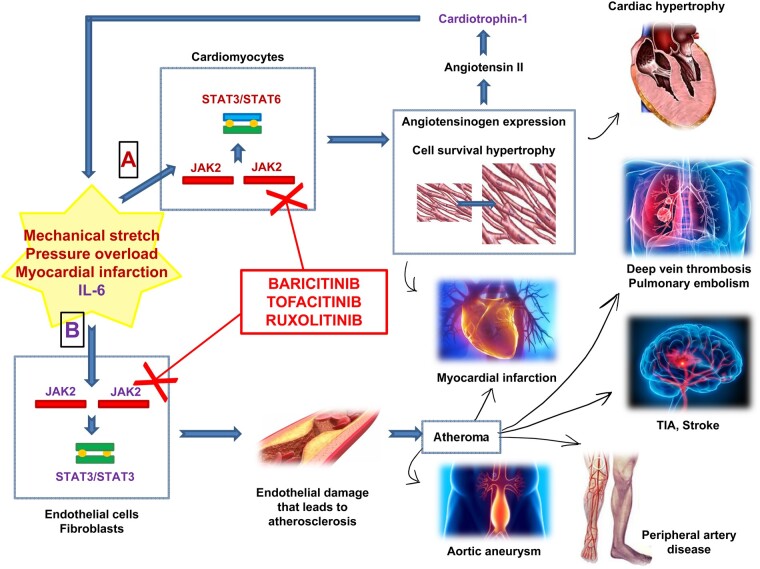
Clinical effects of JAK–STAT pathway activations and JAK–STAT inhibitors. (A) Stimuli, such as mechanical stretch, pressure overload and myocardial infarction, activate the JAK2/JAK2-STAT3/STAT6 pathway. This way allows the expression of the angiotensinogen gene promoter in cardiac myocytes. Angiotensinogen eventually leads to the production of angiotensin II that in turn induces the production of cardiothropin-1, a member of the IL-6 family, ultimately producing cardiac hypertrophy. The clinical effects of this pathway are cardiac hypertrophy or myocardial infarction (both could result in heart failure). Cardiotrophin-1 in turn allows the activation of the B-pathway. (B) Cytokines, such as IL-6, could activate the JAK2/JAK2-STAT3/STAT3 pathway in fibroblasts and endothelial cells. They are responsible for the endothelial damage that leads to atherosclerosis, with the formation of atheroma. There are several events linked to atherosclerotic cardiovascular disease, such as myocardial infarction, deep vein thrombosis and pulmonary embolism, cerebrovascular events (transient ischaemic attack, stroke), peripheral artery disease, and the formation of aortic aneurysms. JAK–STAT inhibitors, through the inhibition of the JAK–STAT pathway, may represent a way to prevent these adverse cardiovascular events. Baricitinib (JAK1/JAK2 inhibitor), tofacitinib (JAK1/JAK2/JAK3 inhibitor) and ruxolitinib (JAK1/JAK2 inhibitor) are treatment approved in RA and in MPNs that are hypothesized to have potential cardiovascular benefit.

An official website of the United States government
Here's how you know
Official websites use .gov
A
.gov website belongs to an official
government organization in the United States.
Secure .gov websites use HTTPS
A lock (
) or https:// means you've safely
connected to the .gov website. Share sensitive
information only on official, secure websites.