical Nutrition. 2014. p. 1096–104. [DOI] [PubMed] [Google Scholar]
- 2.Malik VS, Hu FB. Sweeteners and risk of obesity and type 2 diabetes: The role of sugar-sweetened beverages. Curr Diab Rep. 2012;12(2):195–203. [DOI] [PubMed] [Google Scholar]
- 3.Carwile JL, Willett WC, Spiegelman D, Hertzmark E, Frazier AL, Michels KB. Sugar-sweetened beverage consumption and age at menarche in a prospective study of US girls. Hum Reprod [Internet]. 2015;30(3):1–9. Available from: http://humrep.oxfordjournals.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park S, Blanck HM, Sherry B, Jones SE, Pan L. Regular-Soda Intake Independent of Weight Status Is Associated with Asthma among US High School Students. J Acad Nutr Diet [Internet]. 2013;113(1):106–11. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=2011794789&site=ehost-live&scope=cite [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barquera S, Hernandez-Barrera L, Tolentino ML, et al. Energy Intake from Beverages Is Increasing among Mexican Adolescents and Adults. J Nutr [Internet]. 2008;138(12):2454–61. Available from: http://jn.nutrition.org/cgi/doi/10.3945/jn.108.092163 [DOI] [PubMed] [Google Scholar]
- 6.Han E, Kim TH, Powell LM. Beverage consumption and individual-level associations in South Korea. BMC Public Health. 2013;13(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hennessy M, Bleakley A, Piotrowski JT, Mallya G, Jordan A. Sugar-Sweetened Beverage Consumption by Adult Caregivers and Their Children: The Role of Drink Features and Advertising Exposure. Heal Educ Behav. 2015;42(5):677–86. [DOI] [PubMed] [Google Scholar]
- 8.Bogart LM, Elliott MN, Ober AJ, et al.Home Sweet Home: Parent and Home Environmental Factors in Adolescent Consumption of Sugar-Sweetened Beverages. Acad Pediatr. 2017;17(5):529–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pinket AS, De Craemer M, De Bourdeaudhuij I, et al. Can parenting practices explain the differences in beverage intake according to socio-economic status: The toybox-study. Nutrients. 2016;8(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Ansem WJC, Van Lenthe FJ, Schrijvers CTM, Rodenburg G, Van De Mheen D. Socio-economic inequalities in children’s snack consumption and sugar-sweetened beverage consumption: The contribution of home environmental factors. Br J Nutr. 2014;112(3):467–76. [DOI] [PubMed] [Google Scholar]
- 11.Han E, Powell LM. Consumption Patterns of Sugar-Sweetened Beverages in the United States. J Acad Nutr Diet. 2013;113(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kenney EL, Gortmaker SL. United States Adolescents’ Television, Computer, Videogame, Smartphone, and Tablet Use: Associations with Sugary Drinks, Sleep, Physical Activity, and Obesity. J Pediatr. 2016/December/19. 2017;182:144–9. [DOI] [PubMed] [Google Scholar]
- 13.Larson N, Laska MN, Story M, Neumark-Sztainer D. Sports and energy drink consumption are linked to health-risk behaviours among young adults. Public Heal Nutr. 2015/February/17. 2015;18(15):2794–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bruce MA, Beech BM, Thorpe RJ, Griffith DM. Racial disparities in sugar-sweetened beverage consumption change efficacy among male first-year college students. Am J Mens Health. 2016;10(6):N168–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luszczynska A, de Wit JBF, de Vet E, et al. At-Home Environment, Out-of-Home Environment, Snacks and Sweetened Beverages Intake in Preadolescence, Early and Mid-Adolescence: The Interplay Between Environment and Self-Regulation. J Youth Adolesc. 2013;42(12):1873–83. [DOI] [PubMed] [Google Scholar]
- 16.Lebel A, Morin P, Robitaille É, Lalonde B, Florina Fratu R, Bisset S. Sugar Sweetened Beverage Consumption among Primary School Students: Influence of the Schools’ Vicinity. J Environ Public Health. 2016;2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shi L The association between the availability of sugar-sweetened beverage in school vending machines and its consumption among adolescents in california: A propensity score matching approach. J Environ Public Health. 2010;2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jansen EC, Miller AL, Lumeng JC, et al. Externalizing behavior is prospectively associated with intake of added sugar and sodium among low socioeconomic status preschoolers in a sex-specific manner. Int J Behav Nutr Phys Act. 2017;14(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vollrath ME, Stene-Larsen K, Tonstad S, Rothbart MK, Hampson SE. Associations between temperament at age 1.5 years and obesogenic diet at ages 3 and 7 years. J Dev Behav Pediatr. 2012;33(9):721–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gubbels JS, Kremers SPJ, Stafleu A, et al. Diet-related restrictive parenting practices. Impact on dietary intake of 2-year-old children and interactions with child characteristics. Appetite. 2009;52(2):423–9. [DOI] [PubMed] [Google Scholar]
- 21.Frankel LA, Hughes SO, O’Connor TM, Power TG, Fisher JO, Hazen NL. Parental influences on children’s self-regulation of energy intake: Insights from developmental literature on emotion regulation. Vol. 2012, Journal of Obesity. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reicks M, Banna J, Cluskey M, et al. Influence of parenting practices on eating behaviors of early adolescents during independent eating occasions: Implications for obesity prevention. Vol. 7, Nutrients. 2015. p. 8783–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melbye EL, Bergh IH, Hausken SES, et al. Adolescent impulsivity and soft drink consumption: The role of parental regulation. Appetite. 2016;96:432–42. [DOI] [PubMed] [Google Scholar]
