Abstract
This review aims to investigate the potential of telenursing as a nursing care delivery model for lung cancer throughout the COVID-19 pandemic using a scoping review. The Preferred Reporting Item for Systematic Reviews and Meta-analysis for Scoping Review (PRISMA-ScR) were used in this study. The topic was thoroughly researched in PubMed, CINAHL, and Science Direct. Based on the initial search, there were eight relevant studies out of 432. Websites, phone calls, and lifestream were among the telenursing models discovered in the care of lung cancer patients. The delivery care provided includes monitoring vital signs, symptoms, chemotherapy toxicity, support care, education, and postoperative rehabilitation. Telenursing is considered appropriate for lung cancer patients because it has been shown to help with symptom management, functional status, quality of life, and diminishing the demand for care support. Therefore, telenursing can be used to deliver care for lung cancer throughout the COVID-19 pandemic.
Keywords: COVID-19, lung cancer, nursing delivery care, telenursing
Introduction
Since the outbreak of COVID-19 pandemic in 2019, this severe acute respiratory syndrome caused by coronavirus 2 (SARS-CoV-2) has developed into a worldwide disaster with devastating consequences for human life. Various activities and academic events, including cancer care, research, and academic conferences, have been severely disrupted in an attempt to avert the expansion of the COVID-19.1 Although the pandemic has affected globally, specific subgroups of patients have been disproportionately affected. Patients with certain medical conditions, such as cancer, are identified by the Centers for Disease Control and Prevention (CDC) as having an exceptionally high possibility of developing critical COVID-19 illness.2
Throughout the COVID-19 pandemic, cancer patients may suffer a devastating impact. Furthermore, due to prioritization and resource constraints, care delivery for chronic conditions, including cancer, have been at least partially disrupted during the pandemic’s peaks. Health-care providers and patients have also had to constantly reassess the risks and benefits of cancer-directed interventions with reference to the increased risk of COVID-19 infection.3 Therefore, appropriate home-health technology can be critical in assisting rural-households patients and caretakers in developing the self-management expertise required to live with their illness.
The current telehealth trend shows that telenursing can significantly alleviate these difficulties by redesigning health-care practices and improving quality care delivery, including during the COVID-19 pandemic. Telenursing brings about impactful change that benefits both providers and clients by alleviating the time and costs for healthcare and improving access to care.4 More than 90% of Island Health nurses suggest telehealth as a client care procedure, and 100% encourage telehealth to enhance care to susceptible societies.4 Telehealth, including telenursing specifically for patients with chronic diseases, is becoming progressively crucial during the pandemic. The unconventional use of digital technologies is able to prevail to deliver valuable patient–clinician interaction, for clinical care as well as for patient care obedience along with performance alteration.5 While numerous studies have shown that telehealth and telenursing play a role in chronic disease management,6–8 no study has scope reviewed the telenursing model and its effectiveness for managing lung cancer.
Therefore, in response to safe care needs for lung cancer patients in the new problems of COVID-19, it is important to assess the model, delivery service, feasibility, and efficiency of telenursing to lung cancer. The consequences of this study can have favorable implications for nursing and other professionals, applications developers, social communities, and scientific institutions. A scoping review of various telenursing models can assist developers in understanding the shortcomings of existing telecommunication programs and help include different features and creative technology in the development of future models. Nurses and other health professionals can also analyze varying telenursing models and propose the most efficient telenursing model for patients, enabling them to better control their health. In referring to an adequate model, nursing care activities such as nursing diagnostic and monitoring for lung cancer patients can be carried out online, saving time and money and preventing the transmission of COVID-19 through less traveling.
In this sense, this review purposes to explore the potential of telenursing thoroughly. This assessment is expected to present an outline of the model as well as potential of telenursing as a nursing care delivery model for lung cancer throughout the COVID-19 pandemic.
