Abstract
Although Mexican immigrants to the United States (US) have historically held health and mortality advantages over US-born groups, evolving population dynamics in Mexico paired with shifts in Mexico-US immigration patterns and policy regimes have raised new concerns about the metabolic health of recent cohorts of Mexican immigrants. Using a nationally representative sample of adults aged 20-years and older (n = 10,833) from the National Health and Nutrition Examination Study (NHANES, 1999–2016), we assess and seek to explain differences in metabolic syndrome (MetS) risk by race-ethnicity, country of origin, and duration of residence in the US and evaluate whether recent Mexican immigrants continue to exhibit a metabolic health advantage. We decompose the difference in MetS prevalence between US-born whites (45.5%) and recent Mexican immigrants (29.5%) to determine how demographic, socioeconomic, and health behavior characteristics contribute to the patterning of metabolic health. Findings reveal that recent Mexican immigrants hold a metabolic health advantage over all groups, which is accounted for by their younger age structure. Yet recent Mexican immigrants would retain a sizable age-adjusted MetS advantage if they were to achieve parity with US-born whites on education, income, and food security. To ensure that newly-arrived Mexican immigrants continue to experience historically favorable health and mortality prospects, modest policy changes could offer health-promoting protections in the form of increased economic and food security, as well as improved educational opportunities for younger immigrants.
Keywords: Hispanic paradox, Immigrant health advantage, Metabolic syndrome, Mexico-US immigration, Decomposition
Highlights
-
•
Recent Mexican immigrants hold a metabolic health advantage over earlier immigrants and US-born groups.
-
•
The metabolic health advantage of recent Mexican immigrants is explained by their younger age, but would be retained with improved SES.
-
•
Policy changes could improve immigrants’ metabolic health through increased economic and food security, as well as improved educational opportunities.
1. Introduction
A large body of research examines racial-ethnic and immigrant-native health disparities among the adult population in the United States (US). Studies indicate that minoritized racial-ethnic groups such as Blacks and Hispanics have worse health than the majority group of non-Hispanic whites (Brown, 2018). Research also documents an immigrant health advantage across various racial-ethnic backgrounds and areas of origin with immigrants experiencing better health, particularly within their first decade of relocation, and also outliving their native US-born peers (Antecol & Bedard, 2006; Brown, 2018; Hummer & Gutin, 2018). Hispanics also hold a puzzling yet persistent survival advantage over non-Hispanic whites, termed the Hispanic paradox, which is most pronounced among first-generation Mexican immigrants (Lariscy et al., 2015; Markides & Coreil, 1986; Markides & Eschbach, 2005).
Despite these consistently documented patterns, it is unclear whether recent waves of Mexican immigrants will continue to enjoy a health advantage in at least one key area, metabolic syndrome (MetS). MetS captures several markers of dysregulation—including obesity, elevated blood glucose levels, and hypertension—and is a strong predictor of morbidity and mortality (Alberti et al., 2009; Eckel et al., 2010). There are two key sources of concern about the future metabolic health of recent cohorts of Mexican immigrants to the US. First, Mexico's rapid nutrition and epidemiologic transitions have been followed by one of the steepest increases in obesity observed in any country (Popkin et al., 2012), with adult rates rising by 42.2% between 2000 and 2018 (Barquera et al., 2020). Second, a shift in Mexico-US immigration patterns and policy regimes has left recent waves of immigrants more vulnerable to the health deteriorating effects of heightened discrimination, hostility, and harsh work environments (Orrenius & Zavodny, 2009; Viruell-Fuentes et al., 2012).
Using nationally representative population health data, this study examines the metabolic health of foreign-born Mexicans, stratified by duration of residence in the US, relative to US-born Mexican Americans and non-Hispanic whites. We also further assess how key demographic, socioeconomic, and health behavior characteristics contribute to observed population health disparities. This study advances scholarship on racial-ethnic and immigrant-native health disparities, generally, and also specifically contributes new knowledge on the recent metabolic health of the US Mexican-origin population in two key ways. First, we leverage population level biomarker data to capture all the dimensions of MetS that have been linked to increased morbidity and mortality. Second, we focus on the role of social factors in population health disparities—including demographic, socioeconomic, and health behavior characteristics—to generate evidence that can help inform policy solutions. Generating a fuller understanding of how demographic, socioeconomic, and health behavior characteristics contribute to the recent patterning of metabolic health across groups defined by race-ethnicity, country of origin, and duration of residence can help researchers and policymakers identify preventive strategies to slow the rising risk of obesity and related metabolic conditions in the US and Mexico, and ultimately help preserve the prolonged life expectancy of Mexican immigrants and their descendants living in the US.
2. Background
2.1. Racial-ethnic health disparities
Despite overall improvements in health and longevity over the past century, significant racial-ethnic health disparities rooted in social inequality persist and continue to present the greatest impediment to improving population health in the US (Gutin & Hummer, 2021; House, 2002). In racialized societies like the US (Bonilla-Silva, 1997), racism structures how minoritized groups, currently and historically, face differential access to resources, opportunities, and risks, making racism a fundamental cause of health and health disparities (Phelan & Link, 2015). Historically, the predominant focus of health disparities research in the US has been on Black-white health gaps, but disparities have also been increasingly documented between whites and Hispanics. Research in this area has emphasized Hispanics’ survival advantage (Elo et al., 2004; Lariscy et al., 2015), but less attention has been dedicated to understanding whether the Hispanic paradox in mortality extends to other dimensions of health and wellbeing (Hayward et al., 2014). The existing research is mixed, suggesting that, compared to whites, Hispanics have similar or more favorable rates of cardiovascular disease and cancer (Crimmins et al., 2004), comparable or better psychological wellbeing (Williams, 2018), but higher rates of diabetes and disability (Crimmins et al., 2004; Hayward et al., 2014). These equivocal findings on the relative health standing of Hispanics are largely attributable to the complexity and heterogeneous patterns introduced by intersecting systems of discrimination and inequality by race, ethnicity, and immigrant status (Boen & Hummer, 2019).
2.2. Immigrant health advantage
Immigrants have lower mortality rates than US-born individuals (Dupre et al., 2012), less disability during their working years (Levchenko, 2021; Markides et al., 2007), and fewer chronic health conditions, including cancer, diabetes, heart disease, hypertension, and stroke (Brown, 2018; Gorman et al., 2010). In the US, this “immigrant health advantage” is particularly well-documented amongst the Mexican-origin population (Cho et al., 2004). Three explanations have been proposed to account for this healthy immigrant effect, including migrant selection, data issues, and differences in health behaviors and risk profiles.