- 24.Wills TA, Isasi CR, Mendoza D, Ainette MG. Self-Control Constructs Related to Measures of Dietary Intake and Physical Activity in Adolescents. J Adolesc Heal. 2007;41(6):551–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oddy WH, Robinson M, Ambrosini GL, et al. The association between dietary patterns and mental health in early adolescence. Prev Med (Baltim). 2009;49(1):39–44. [DOI] [PubMed] [Google Scholar]
- 26.Zahedi H, Kelishadi R, Heshmat R, et al. Association between junk food consumption and mental health in a national sample of Iranian children and adolescents: The CASPIAN-IV study. Nutrition. 2014;30(11–12):1391–7. [DOI] [PubMed] [Google Scholar]
- 27.Hu H, Téllez-Rojo MM, Bellinger D, et al. Fetal lead exposure at each stage of pregnancy as a predictor of infant mental development. Environ Health Perspect. 2006;114(11):1730–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kamphaus RW, VanDeventer MC, Brueggemann A, Barry M. Behavior Assessment System for Children-Second Edition [Internet]. The clinical assessment of children and adolescents A practitioners handbook. 2004. 311–326 p. Available from: http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,url,cookie,uid&db=psyh&AN=2006-11859-018&site=ehost-live [Google Scholar]
- 29.Denova-Gutiérrez E, Ramírez-Silva I, Rodríguez-Ramírez S, Jiménez-Aguilar A, Shamah-Levy T, Rivera-Dommarco JA. Validity of a food frequency questionnaire to assess food intake in Mexican adolescent and adult population. Salud Publica Mex [Internet]. 2016;58(6):617. Available from: http://www.saludpublica.mx/index.php/spm/article/view/7862 [DOI] [PubMed] [Google Scholar]
- 30.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bridle-Fitzpatrick S Food deserts or food swamps?: A mixed-methods study of local food environments in a Mexican city. Soc Sci Med [Internet]. 2015;142:202–13. Available from: 10.1016/j.socscimed.2015.08.010 [DOI] [PubMed] [Google Scholar]
- 32.Dallman MF. Stress-induced obesity and the emotional nervous system. Vol. 21, Trends in Endocrinology and Metabolism. 2010. p. 159–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kidwell KM, Nelson TD, Nelson JM, Espy KA. A Longitudinal Study of Maternal and Child Internalizing Symptoms Predicting Early Adolescent Emotional Eating. J Pediatr Psychol [Internet]. 2016;jsw085. Available from: https://academic.oup.com/jpepsy/article-lookup/doi/10.1093/jpepsy/jsw085 [DOI] [PubMed] [Google Scholar]
- 34.Paans NPG, Bot M, Brouwer IA, et al. The association between depression and eating styles in four European countries: The MooDFOOD prevention study. J Psychosom Res. 2018;108:85–92. [DOI] [PubMed] [Google Scholar]
- 35.Sadeh A, Tikotzky L, Kahn M. Sleep in infancy and childhood: Implications for emotional and behavioral difficulties in adolescence and beyond. Vol. 27, Current Opinion in Psychiatry. 2014. p. 453–9. [DOI] [PubMed] [Google Scholar]
- 36.Chaput J-P, Tremblay MS, Katzmarzyk PT, et al. Sleep patterns and sugar-sweetened beverage consumption among children from around the world. Public Health Nutr [Internet]. 2018;(5):1–9. Available from: https://www.cambridge.org/core/article/sleep-patterns-and-sugarsweetened-beverage-consumption-among-children-from-around-the-world/7FC7BE97BB8409FDD955439670B2C4C7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fu ML, Cheng L, Tu SH, Pan WH. Association between Unhealthful Eating Patterns and Unfavorable Overall School Performance in Children. J Am Diet Assoc. 2007;107(11):1935–43. [DOI] [PubMed] [Google Scholar]
- 38.Fröjd SA, Nissinen ES, Pelkonen MUI, Marttunen MJ, Koivisto AM, Kaltiala-Heino R. Depression and school performance in middle adolescent boys and girls. J Adolesc. 2008;31(4):485–98. [DOI] [PubMed] [Google Scholar]
- 39.Chen X, Rubin KH, Li BS. Depressed mood in Chinese children: relations with school performance and family environment. J Consult Clin Psychol [Internet]. 1995;63(6):938–47. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8543716 [DOI] [PubMed] [Google Scholar]
- 40.Wood JJ, Wood J. Effect of anxiety reduction on children’s school performance and social adjustment. Dev Psychol [Internet]. 2006;42(2):345–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16569172 [DOI] [PubMed] [Google Scholar]
- 41.Mazzone L, Ducci F, Scoto MC, Passaniti E, D’Arrigo VG, Vitiello B. The role of anxiety symptoms in school performance in a community sample of children and adolescents. BMC Public Health. 2007;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kolko DJ, Kazdin AE. Emotional/Behavioral Problems in Clinic and Nonclinic Children: Correspondence Among Child, Parent and Teacher Reports. J Child Psychol Psychiatry. 1993;34(6):991–1006. [DOI] [PubMed] [Google Scholar]
- 43.Ahn JS, Min S, Kim MH. The role of uncontrolled eating and screen time in the link of attention deficit hyperactivity disorder with weight in late childhood. Psychiatry Investig. 2017;14(6):808–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leventakou V, Micali N, Georgiou V, et al. Is there an association between eating behaviour andattention-deficit/hyperactivity disorder symptoms in preschool children? J CHILD Psychol PSYCHIATRY. 2016;57(6):676–84. [DOI] [PubMed] [Google Scholar]
- 45.Dahl RE, Gunnar MR. Heightened stress responsiveness and emotional reactivity during pubertal maturation: Implications for psychopathology. Development and Psychopathology. 2009;21(1):1–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.