Materials and Methods
Study Design
This study was designed using Arksey and O’Malley’s scoping review framework, that enables for the inclusion of an extensive study designs to present a comprehensive outline of the research field.9 It was reported succeeding the Preferred Reporting Item for Systematic Review and Meta-analysis for Scoping Review (PRISMA-ScR). The scoping review methodology is suited for this subject because it allows for a thorough study of telenursing care domains to lung cancer. The scoping review began with a broad research topic that was narrowed during the study process to allow for more comprehensive evaluations of the efficacy outcomes. The first study question that informed the initial search process was: which models and type of delivery care services aim to promote informal or formal care in terms of acceptance, efficacy, and efficiency?
Search Strategy
For the publication search, three databases were used: PubMed, CINAHL, and Science Direct. Medical Subject Heading (MeSH)-adjusted literature search was performed using keywords and Boolean operators: ((teleNursing) AND (lung cancer)).
Eligibility Criteria
The criteria in this study based on the PICO framework criteria are:
Patient: Lung cancer and nurse
Intervention: Telenursing
Comparison: No comparison
Outcome: Nursing care delivery model or effect
Other than above, the eligibility conditions were predetermined. We only considered a number of publications that had been accepted for publication or had already been published in peer-reviewed journals. Preprints were not taken into account. All forms of publications were evaluated, including opinions, points of view, original research pieces, and reviews, with no geographic, time, or language constraints.
Data Collection and Analysis
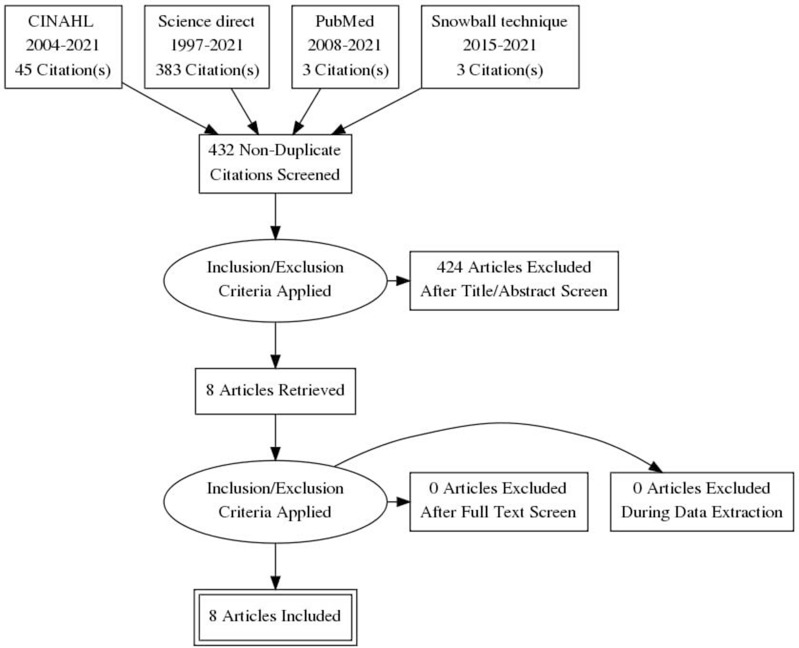
All authors completed the study selection process and the included studies followed the PRISMA flow chart: (1) identifying duplicates; (2) screening of titles and abstracts; and (3) full-text availability. The tabulation method was used to extract data from the study results manually. Among the data items searched were author, country, study design, nursing delivery care, model, and effectiveness.
Results
Description of Selection Study
The initial search identified 432 studies from the database. After excluding 424 studies as irrelevant, the authors included eight studies in this scoping review.10–17 Figure 1 depicts the flow of the study selection process.
Figure 1.
PRISMA flow diagram.
Study Characteristics
The authors identified studies with the following designs: feasibility study, randomized controlled trial, pilot randomized trial with and without controlled trial, quasi-experimental, and user-centered design. Appalachian (n = 2), United Kingdom (n = 2), Iran (n = 2), United States (n = 4), and Netherlands (n = 1) studies were included. The study included 381 participants including lung cancer patients and nurses (see Table 1).