First, immigrants are selected on numerous characteristics positively associated with health, and thus are generally healthier than the populations they leave behind and often those they are joining (Riosmena et al., 2013). The initial health advantage of the US immigrant population may also be partially reinforced by a pattern of return migration amongst migrants in poor health, commonly referred to as the “salmon bias” (Abraído-Lanza et al., 1999; Palloni & Arias, 2004). While positive selection on education and health have long characterized Mexican immigration to the US (Akresh, 2008), there are signs that this pattern is beginning to attenuate (Feliciano, 2005) and separate research also shows that return migration plays a limited role in observed health and mortality differences (Hummer et al., 2007; Riosmena et al., 2013; Turra & Elo, 2008).
A second explanation considers possible data issues that may disproportionately influence the health and mortality records of Hispanic immigrants, such as misidentification of ethnicity and age on death certificates and a higher probability of mismatched mortality records in population data sources. There is little empirical evidence that data issues account for a significant portion of Hispanic immigrant-native disparities (Hummer et al., 2007; Palloni & Arias, 2004), although differential linkage of mortality records has been found to reduce the accuracy of mortality risk estimation for Hispanics in nationally-based US data sources (Lariscy, 2011). Finally, a third explanation focuses on differences in the health risk profiles of immigrants compared to the US native-born population, specifically less intensive and lower rates of smoking, lower rates of excessive drinking, and less obesity (Singh & Siahpush, 2002). Smoking behavior, in particular, has been shown to explain the majority of Mexican immigrants’ health and mortality advantage over US-born whites (Blue & Fenelon, 2011; Fenelon, 2013). While all three of these explanations partially account for the health advantages previously observed among US Hispanic immigrants, it is also important to consider recent changes to the conditions immigrants experience in both sending and receiving countries to make sense of contemporary health patterns and to predict future trajectories.
2.3. Demographic, nutrition, and epidemiologic transitions and the rise of metabolic health risks in Mexico and the US
Over the past two decades Mexico has experienced significant demographic, nutrition, and epidemiologic transitions (Rivera et al., 2004). While all three transitions are interrelated, the demographic transition has been marked by lowered risk of premature mortality and population aging, the nutritional transition by a shift from prevalent undernutrition to a predominance of diet-related chronic conditions, and the epidemiologic transition by chronic conditions replacing infectious disease as the primary source of premature morbidity and mortality (Omran, 1971; Popkin, 2001). The drivers of evolving population dynamics in Mexico are multifactorial, but the influence of globalization and trade liberalization, such as the passing of the North American Free Trade Agreement (NAFTA) in 1992, has played an outsized role in weakening the power and viability of domestic food suppliers and yielding a food environment dominated by cheap and abundant processed foods (Thow, 2009). This drastic overhaul of the country's domestic food environment helped lay the groundwork for the rapid increase in obesity and related metabolic conditions that Mexico has experienced over the past two decades (Barquera & Rivera, 2020).
For much of the early 21st century, the US had the highest recorded adult obesity prevalence among OECD countries. Yet following these rapid nutrition and epidemiologic transitions, adult obesity in Mexico rose quickly and slightly surpassed that of the US in 2013 (Barquera & Rivera, 2020). The US has since reclaimed the top ranking, although the proportion of severely obese adults and the mortality risks associated with obesity remain higher in Mexico (Barquera et al., 2020; Monteverde et al., 2010; Ogden et al., 2020). Within the US, a similar dynamic exists with Hispanics, and Mexican Americans in particular, exhibiting a higher obesity prevalence than whites (Flegal et al., 2012, 2016). In both countries today, the main causes of preventable mortality are associated with obesity, including cardiovascular disease, diabetes, chronic respiratory disease, and cancer (World Health Organization (WHO), 2018a, World Health Organization (WHO), 2018b). This convergence in the nutritional and epidemiologic profiles of Mexico and the United States raises important questions about whether recent and future generations of Mexican immigrants will continue to hold a metabolic health advantage over the US-born population (Goldman, 2016), with some evidence suggesting that this advantage has already begun to deteriorate among youth-aged Mexican immigrants in California (Buttenheim et al., 2013).
2.4. Social determinants of immigrant health deterioration
Immigrants' health tends to decline shortly after migration (Goldman et al., 2014), with evidence that initial health advantages erode significantly and can even disappear altogether within the first decade of relocation (Antecol & Bedard, 2006). One prominent explanation points to the detrimental effects of acculturation on immigrant health behaviors through exposure to US society, which has been supported as a leading explanation for the “disability crossover” (Levchenko, 2021), whereby Mexican immigrants with an initial age-specific disability advantage in their working years later have higher rates of disability relative to US-born whites at older ages regardless of educational achievement (Levchenko, 2021). However, more nuanced explanations have also been offered, guided by segmented assimilation theory and related frameworks from the immigrant integration literature (Portes & Zhou, 1993). These explanations recognize both immigrants' acculturation to American preferences and norms and also the existence of segmented pathways to immigrant inclusion based on socioeconomic position and mobility (Goldman et al., 2014; Van Hook et al., 2016). Thus, while the majority of Mexican immigrants facing socioeconomic disadvantage might be expected to acculturate to the less healthy behaviors of lower-income groups in the US (Abraído-Lanza et al., 2006), others will incorporate into more advantaged positions where they may encounter health promoting behaviors and opportunities. Consistent with this framework of multiple acculturative processes, research comparing Mexican migrants to non-migrants remaining in Mexico shows that those who migrate are more likely to experience significant short-term changes in health, whether positive or negative, with an overall trend towards health deterioration for the majority of recent Mexican immigrants (Goldman et al., 2014). However, evidence consistent with various acculturative processes does not rule out the possibility that discrimination and other structural forces may be operating simultaneously to influence patterns of immigrant health deterioration regardless of socioeconomic standing and level of integration into US society (Levchenko, 2021). Thus, others have also focused on social inequality as a root cause of immigrant health declines, acknowledging that Mexican immigrants across the socioeconomic spectrum may face varying levels of discrimination and chronic stress due to how they are perceived and treated within US society (Viruell-Fuentes et al., 2012). Taken together, it is clear that research on racial-ethnic and nativity health disparities must consider not only the effect of exposure to US society on immigrant health and health behaviors, but also the contribution of social factors and structural environments that play a role in shaping immigrants’ experiences and opportunities post-migration.
2.5. Research aims
In light of uncertainty over the current and future metabolic health of the Mexican-origin population in the US, we pursue two aims in the present study:
-
1.
Compare the metabolic profiles of adult-aged US-born whites, US-born Mexican Americans, and recent and earlier Mexican immigrants to evaluate whether recent Mexican immigrants hold a metabolic health advantage.
-
2.
Assess the contribution of demographic, socioeconomic, and health behavior characteristics to observed population health gaps by race-ethnicity, country of origin, and duration of residence in the US.
