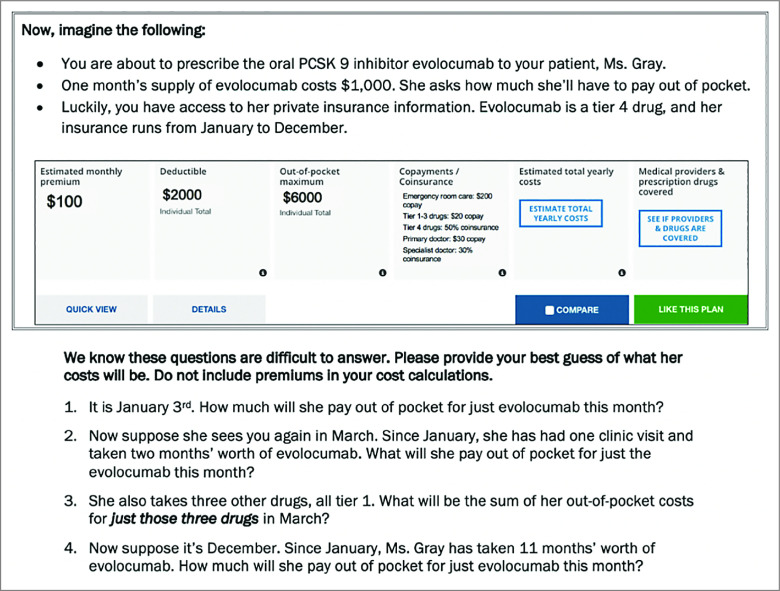
Figure 1. Vignette Assessing Physicians’ Ability to Estimate Out-of-Pocket Costs.
This figure shows the vignette that primary care physicians received. In the vignette that gastroenterologists received, the medication was adalimumab. In the vignette that rheumatologists received, the medication was tofacitinib. Four questions asked physicians to estimate how much the patient would have to pay out of pocket at 4 time points between January and December. Physicians were told that the patient consistently picked up her medications every month. The aim of the 4 questions tied to the vignette was to capture physicians’ ability to estimate out-of-pocket costs using 4 types of insurance cost-sharing: (1) deductibles, (2) coinsurance, (3) copays, and (4) out-of-pocket maximums. The insurance information is presented in the same format used by insurance plans available on the HealthCare.gov website. The insurance plan ran from January to December and the new drug was listed as tier 4 on the plan’s formulary. The first question asked how much she would pay for the tier 4 drug in January. In January, she would not have met her deductible of $2000, so she would have to pay the full price of the drug: $1000. The second question asked how much she would pay for the drug in March. By this time, she would have met her deductible by paying $1000 in January and $1000 in February, so she would owe the coinsurance for tier 4 drugs (50%): $500. The third question asked how much she would pay for 3 other tier 1 drugs available through an outpatient pharmacy benefit in March. Her insurance plan indicated a $20 copay per tier 1 drug, so she would owe a total of $60 for these 3 drugs. Finally, the fourth question asked how much she would pay for the new drug in December. By then, she would have met her out-of-pocket maximum of $6000, so she would owe nothing for the drug ($0).