Table 1.
Characteristic of Study
| Ref | Sample | Location | Study Design | Aims |
|---|---|---|---|---|
| [17] | 10 patients hospitalized with lung cancer | Appalachian | Feasibility study | To investigate the feasibility |
| [16] | 112 lung, breast, colorectal cancer patients | United Kingdom | Randomized controlled trial | To evaluate the impact on chemotherapy-related toxicity |
| [15] | 35 nurses | United Kingdom | Mixed method | To evaluate nurse perception and experience |
| [11] | 47 patients discharged with lung cancer | Appalachian | The pilot randomized controlled trial | To investigated the effectiveness |
| [13] | 60 patients with lung and colon cancer | Iran | Quasi-experimental | To determine the impact of Telenursing on improving quality of life |
| [12] | 60 patients with cancer, including 5 lung cancer patients | Iran | Randomized controlled trial | To assess the impact on supportive care needs |
| [14] | 106 lung cancer patients and caregiver | Indianapolis, United State | Randomized pilot trial | Preliminary efficacy evaluation |
| [10] | 5 lung cancer and 5 health professionals, including 1 nurse | Netherlands | A user-centred design | Report on the process of co-creation and evaluation of a program |
Result Finding
Thema 1: Telenursing Model
There are several models for telenursing in the care of lung cancer patients. Phone calls, websites, and lifestream software are examples of models that have been used. Table 2 shows the telenursing model developed in lung cancer services.
Table 2.
Summary of Findings
| Ref | Type of Nursing Delivery | Model | Input | Process | Output | Results |
|---|---|---|---|---|---|---|
| [17] | HomMed Telemonitoring (vital sign and symptom monitoring) | LifeStream software | Patients are asked to check vital signs and fill in psychological assessment data as well as closed questions (yes/no). | The telemonitor passes on to the Honeywell LifeStream software which will be received and accessed in the nurse’s office. The nurse reviews the vital signs after 3 hours after the data is successfully transmitted, then calls the patient to discuss the data sent | Nurse-coaching, self-management, dan call to their clinician | One of every five patients receiving usual care and three of every five patients being monitored completed the entire study. Telemonitored data transmission was feasible and well-received in rural areas; symptom and physiologic data were inconsistent but typical lung cancer. |
| [16] | A mobile phone-based advanced symptom management system (ASyMS©) (monitor and manage chemotherapy-related toxicity) | A mobile phone-based advanced symptom management system | Patients were asked to complete an electronic symptom questionnaire on their mobile phone and take their temperature with an electronic thermometer and enter it into the mobile phone. | This symptom data was immediately transmitted in ‘real time’ to the study server via a secure General Packet Radio Services connection. A dedicated 24-hour pager system was employed to notify health professional based at the clinical site of any incoming symptom reports of concern, with two degrees of alert. An ‘amber alert’ was used to notify clinicians of patients who were suffering toxicities at home that were not severe or life-threatening, but where early care could be useful in preventing further progression of the symptoms reported. A ‘red alert’ was utilized to notify physicians of patients who were pyrexial and/or having severe or life-threatening toxicities at home, and they were instructed to contact patients as quickly as possible. |
Based on the severity of the patient’s symptoms, self-care advice is provided, and nurses conduct appropriate interventions. | Patients were hugely positive about using the ASyMS handset to record their symptoms, with 91% believing that it had aided in managing their symptoms. |
| [15] | A mobile phone-based advanced symptom management system (ASyMS©) (monitor and manage chemotherapy-related toxicity) | A mobile phone-based advanced symptom management system | Patients were asked to complete an electronic symptom questionnaire on their mobile phone and take their temperature with an electronic thermometer and enter it into the mobile phone. | This symptom data was immediately transmitted in ‘real time’ to the study server via a secure General Packet Radio Services connection. A dedicated 24-hour pager system was employed to notify health professional based at the clinical site of any incoming symptom reports of concern, with two degrees of alert. An ‘amber alert’ was used to notify clinicians of patients who were suffering toxicities at home that were not severe or life-threatening, but where early care could be useful in preventing further progression of the symptoms reported. A’red alert’ was utilized to notify physicians of patients who were pyrexial and/or having severe or life-threatening toxicities at home, and they were instructed |