3. Materials and methods
3.1. Data and sample
Data were acquired from the National Health and Nutrition Examination Survey (NHANES), a cross-sectional, nationally representative, population-based survey conducted by the Centers for Disease Control and Prevention that uses a complex, multistage probability sampling strategy designed to be representative of the civilian, non-institutionalized US population (NCHS, 2013; NCHS, 2018). We combined eight waves of data (1999–2016) for adults aged 20 or older. We excluded respondents who were pregnant (n = 1029), did not complete the physical examination (n = 1480), were not included in the morning laboratory examination that was restricted to the fasting subsample (n = 16,076) or had their age top-coded in NHANES (n = 790), leaving an eligible sample of 11,559 individuals. The sample was further restricted to those with complete information on all study outcomes, creating a final analytic sample of 10,833 individuals (93.7% of eligible sample): foreign-born Mexican (n = 1799), US-born Mexican American (n = 1334), US-born non-Hispanic white (n = 7700).
3.2. Measures
Metabolic syndrome (MetS) was the primary outcome. We constructed the MetS measure using the six individual risk factors included in the most recently harmonized definition of MetS (Alberti et al., 2009). MetS encapsulates several health conditions that epidemiological studies have found to co-occur in patients with a high risk of cardiovascular disease and type-2 diabetes. The six indicators of metabolic dysregulation include: elevated fasting glucose (≥100 mg/dL), elevated triglycerides (≥150 mg/dL), lowered HDL cholesterol (<40 mg/dL for males, <50 mg/dL for females), elevated blood pressure (systolic ≥130 mmHg, diastolic ≥85 mmHg), obesity (BMI ≥30 kg/m2), and an increased waistline (≥102 cm for males, ≥ 88 cm for females) (Alberti et al., 2009; Eckel et al., 2005). Respondents were classified as having MetS if they possessed three or more of the individual health risks based on NHANES laboratory and physical examinations, or self-reported taking medications to control them (Alberti et al., 2009; Eckel et al., 2005). We created dichotomous measures (0/1) for each component as well as a summary indicator of MetS (0/1).
We divided the sample into four groups to examine differences in MetS by race-ethnicity, country of origin, and duration of residence in the US. The two US-born groups, non-Hispanic whites (hereafter, US-born whites) and Mexican Americans, were each defined based on self-reported responses to a single race-ethnicity question. In order to analyze expected changes in health status with increasing time spent in the US, we sub-classified the foreign-born Mexicans (Mexican immigrants) into two additional groups (recent and earlier immigrants) based on their self-reported duration of residence in the US: less than ten years (n = 493), or ten years or more (n = 1250).
Three categories of independent variables were used to explain prevalence differences in MetS: demographic characteristics, socioeconomic factors, and health behaviors. Demographic characteristics included age and gender. Socioeconomic factors included education (less than high school, high school or GED, and some college/college graduate), employment (not employed, part-time under 35 h/week, and full-time over 35 h/week), and income (income-to poverty ratio). Given the cross-sectional nature of the data, we selected three health behaviors that would be difficult for respondents to alter in response to a diagnosis of MetS in effort to minimize reverse causation bias. These included three-category measures of alcohol consumption (never or former drinker, moderate drinker [≤ 1 drink/day for females, ≤ 2 drinks/day for males], and heavy or binge drinker [> 1 drink/day for females, > 2 drinks/day for males]) and food security (full, marginal, and low/very low), as well as a continuous measure of years spent smoking. We also included a survey wave indicator in all analyses to adjust for trends in MetS over the study period.
3.3. Analysis
All analyses were weighted and conducted in Stata/MP-2 17.0 using the svy command prefix (StataCorp, College Station, Texas, USA). Within the analytic sample, 15.3% had missing data on one or more covariates (education, employment, income-to-poverty ratio, years smoking, alcohol, and/or food security), with no more than 6.3% of the sample missing on any single covariate. In order to preserve cases and to avoid introducing bias through listwise deletion (Allison, 2001), we employed multiple imputation separately for each study population. We estimated unadjusted proportions and means for all demographic, socioeconomic, and health behavior characteristics, as well as all metabolic health outcomes. To account for major differences in the age structure of each of our four study populations, we then estimated 18-year age-standardized prevalence rates using direct standardization to the 2000 US Census population age distribution (Klein & Schoenborn, 2001). We also determined the prevalence rate for each study group at every two-year survey wave, and then imposed a GLM smoothing function to graph the group trends in MetS over the full study period.
For the main analysis, we decomposed the MetS prevalence difference between US-born whites and recent Mexican immigrants, in order to assess how key demographic, socioeconomic, and health behavior characteristics contribute to a possible immigrant health advantage. The decomposition divides between-group differences in the dependent variable into a component due to differences in population characteristics (i.e., the “explained” or “endowment” portion) and a component due to differential returns to those characteristics (i.e., the “unexplained” or “coefficient” portion). The unexplained portion represents the between group disparity that would theoretically remain if the two groups were matched on identical levels for all model variables.
This technique—first introduced by sociologist and demographer Kitagawa (Kitagawa, 1955), and further popularized by economists Blinder and Oaxaca (Blinder, 1973; Oaxaca, 1973)—has been increasingly recognized as a preferred approach for analyzing and explaining racial-ethnic disparities in health (Jackson & VanderWeele, 2018; VanderWeele & Robinson, 2014). An age2 term was also included to account for the curvilinear association between age and MetS.
We subsequently estimated associations between independent variables and MetS in each study population using Poisson regression with a log link function and robust standard errors to directly estimate the prevalence rate ratio (PRR) between groups (Barros & Hirakata, 2003). This model also included interactions of gender x race-ethnicity/country of origin/duration of residence group and education x race-ethnicity/country of origin/duration of residence group to account for expected differences in associations by study population. An age2 term was also included in our regression model. We then estimated the predicted prevalence of MetS associated with a specified value of each covariate with age held at the overall sample mean (46.5), and all other covariates fixed at their observed levels for each individual and then averaged within each group. All tests were two-sided and significance was considered at P < 0.05 for all analyses.
4. Results
4.1. Descriptive statistics
Table 1 summarizes the weighted demographic, socioeconomic, and health behavior characteristics, of the four study groups. Recent Mexican immigrants were the youngest group, with a mean age of 32.2 years for those residing in the US less than ten years. Mexican immigrants residing in the US for ten years or more were closer in age to US-born Mexican Americans, with mean ages for these groups of 42.1 and 40.2 years, respectively. US-born whites were the oldest population, with a mean age of 47.2 years. Both groups of foreign-born Mexicans were composed of more males compared to US-born Mexican Americans and US-born whites. Both groups of foreign-born Mexicans had significantly lower educational attainment and income, but had higher levels of full-time employment than US-born groups. In terms of health behaviors, both the US-born and foreign-born Mexicans had smoked fewer years than US-born whites on average. The foreign-born Mexican groups had the highest share of non- and former-drinkers, but also the highest levels of heavy alcohol drinkers, while US-born whites and Mexican Americans had higher shares of moderate drinkers. US-born whites were the most food secure of all the groups, with significantly higher levels of full food security and the lowest levels of food insecurity (i.e., low/very low food security), while both groups of foreign-born Mexicans had lower levels of food security and higher levels of food insecurity relative to the US-born groups.
Table 1.
Weighted demographic, socioeconomic, health behavior characteristics, and outcomes by race-ethnicity, country of origin, and duration of residence: US-residing adults in the National Health and Nutrition Examination Survey (NHANES, 1999–2016) (N = 10,833).
|
US-born |
Foreign-born Mexicans (FBM) |
|||
|---|---|---|---|---|
| Non-Hispanic whites (NHW) (N = 7700) |
Mexican Americans (MA) (N = 1334) |
In US < 10 years (N = 491) | In US 10+ years (N = 1308) | |
| Demographic characteristics | ||||
| Age, [mean (SE)] | 47.2†‡§ (0.277) | 40.2*‡§ (0.462) | 32.2*†§ (0.552) | 42.1*†‡ (0.553) |
| Gender, male [%] | 49.9‡§ | 50.9‡§ | 59.1*† | 54.9*† |
| Socioeconomic characteristics | ||||
| Education [%] | ||||
| Less than high school | 11.7†‡§ | 24.1*‡§ | 66.5*† | 67.5*† |
| High school or GED | 24.5§ | 24.1§ | 20.7 | 16.4*† |
| Some college or college graduate | 63.7†‡§ | 51.8*‡§ | 12.8*† | 16.2*† |
| Income-to-poverty ratio (PIR), [mean (SE)] | 3.3†‡§ (0.044) | 2.5*‡§ (0.085) | 1.3*†§ (0.064) | 1.6*†‡ (0.048) |
| Employment [%] | ||||
| Not employed | 32.3‡ | 31.6‡ | 24.8*† | 29.0 |
| Part time (1–34 h/week) | 14.3 | 14.5 | 13.3 | 12.8 |
| Full time (≥35 h/week) | 53.4‡§ | 53.9‡ | 61.9*† | 58.2* |
| Health behaviors | ||||
| Smoking, years spent [mean (SE)] | 10.7†‡§ (0.257) | 6.8*‡ (0.371) | 4.8*†§ (0.428) | 6.5*‡ (0.383) |
| Alcohol [%] | ||||
| Never or former drinker | 23.7‡§ | 25.3§ | 30.8* | 35.7*† |
| Current moderate drinker | 38.8†‡§ | 26.1*‡§ | 19.2*† | 20.4*† |
| Current heavy or binge drinker | 37.5†‡§ | 48.6* | 50.0* | 43.8* |
| Food security [%] | ||||
| Full food security | 85.4†‡§ | 65.7*‡§ | 45.1*†§ | 53.6*†‡ |
| Marginal food security | 5.4†‡§ | 15.1*‡ | 23.5*†§ | 17.5*‡ |
| Low/very low food security | 9.2†‡§ | 19.2*‡§ | 31.4*†§ | 28.9*† |
| Outcomes, unadjusted 18-year prevalence | ||||
| High-risk metabolic health indicators [%] | ||||
| Pre-diabetes | 43.2§ | 44.8§ | 41.9§ | 55.5*†‡ |
| High triglycerides | 29.5§ | 31.5 | 29.2 | 34.4* |
| Low HDL cholesterol | 40.3‡ | 41.6‡ | 34.4*†§ | 40.7‡ |
| High blood pressure | 38.5†‡§ | 32.0*‡§ | 13.2*†§ | 26.5*†‡ |
| High waist circumference | 54.6†‡ | 60.8*‡§ | 36.9*†§ | 54.8†‡ |
| Obesity | 33.5†‡§ | 45.5†‡§ | 23.2*†§ | 39.8†‡§ |
| Metabolic syndrome, ≥3 high-risk health indicators |
45.5†‡ | 50.9*‡ | 29.5*†§ | 49.6‡ |
| Outcomes, age-standardized 18-year prevalencea | ||||
| High-risk metabolic health indicators [%] | ||||
| Pre-diabetes | 40.5†‡§ | 49.8*§ | 50.7*§ | 56.9*†‡ |
| High triglycerides | 28.6†‡§ | 33.7* | 37.6* | 34.3* |
| Low HDL cholesterol | 39.0†§ | 43.2* | 38.2 | 42.3* |
| High blood pressure | 34.9†‡§ | 38.5*‡§ | 28.8*† | 30.8*† |
| High waist circumference | 52.6† | 63.5*‡§ | 50.7† | 55.5† |
| Obesity | 32.7†‡§ | 46.2*‡§ | 28.1*†§ | 40.1*†‡ |
| Metabolic syndrome, ≥3 high-risk health indicators |
42.9†§ | 55.4*‡§ | 43.0†§ | 50.7*†‡ |
Notes. Weighted descriptive statistics. Symbols indicate a statistically significant difference at the α = 0.05 level in proportions/means between the respective group in each column and US-born non-Hispanic whites (*), US-born Mexican Americans (†), foreign-born Mexicans in the US < 10 years (‡), and foreign-born Mexicans in the US 10 or more years (§).
Prevalence rates for the eighteen-year study period are age-standardized to the US population distribution according to the 2000 US Census and incorporate survey weights to generate nationally representative estimates.
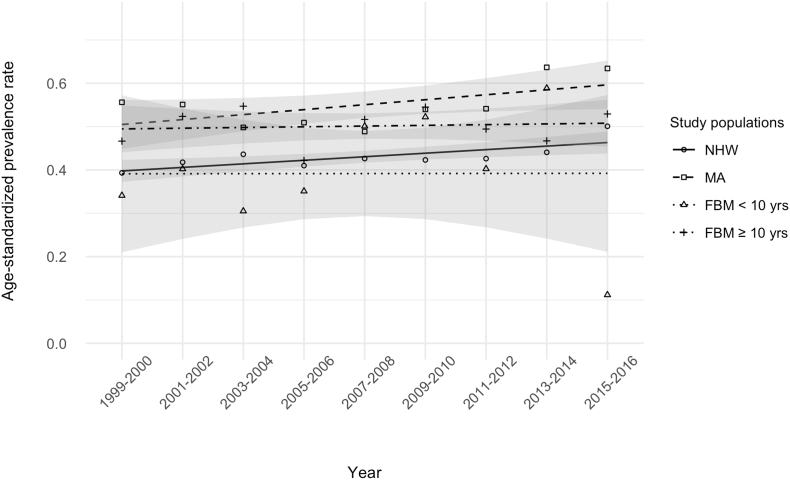
Table 1 also presents the unadjusted and age-standardized health outcomes by study group. Prior to age-standardization, recent Mexican immigrants hold a clear and significant advantage in metabolic health, with lower prevalence rates of low HDL cholesterol, high blood pressure, high waist circumference, obesity, and MetS overall as compared to the other three groups. US-born Mexican Americans and foreign-born Mexicans residing in the US for ten years or more had the highest unadjusted prevalence rates of MetS overall, along with high levels of many of the individual high-risk metabolic health indicators. Upon standardizing all of the study groups to the 2000 US Census age distribution, the recent immigrant health advantage in MetS over US-born whites disappears. However, a significant advantage remains for recent Mexican immigrants over earlier Mexican immigrants and US-born Mexican Americans. Fig. 1 portrays these age-standardized trends in MetS over the eighteen-year study period, with recent Mexican immigrants and US-born whites holding lower prevalence rates of MetS at the beginning of the period, but a less distinct advantage over the other two groups by the end of the period. This figure also reveals that both US-born groups held trajectories of increasing MetS prevalence over the study period, while both groups of Mexican immigrants are seen to follow relatively flat overall trends.