Based on the severity of the patient’s symptoms, self-care advice is provided, and nurses conduct appropriate interventions. | Overall, nurses viewed the use of ASyMS in the management of chemotherapy-related toxicity in lung cancer patients favourably. |
| [11] | Honeywell HomeMed GenesisTM DM (symptoms monitoring) | LifeStream software | Each morning, patients were scheduled to send telemonitored physiologic parameters and symptoms data to the office. Furthermore, individuals were allowed to utilize the device whenever they felt the need for immediate measurement. | Nurses check the information received daily through the LifeStreamTM and called patients to interpret the results as needed, utilizing a questioning/coaching strategy. | Nurses described changes in physiological signs and symptoms and advised patients on how to problem solve and when to call their oncologist specialists, based on motivational interview training. | The telemonitored group improved more in terms of both functional status (Wald X2 = 3.78, p = 0.05) and quality of life (QOL) (Wald X2 = 7.25, p = 0.007). |
| [13] | Not explained the type of delivery | N/I about model | N/I about input | N/I about process | Counselling, 2 call a week | Telenursing improved the quality of life in all aspects (p< 0.001). |
| [12] | Telenursing on the need for supportive care (SCN) (providing supportive care and education) | Telephone calls | Nurses two telephone calls per week of 15 to 30 min | Telephone calls to patients | Information about cancer and treatment options, as well as side effects of chemotherapy and how to manage them (including nausea, vomiting, diarrhoea, constipation, mucositis, and fatigue), as well as self-care in cancer in the areas of nutrition, physical activity, and sleeping. | The results showed that the intervention group’s mean score of dimensions and total SCNs, or supportive care needs, were significantly lower than the control group after the intervention (p0.05). |
| [14] | Telephone-based symptom management (TSM) (management symptoms and emotions) | Telephone calls | Patients were taught symptom management techniques. Symptom management strategies such as relaxation exercises, problem-solving, cognitive restructuring, emotion-focused/self-soothing approaches, communication skills, pleasant activity scheduling, and activity pacing were taught to the patient and caregiver during the four sessions | TSM was conducted through a speakerphone, and all sessions were audio-recorded. Each participant received the same handouts outlining the major points discussed during the sessions and home practice assignments and a CD with relaxation exercise instructions | An instruction in symptom management strategies | At two and six weeks post-intervention, no significant differences were found for all patient outcomes and caregiver self-efficacy for assisting the patient in managing symptoms and caregiving burden. TSM had a negligible effect on caregiver self-efficacy for managing their own emotions and perceived social constraints from the patient. |
| [10] | Information and Communication (ICT) (rehabilitation/ post-surgery care) | The application developed consists of 1) self-monitoring of symptoms and physical activity using on-body sensors and a smartphone, and 2) a web-based physical exercise program. | N/A | N/A | N/A | Seventy-one percent of patients and 78% of health-care professionals said they would use the app as part of their lung cancer treatment. Patients considered the health-care professionals’ positive attitude toward the application to be critical. Overall, usability was rated acceptable (SUS median score = 70, range 35–95). |
In general, all existing models have two components, namely remote patient monitoring via telecommunication technology and treatment centers in health-care facilities. First, the lifestream model utilizes a monitor that is connected to a telephone line whereby, when the patient takes measurements, such as vital signs, these will then be transmitted to the treatment center, then the nurse will monitor, validate and discuss the data that have been received.11,15–17 Second, in telephone call models, the patient is not asked to do an independent assessment, but will be called by the nurse to do an assessment related to symptoms and provide education.12–14 Finally, other researchers’ models propose the development of a sensor-integrated website and mobile application model.10 The Inputs reported by patients in telenursing include symptom data and physiological data.11,15–17 The output of telenursing activities is the provision of counseling, education, self-care management related to symptoms, and referrals.11–17
Thema 2: Delivery Service of Telenursing
The delivery care provided in telenursing services for lung cancer patients includes monitoring vital signs, symptoms, and toxicity after chemotherapy and support care, education, and post-surgery rehabilitation (see Table 2). Each type of delivery care is delivered remotely via telenursing, which can be accessed via sensors, websites, phone calls, or lifestream software.