Fig. 1.
Age-standardized metabolic syndrome (MetS) prevalence by race-ethnicity, country of origin, and duration of residence: US-residing adults in the National Health and Nutrition Examination Survey (NHANES, 1999–2016) (N = 10,833)
Notes. Prevalence rates for each two-year study period (presented as point estimates) are age-standardized to the US population distribution according to the 2000 US Census and incorporate survey weights to generate nationally representative estimates. A GLM smoothing function is applied to overlay the trends in metabolic syndrome for each group over the eighteen-year study period. The study populations are abbreviated as follows: US-born non-Hispanic whites (NHW), US-born Mexican Americans (MA), foreign-born Mexicans residing in the US for less than ten years (FBM < 10 yrs), and foreign-born Mexicans residing in the US for ten years or more (FBM ≥ 10 yrs).
4.2. Decomposition
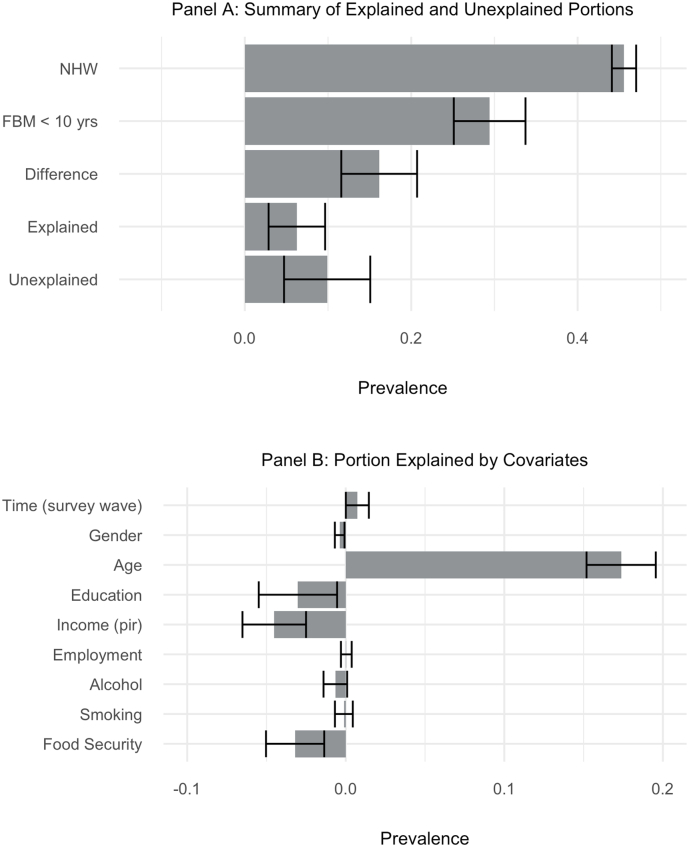
The results of the decomposition analysis are summarized in Fig. 2. Panel A depicts the unadjusted MetS prevalence rates for US-born whites (45.5%) and recent Mexican immigrants (29.5%), as well the prevalence difference between the two groups (16.0%). The explained portion in Panel A indicates that nearly 40% of the prevalence difference (i.e., 6.1 prevalence points) would be eliminated if associations were causal and the two groups had the same mean level on all model variables. Conversely, the remaining ∼60% of the gap (9.9 prevalence points) would theoretically remain under these same conditions. Panel B summarizes the contribution of each study variable to the explained portion of the MetS prevalence difference between US-born whites and recent Mexican immigrants. While the full prevalence difference is accounted for by the younger age structure of recent Mexican immigrants as compared to US-born whites (i.e., statistically-explaining 17.4 prevalence points), this group would retain a sizable metabolic health advantage of roughly 11.6 prevalence points, even after adjusting for age differences, if they were to achieve parity with US-born whites on education (3.2 prevalence points), income levels (4.5 prevalence points), drinking behavior (0.7 prevalence points), and levels of food security (3.2 prevalence points).
Fig. 2.
Decomposition of the prevalence difference in metabolic syndrome (MetS) between US-born non-Hispanic whites and foreign-born Mexicans residing in the US < 10 years (NHANES, 1999–2016) (N = 8191)
Notes. Panel A summarizes the explained and unexplained portions of a two-way, logistic regression-based Oaxaca-Blinder decomposition of the prevalence difference in metabolic syndrome between non-Hispanic whites (NHW) and recent Mexican immigrants (FBM < 10 yrs). Panel B portrays the individual contribution of each study variable to the explained portion of the decomposition.
4.3. Multivariate and predictive models
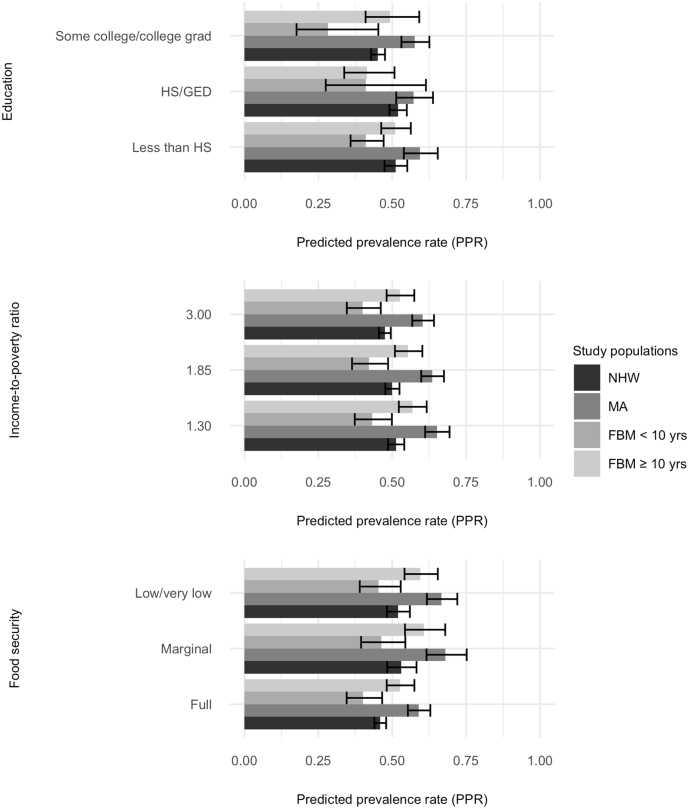
Fig. 3 presents the predicted prevalence rate of MetS associated with specified levels of the three social factors found to have the greatest potential to improve recent Mexican immigrants’ metabolic health: education, income, and food security. Consistent with the results of the decomposition, recent Mexican immigrants are shown to retain a metabolic health advantage over US-born whites when both groups are assigned the same fixed level on each of these measures. Of note, while US-born Mexican Americans and foreign-born Mexicans residing in the US for ten or more years also receive relative improvements in their metabolic health risk from increasing education, income, and food security, these gains are not sufficient to overcome their metabolic health disadvantage relative to US-born whites and recent Mexican immigrants. The underlying Poisson regression model from which the predicted prevalence rates were derived is summarized in Table A.1 of the supplemental online files and the full set of predicted prevalence rates associated with all study measures is summarized in Table A.2.
Fig. 3.
Predicted prevalence rates of metabolic syndrome (MetS) associated with select demographic, socioeconomic, and health behavior characteristics by race-ethnicity, country of origin, and duration of residence: US-residing adults in the National Health and Nutrition Examination Survey (NHANES, 1999–2016) (N = 10,833)
Notes. Predicted prevalence rate (PPR) associated with key independent variables (holding age at the sample mean of 46.5 and all other covariates at their observed levels for each individual) by race-ethnicity/country of origin/duration of residence group. Predicted rates are based on an underlying Poisson regression model with a log link function and robust standard errors, used to directly estimate the prevalence rate ratio between groups.
5. Discussion
In this paper we first aimed to determine whether the Hispanic advantage in mortality extends to a lower risk of the major chronic conditions which constitute metabolic syndrome among recent Mexican immigrants to the US. We find that recent Mexican immigrants do exhibit an overall metabolic health advantage, which is largely attributed to their younger age structure compared to earlier Mexican immigrants, US-born Mexican Americans, and US-born whites. We then explored how key demographic, socioeconomic, and health behavior characteristics contribute to the prevalence of MetS among foreign-born and US-born Mexican Americans relative to US-born whites. The insights from this analysis advance our knowledge of how key characteristics relate to the metabolic health of Mexican immigrants and illuminate areas of policy intervention that may help to preserve their health, and that of their descendants, with increasing time spent in the United States.
A small number of nationally-representative studies have previously explored whether the Hispanic advantage in mortality extends to a lower risk of the major chronic conditions which constitute MetS and related syndromes (Boen & Hummer, 2019; Crimmins et al., 2007; Zhang et al., 2012), all reporting no significant Hispanic metabolic health advantage after adjusting for basic demographic factors, such as age, gender, and/or marital status. Yet given sample size and data constraints, each of these earlier studies was prevented from further stratifying by country of origin and duration of residence, which are notable limitations given that foreign-born Mexicans residing in the US for less than a decade typically hold the greatest overall health and mortality advantages (Antecol & Bedard, 2006; Markides & Eschbach, 2005). The present study improves on these limitations, yet reaches a similar conclusion, as we found that the full prevalence difference in MetS between recent Mexican immigrants and US-born whites was more than accounted for by the immigrants' younger age structure. However, our results also reveal that recent Mexican immigrants would retain a sizable metabolic health advantage, regardless of age structure, if they were to achieve parity with US-born whites in terms of educational attainment, income levels, and food security. This finding aligns with prior research suggesting that Hispanics’ mortality levels would be even more favorable if not for their socioeconomic disadvantage (Lariscy et al., 2015). Additionally, though not sufficient to overcome their significant metabolic health disadvantage, US-born Mexican Americans and earlier Mexican immigrants were also predicted to see relative improvements in their MetS risk from higher levels of education, income, and food security. These results highlight the need to take a preventive, social determinants focused approach in supporting newly-arrived immigrants in maintaining their health upon migrating to the US.
Policy solutions are needed to help resolve many of the socioeconomic inequalities immigrants face. Our results support focusing on policies that would help to resolve immigrant-native disparities in income, food security, and education, such as equitable pathways to citizenship and robust worker protections. A path to citizenship has already been proposed for undocumented agricultural workers under the House-approved, Senate-pending Farm Workforce Modernization Act of 2021 (H.R.1603) (Lofgren, 2021). Additional legislation could also help to ensure all undocumented workers, whose labor currently upholds multiple sectors of the US economy, are able to receive livable wages, safe and humane work and living conditions, and robust enforcement of these protections. Short of providing a pathway to citizenship and extending additional protections for migrant workers, both the food insecurity and immediate financial precarity faced by newly-arrived immigrants could be partially addressed by de-coupling the eligibility for federal and state-based welfare programs—such as SNAP benefits, housing assistance, disability and unemployment, Medicaid, and SSI—from documentation status, especially since undocumented immigrants already pay billions of dollars into these programs annually (Southern Poverty Law Center, 2010). The expected impact on metabolic health from this proposed shift in policy is further supported by recent research showing that unauthorized Hispanic immigrants face significantly heightened risks of weight gain and obesity with time spent in the US relative to their co-ethnic peers who hold legal residence status (Altman & Bachmeier, 2021).
Improving the educational attainment of adult immigrants will likely prove difficult under any policy regime, but opportunities to pursue higher education should be safeguarded and expanded for those who migrate as children or teenagers. While young immigrants are currently able to seek protections under the Deferred Action for Childhood Arrivals (DACA) policy, as a temporary work permit program, DACA has been shown to present barriers to higher education by incentivizing work over educational investment (Hsin & Ortega, 2018). In a recent session of Congress the House approved the American Dream and Progress Act of 2019 before it stalled in the Senate, which would have offered young immigrants permanent legal status (H.R.6) (Roybal-Allard, 2019). The passage of this more expansive legislation would be expected to have a significant impact on reducing barriers to educational attainment for young immigrants (Francesc et al., 2019). Our findings suggest that policy solutions are needed to address socioeconomic inequality and support immigrant health, and a variety of recent legislative efforts have been aligned with this goal; what is needed now is the political will to pass them.
While this study offers significant contributions to the current literature on the health of Mexican immigrants to the US, it also presents limitations. First, our study faces a number of possible selection issues. Given that we do not have access to data from the counterfactual population of Mexicans who did not migrate to the US, we cannot assess healthy migrant selection effects as part of the explanation for recent Mexican immigrants' initial metabolic health advantage relative to the other groups in our sample. This is notable since other researchers able to combine data from NHANES (1999–2010) with data from the Mexican National Health and Nutrition Survey (2006) have found evidence of a modest migrant selection effect contributing to foreign-born Mexicans’ metabolic health advantage relative to non-Hispanic whites (Beltrán-Sánchez et al., 2016). Related to this, we also cannot rule out the presence of selection bias into the NHANES sample, as it is possible that immigrants selected and willing to respond may differ in systematic and consequential ways from those not selected or not willing to respond to survey administrators. However, even in the presence of unmeasured migrant selection effects, our results offer valuable insight into key factors that influence the health of those who did migrate and now reside in the US.