First, the patient’s vital signs and symptoms are monitored from the data received from the patient. The vital signs monitored include blood pressure, pulse, weight scales, temperature, and oxygen saturation sensors. In addition, patients are monitored for subjective symptoms using physiological parameters, which include question items related to ability or activity barriers (including standing and walking), eating, dyspnea, fatigue, shortness of breath, nausea and vomiting, and anxiety.17 In patients after receiving chemotherapy, monitoring includes specific symptoms related to toxicity and temperature monitoring.15,16 Through the symptoms and physiological indicators collected, nurses can identify the patient’s risk level to adjust self-care planning, self-management and referral to a doctor.
Second, patients will receive treatment in the form of education, counseling, self-care, and self-management.11–13,15–17 Education and counseling are provided in the form of information related to cancer and treatment options or self-care management, as well as side effects of chemotherapy and how to manage them (as well as nausea, vomiting, fatigue, constipation, diarrhea, and mucositis).11,12,15–17 In addition, education is provided in the form of self-care for cancer patients in the areas of dietetics, physical exercise, and sleeping.12
Third, patients will be referred according to the severity of the reported symptoms, including severe or life-threatening toxicities at home and self-management initiation will be carried out when the reported symptoms do not indicate the need for hospitalization.11,15,16 In addition, home monitoring will be facilitated for consultation with doctors or specialists to obtain treatment recommendations according to symptoms.11,17
Theme 3: The Feasibility and Effectiveness of Telenursing
The feasibility study on telenursing in lung cancer patients and nurses shows that it is feasible, even in rural areas. According to a study,17 telenursing data transmission can be done and received effectively in rural areas. Patients and nurses can accept the use of telenursing.10 Furthermore, while telenursing is thought to have a common effect on increasing nurses’ efficacy in managing emotions and social conditions,14 it is also believed to be effective in assisting and managing post-chemotherapy symptoms,16 helping in the management of chemotherapy-related toxicity,15 improving health functional status and quality of life,11,13 and reducing the need for support care.12
Discussion
This scoping review is, to the author’s best knowledge, the first to review the potential of telenursing as a nursing delivery care model for lung cancer throughout the COVID-19 pandemic. The main discoveries revealed that: (i) Websites, phone calls, and lifestream were among the telenursing models discovered in the care of lung cancer patients; (ii) The delivery care provided includes monitoring vital signs, symptoms, and chemotherapy toxicity, support care, education, and postoperative rehabilitation; (iii) Telenursing has been shown to help with symptom management, functional status, quality of life, and reducing the need for care support.
The present obstacle in managing lung cancer patients is balancing the danger of a possibly fatal infection with COVID-19 in opposition to the grave consequences of detaining or failing to treat a potentially fatal malignancy. Cancer patients are especially vulnerable to COVID-19 because of their frequent contact with the healthcare system, their immunocompromised, supportive medications such as steroids and, most essentially, the elderly and their comorbidities.18 The COVID-19 and Cancer Consortium (CCC-19) complete preliminary results were derived from 928 cancer patients, together with 10% lung cancer patients. They revealed a comprehensive rate of death with 13%, a hospitalization rate of 50%, along with 14% of admission to the ICU, and a mechanical ventilation rate of 12%.19 The revised analysis, derived from 2749 evaluable patients, revealed an excessive death rate of 26% for patients with lung cancer, notably higher than for patients with lymphoma (22%), colorectal cancer (19%), breast cancer (8%), prostate cancer (18%), or with an overall mortality rate of 16%.20 The capability to convey treatment safely has to be considered in making decision.