The second area of limitation relates to the cross-sectional nature of our data source, which prevents causal conclusions from being drawn from our analysis. In attempt to minimize likely sources of reverse causation bias, we included measures that would be difficult for respondents to alter in response to a change in health status or diagnosis. However, this precaution also prevented us from including certain measures known to have strong associations with metabolic health, such as dietary intake and physical activity, which may have introduced possible omitted variable bias. The cross-sectional nature of our data also prevented us from directly assessing how the metabolic health of the immigrants in our sample might be affected by the accumulated stresses and opportunities encountered through the process of migration and acculturation. Finally, given our limited sample of foreign-born Mexicans, we were unable to model our outcomes separately for each gender.
6. Conclusion
This study fills a critical gap in our knowledge of how key social and behavioral characteristics influence the metabolic health of first- and later-generation Mexican immigrants, at a time when the prevalence of major chronic metabolic conditions like obesity and diabetes are continuing to rise in both Mexico and the United States. To ensure that newly-arrived Mexican immigrants and their descendants continue to enjoy historically-documented health and mortality advantages in the future, modest changes in US immigration and social policy could help to offer health-promoting protections in the form of increased economic and food security, as well as improved educational opportunities for younger immigrants.
Credit author statement
Maria Carabello: Conceptualization, Data Curation, Formal Analysis, Funding Acquisition, Methodology, Writing – Original Draft, Writing – Review & Editing, Visualization. Julia A. Wolfson: Conceptualization, Data Curation, Funding Acquisition, Supervision, Writing – Review & Editing.
Ethical statement
This research was conducted using publicly available data from the National Health and Nutritional Examination Survey (NHANES), a de-identified population health data source maintained by the National Center of Health Statistics (NCHS). Our secondary analysis of this data was ruled exempt from regulation by the Health Sciences and Behavioral Sciences Institutional Review Board at the University of Michigan (HUM00154839).
Declaration of competing interest
None.
Acknowledgments
Maria Carabello's research on this project was supported by the National Institute on Aging of the National Institutes of Health (Award #T32AG000221 and #T32AG027708). Julia A. Wolfson was supported by the National Institutes of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (Award #K01DK119166). The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institute on Aging or the National Institutes of Diabetes and Digestive and Kidney Diseases. The authors would like to thank participants of the Inequality and Social Demography Workshop at the University of Michigan for their comments on an earlier version of this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100932.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abraído-Lanza A.F., Armbrister A.N., Flórez K.R., Aguirre A.N. Toward a theory-driven model of acculturation in public health research. American Journal of Public Health. 2006;96(8):1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza A.F., Dohrenwend B.P., Ng-Mak D.S., Turner J.B. The Latino mortality paradox: A test of the “salmon bias” and healthy migrant hypotheses. American Journal of Public Health. 1999;89(10):1543–1548. doi: 10.2105/AJPH.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akresh I.R. Overweight and obesity among foreign-born and U.S.-born Hispanics. Biodemography and Social Biology. 2008;54(2):183–199. doi: 10.1080/19485565.2008.9989141. [DOI] [PubMed] [Google Scholar]
- Alberti K.G.M.M., Eckel R.H., Grundy S.M., Zimmet P.Z., Cleeman J.I., Donato K.A., Fruchart J.-C., James W.P.T., Loria C.M., Smith S.C. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood Institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- Allison P.D. SAGE Publications; 2001. Missing data. [DOI] [Google Scholar]
- Altman C.E., Bachmeier J.D. The weight of being unauthorized? Legal status variation in the association between US exposure and obesity among hispanic immigrants in Los Angeles. Journal of Immigrant and Minority Health. 2021;23(5):936–945. doi: 10.1007/s10903-021-01210-x. [DOI] [PubMed] [Google Scholar]
- Antecol H., Bedard K. Unhealthy assimilation: Why do immigrants converge to American health status levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Barquera S., Hernández-Barrera L., Trejo B., Shamah T., Campos-Nonato I., Rivera-Dommarco J. Obesidad en México, prevalencia y tendencias en adultos. Ensanut 2018-19. Salud Pública de México. 2020;62(6, Nov-Dic):682–692. doi: 10.21149/11630. [DOI] [PubMed] [Google Scholar]
- Barquera S., Rivera J.A. Obesity in Mexico: Rapid epidemiological transition and food industry interference in health policies. The Lancet Diabetes & Endocrinology. 2020;8(9):746–747. doi: 10.1016/S2213-8587(20)30269-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barros A.J., Hirakata V.N. Alternatives for logistic regression in cross-sectional studies: An empirical comparison of models that directly estimate the prevalence ratio. BMC Medical Research Methodology. 2003;3(1):21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltrán-Sánchez H., Palloni A., Riosmena F., Wong R. SES gradients among Mexicans in the United States and in Mexico: A new twist to the hispanic paradox? Demography. 2016;53(5):1555–1581. doi: 10.1007/s13524-016-0508-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blinder A.S. Wage discrimination: Reduced form and structural estimates. Journal of Human Resources. 1973;8(4):436–455. doi: 10.2307/144855. JSTOR. [DOI] [Google Scholar]
- Blue L., Fenelon A. Explaining low mortality among US immigrants relative to native-born Americans: The role of smoking. International Journal of Epidemiology. 2011;40(3):786–793. doi: 10.1093/ije/dyr011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen C.E., Hummer R.A. Longer—but harder—lives?: The Hispanic health paradox and the social determinants of racial, ethnic, and immigrant–native health disparities from midlife through late life. Journal of Health and Social Behavior. 2019;60(4):434–452. doi: 10.1177/0022146519884538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Silva E. Rethinking racism: Toward a structural interpretation. American Sociological Review. 1997;62(3):465. doi: 10.2307/2657316. [DOI] [Google Scholar]
- Brown T.H. Racial stratification, immigration, and health inequality: A life course-intersectional approach. Social Forces. 2018;96(4):1507–1540. doi: 10.1093/sf/soy013. [DOI] [Google Scholar]