Telehealth, including telenursing, affects not only clients but also providers by improving access to care as well as relieving the time related to moving for healthcare.4 According to the review findings, various telenursing models, such as websites, phone calls, and lifestreams, are currently being developed. Patients use the telehealth model to remotely transmit data about their symptoms and vital signs.10,11,14–17 Furthermore, nurses can remotely monitor the patient’s vitals and symptoms, provide education, support care, and follow-up based on the patient’s emergency through this model.10–17
Aside from its feasibility, telenursing is thought to positively impact the management of vital signs and symptoms associated with disease and treatment.10,11,14–17 According Mosher et al,14 several possible explanations for the findings should be considered. However, indicative lung cancer patients along with caregivers may necessitate more rigorous interference to reduce symptoms. In addition, telenursing is also considered to improve the physical status and quality of life.11,13 The current review’s findings confirmed the positive efficacy of telenursing in a phone rehabilitation arrangement as a helpful approach throughout complementary therapies for cancer patients and that training is highly beneficial.21,22
A meta-analysis of a similar review looked into the efficacy of telemedicine in enhancing the quality of life of patients with lung cancer. The study’s findings revealed that patients in the telemedicine group had a significantly higher quality of life and less anxiety and depression than patients receiving regular care.23 Telemedicine is one type of telehealth managed by doctors. This meta-analysis demonstrated the consistency of results from telehealth use, including telenursing, in improving quality of life and other positive effects.
Previous related review study regarding the use of telehealth shows positive potential in the management of various chronic health problems. For cardiac surgery patients, telehealth could be valuable for assessment and triage prior to surgery, and could relieve ambulatory visits and rehospitalizations in vascular surgery patients. Remote monitoring could also be effective in treating post-surgery post-excess blood vessel damage, reducing the need for further hospital admission.6 For diabetic patients, telehealth may be useful in increasing the number of people screened and in monitoring the development of retinal disease, not only in pandemics/emergencies but also in routine clinical practice.7 For asthma patients, telehealth, including isolated presence solutions along with spirometry monitoring, has the capability to transform future medical management delivery to children and young people with asthma.8 However, although telehealth, including telenursing, shows potential based on historical evidence in the normal setting, several challenges need to be addressed by nurses and other health professionals.
One such involves proceeding from a nurse’s standpoint of making recommendations to patients to the study convention of assisting patients and their families in discovering something they know, any resources they have, and the way they could acquire those resources.17 The figures on physiologic and symptom transitions are valuable measures of patient precariousness, and nurses could coach patients to self-management using motivational interviewing methods derived from their knowledge in nursing.17
Moreover, legal and ethical issues should not be underestimated. The current study suggests that telehealth’s regulatory environment, including telenursing activity, is unpredictable in many circumstances, which adds to the healthcare activity of telenursing itself.24 Telenursing should also adhere to the ethical and legal standards associated with the nursing profession, yet important gaps remain between technological capabilities and legislation/regulations.25 The current COVID-19 emergency is a call to action. Governments’ political efforts should contain explicit provisions on several fronts for evaluating their telenursing policies and their linked repercussions.25 In avoiding ethical problems, it is emphasized that informed consent is documented and medical information always needs to be subject to data protection and confidentiality. Another critical aspect is the training and professionalism of those who conduct the telenursing activity, such as preparation remains the responsibility of universities, training institutions, and individual scientific societies to provide integrated health training with telenursing as soon as possible.24
Our scoping review had some limitations. With recent clinical studies still ongoing, the number of enrolled articles and participants was small. Furthermore, the lack of data during the COVID-19 pandemic severely limits the potential of tracing the disease’s true management, which is only achievable based on historical evidence in normal settings. However, to the best of our knowledge, this was the first scoping review to look into the potential of telenursing care in lung cancer patients.
Conclusion
Overall, telenursing can potentially be an effective nursing care delivery model and intervention in the administration of the well-being of patients with lung cancer throughout the COVID-19 pandemic. Telenursing is especially important currently, as social distancing measures are expected to remain in place for the foreordained future; the top goal is to investigate the utilization of telenursing to decrease patient-to-nurse and other health professional interaction as much as possible.
As social communities and the healthcare system pursue a “new normal,” increased expenditures in closing technical gaps worldwide will be required to become more common. Therefore, developers are expected to design more common and integrated telenursing technology that allows access to all functions or service delivery. Given the benefits and effectiveness of telenursing, lung cancer patients and health systems are expected to start using telenursing to improve monitoring services. Nurses and other health workers are expected to make protocols that help patients and families meet their health needs according to applicable laws and ethics. In addition, the government is also expected to start reviewing and drafting legislation that supports telenursing and protects patients, nurses, and other health workers in the use of telenursing.
More resources should be invested in the establishment of telenursing care along with more high-quality RCTs should be regulated to investigate the practicality of telenursing in managing patients with lung cancer, particularly during the COVID-19 pandemic.
Acknowledgments
The authors appreciated the Universitas Padjadjaran, Bandung, West Java, Indonesia, and National Library of Indonesia for facilitating the database search to this review.
Funding Statement
There was no external funding.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet (London, England). 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Certain medical conditions and risk for severe COVID-19 illness; 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed July 1, 2021.
- 3.Schrag D, Hershman DL, Basch E. Oncology practice during the COVID-19 pandemic. JAMA. 2020;323(20):2005–2006. doi: 10.1001/jama.2020.6236 [DOI] [PubMed] [Google Scholar]
- 4.Allen M, Aylott M, Loyola M, Moric M, Saffarek L. Nurses: extending care through telehealth. Stud Health Technol Inform. 2015;208:35–39. doi: 10.17265/1548-7709/2015.03.003 [DOI] [PubMed] [Google Scholar]
- 5.Liu N, Huang R, Baldacchino T, et al. Telehealth for noncritical patients with chronic diseases during the COVID-19 pandemic. J Med Internet Res. 2020;22(8):e19493. doi: 10.2196/19493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ajibade A, Younas H, Pullan M, Harky A. Telemedicine in cardiovascular surgery during COVID-19 pandemic: a systematic review and our experience. J Card Surg. 2020;35(10):2773–2784. doi: 10.1111/jocs.14933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galiero R, Pafundi PC, Nevola R, et al. The importance of telemedicine during COVID-19 pandemic: a focus on diabetic retinopathy. Tatti P, ed. J Diabetes Res. 2020;2020:9036847. doi: 10.1155/2020/9036847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davies B, Kenia P, Nagakumar P, Gupta A. Paediatric and adolescent asthma: a narrative review of telemedicine and emerging technologies for the post-COVID-19 era. Clin Exp Allergy. 2021;51(3):393–401. doi: 10.1111/cea.13836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 10.Timmerman JG, Tönis TM, Weering MG, et al. Co-creation of an ICT-supported cancer rehabilitation application for resected lung cancer survivors: design and evaluation. BMC Health Serv Res. 2016;1–11. doi: 10.1186/s12913-016-1385-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen Y, Narsavage G, Frick K, Petitte T. Home-telemonitoring lung cancer intervention in Appalachia: a pilot study. Physiol Behav. 2017;176(3):139–148. [PMC free article] [PubMed] [Google Scholar]
- 12.Ebrahimabadi M, Rafiei F, Nejat N. Can tele-nursing affect the supportive care needs of patients with cancer undergoing chemotherapy? A randomized controlled trial follow-up study. Support Care Cancer. 2021;29:5865–5872. doi: 10.1007/s00520-021-06056-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chakeri A, Salehi S, Gharebagh ZA, Haghani S. Evaluating the effect of tele - nursing on the quality of life of cancer patients admitted to selected hospitals of Tehran University of Medical Sciences in 2014–2015. Int J Ayurved Med. 2015;9:83–87. [Google Scholar]
- 14.Mosher CE, Winger JG, Hanna N, et al. Randomized pilot trial of a telephone symptom management intervention for symptomatic lung cancer patients and their family caregivers. J Pain Symptom Manage. 2016;52(4):469–482. doi: 10.1016/j.jpainsymman.2016.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maguire R, McCann L, Miller M, Kearney N. Nurse’s perceptions and experiences of using of a mobile-phone-based Advanced Symptom Management System (ASyMS) to monitor and manage chemotherapy-related toxicity. Eur J Oncol Nurs. 2008;12(4):380–386. doi: 10.1016/j.ejon.2008.04.007 [DOI] [PubMed] [Google Scholar]
- 16.McCann L, Maguire R, Miller M, Kearney N. Patients’ perceptions and experiences of using a mobile phone-based advanced symptom management system (ASyMS) to monitor and manage chemotherapy related toxicity. Eur J Cancer Care (Engl). 2009;18(2):156–164. doi: 10.1111/j.1365-2354.2008.00938.x [DOI] [PubMed] [Google Scholar]
- 17.Petitte TM, Narsavage GL, Chen Y-J, Coole C, Forth T, Frick KD. Feasibility study: home telemonitoring for patients with lung cancer in a mountainous rural area. Oncol Nurs Forum. 2014;41(2):153–161. doi: 10.1188/14.ONF.153-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Passaro A, Bestvina C, Velez Velez M, Garassino MC, Garon E, Peters S. Severity of COVID-19 in patients with lung cancer: evidence and challenges. J Immunother Cancer. 2021;9(3):1–10. doi: 10.1136/jitc-2020-002266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuderer NM, Choueiri TK, Shah DP, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet (London, England). 2020;395(10241):1907–1918. doi: 10.1016/S0140-6736(20)31187-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rini BI. Abstract IA26: understanding the impact of COVID in cancer patients through the COVID-19 and Cancer (CCC-19) and other COVID consortiums. Clin Cancer Res. 2020;26(18Supplement):IA26–IA26. doi: 10.1158/1557-3265.COVID-19-IA26 [DOI] [Google Scholar]
- 21.Galiano-Castillo N, Ariza-García A, Cantarero-Villanueva I, et al. Telehealth system (e-CUIDATE) to improve quality of life in breast cancer survivors: rationale and study protocol for a randomized clinical trial. Trials. 2013;14(1):187. doi: 10.1186/1745-6215-14-187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shojaee A, Nehrir B, Naderi N, Zareyan A. Comparison of patient education and follow up by nurse on anxiety in heart failure patients. Med Surg Nurs J. 2014;3(1):52–60. [Google Scholar]
- 23.Pang L, Liu Z, Lin S, et al. The effects of telemedicine on the quality of life of patients with lung cancer: a systematic review and meta-analysis. Ther Adv Chronic Dis. 2020;11:2040622320961597. doi: 10.1177/2040622320961597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nittari G, Khuman R, Baldoni S, et al. Telemedicine practice: review of the current ethical and legal challenges. Telemed J e-Health. 2020;26(12):1427–1437. doi: 10.1089/tmj.2019.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Battineni G, Nittari G, Sirignano A, Amenta F. Are telemedicine systems effective healthcare solutions during the COVID-19 pandemic? J Taibah Univ Med Sci. 2021;16(3):305–306. doi: 10.1016/j.jtumed.2021.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]