- Buttenheim A.M., Pebley A.R., Hsih K., Chung C.Y., Goldman N. The shape of things to come? Obesity prevalence among foreign-born vs. US-born Mexican youth in California. Social Science & Medicine. 2013;78:1–8. doi: 10.1016/j.socscimed.2012.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho Y., Frisbie W.P., Hummer R.A., Rogers R.G. Nativity, duration of residence, and the health of Hispanic adults in the United States. International Migration Review. 2004;38(1):184–211. doi: 10.1111/j.1747-7379.2004.tb00193.x. [DOI] [Google Scholar]
- Crimmins E.M., Hayward M.D., Seeman T.E. In: Critical perspectives on racial and ethnic differences in health in late life. Anderson N.B., Bulatao R.A., Cohen B., editors. 2004. Race/ethnicity, socioeconomic status, and health.http://www.ncbi.nlm.nih.gov/books/NBK25526/ National Academies Press (US) [PubMed] [Google Scholar]
- Crimmins E.M., Kim J.K., Alley D.E., Karlamangla A., Seeman T. Hispanic paradox in biological risk profiles. American Journal of Public Health. 2007;97(7):1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre M.E., Gu D., Vaupel J.W. Survival differences among native-born and foreign-born older adults in the United States. PloS One. 2012;7(5):e37177. doi: 10.1371/journal.pone.0037177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckel R.H., Alberti K., Grundy S.M., Zimmet P.Z. The metabolic syndrome. The Lancet. 2010;375(9710):181–183. doi: 10.1016/S0140-6736(09)61794-3. [DOI] [PubMed] [Google Scholar]
- Eckel R.H., Grundy S.M., Zimmet P.Z. The metabolic syndrome. The Lancet. 2005;365(9468):1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- Elo I.T., Turra C.M., Kestenbaum B., Ferguson B.R. Mortality among elderly Hispanics in the United States: Past evidence and new results. Demography. 2004;41(1):109–128. doi: 10.1353/dem.2004.0001. [DOI] [PubMed] [Google Scholar]
- Feliciano C. Educational selectivity in U.S. Immigration: How do immigrants compare to those left behind? Demography. 2005;42(1):131–152. doi: 10.1353/dem.2005.0001. [DOI] [PubMed] [Google Scholar]
- Fenelon A. Revisiting the Hispanic mortality advantage in the United States: The role of smoking. Social Science & Medicine. 2013;82:1–9. doi: 10.1016/j.socscimed.2012.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal K.M., Carroll M.D., Kit B.K., Ogden C.L. Prevalence of obesity and trends in the distribution of body mass index among US Adults, 1999-2010. JAMA. 2012;307(5):491. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Flegal K.M., Kruszon-Moran D., Carroll M.D., Fryar C.D., Ogden C.L. Trends in obesity among adults in the United States, 2005 to 2014. Journal of the American Medical Association. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francesc O., Ryan E., Amy H. The economic effects of providing legal status to DREAMers. IZA Journal of Labor Policy. 2019;9(1) doi: 10.2478/izajolp-2019-0005. [DOI] [Google Scholar]
- Goldman N. Will the Latino mortality advantage endure? Research on Aging. 2016;38(3):263–282. doi: 10.1177/0164027515620242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N., Pebley A.R., Creighton M.J., Teruel G.M., Rubalcava L.N., Chung C. The consequences of migration to the United States for short-term changes in the health of Mexican immigrants. Demography. 2014;51(4):1159–1173. doi: 10.1007/s13524-014-0304-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman B.K., Read J.G., Krueger P.M. Gender, acculturation, and health among Mexican Americans. Journal of Health and Social Behavior. 2010 doi: 10.1177/0022146510386792. [DOI] [PubMed] [Google Scholar]
- Gutin I., Hummer R.A. Social inequality and the future of US life expectancy. Annual Review of Sociology. 2021;47(1) doi: 10.1146/annurev-soc-072320-100249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward M.D., Hummer R.A., Chiu C.-T., González-González C., Wong R. Does the Hispanic Paradox in U.S. adult mortality extend to disability? Population Research and Policy Review. 2014;33(1):81–96. doi: 10.1007/s11113-013-9312-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House J.S. Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. Journal of Health and Social Behavior. 2002;43(2):125–142. doi: 10.2307/3090192. [DOI] [PubMed] [Google Scholar]
- Hsin A., Ortega F. The effects of Deferred Action for Childhood Arrivals on the educational outcomes of undocumented students. Demography. 2018;55(4):1487–1506. doi: 10.1007/s13524-018-0691-6. [DOI] [PubMed] [Google Scholar]
- Hummer R.A., Gutin I. In: “. Hayward M.D., Majmundar M.K., editors. The National Academies Press; Washington, DC: 2018. Racial/ethnic and nativity disparities in the health of older US men and women.” pp. 31–66 in future directions for the Demography of aging: Proceedings of a Workshop. [DOI] [PubMed] [Google Scholar]
- Hummer Robert A., Powers Daniel A., Pullum Starling G., Gossman Ginger L., Frisbie W. Parker. Paradox found (again): Infant mortality among the Mexican-origin population in the United States. Demography. 2007;44(3):441–457. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J., VanderWeele T. Decomposition analysis to identify intervention targets for reducing disparities. Epidemiology. 2018;29(6):825–835. doi: 10.1097/EDE.0000000000000901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitagawa E.M. Components of a difference between two rates. Journal of the American Statistical Association. 1955;50(272):1168–1194. doi: 10.2307/2281213. [DOI] [Google Scholar]
- Klein R.J., Schoenborn C.A. American Psychological Association; 2001. Age adjustment using the 2000 projected U.S. population. [DOI] [PubMed] [Google Scholar]
- Lariscy J.T. Differential record linkage by hispanic ethnicity and age in linked mortality studies: Implications for the epidemiologic paradox. Journal of Aging and Health. 2011;23(8):1263–1284. doi: 10.1177/0898264311421369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lariscy J.T., Hummer R.A., Hayward M.D. Hispanic older adult mortality in the United States: New estimates and an assessment of factors shaping the Hispanic Paradox. Demography. 2015;52(1):1–14. doi: 10.1007/s13524-014-0357-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levchenko Y. Disability crossover among Mexican immigrants in America, America. Social Science & Medicine. 2021;285:114290. doi: 10.1016/j.socscimed.2021.114290. Aging into disadvantage. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lofgren, Z. (2021, March 22). H.R.1603-117th Congress (2021-2022): Farm Workforce Modernization Act of 2021 (2021/2022) [Legislation]. https://www.congress.gov/bill/117th-congress/house-bill/1603.
- Markides K.S., Coreil J. The health of Hispanics in the southwestern United States: An epidemiologic paradox. Public Health Reports. 1986;101(3):253–265. https://www.jstor.org/stable/4627869 [PMC free article] [PubMed] [Google Scholar]
- Markides K.S., Eschbach K. Aging, migration, and mortality: Current status of research on the Hispanic Paradox. Journal of Gerontology: Serie Bibliographique. 2005;60(S2):S68–S75. doi: 10.1093/geronb/60.Special_Issue_2.S68. [DOI] [PubMed] [Google Scholar]
- Markides K.S., Eschbach K., Ray L.A., Peek M.K. In: The health of aging Hispanics: The Mexican-origin population. Angel J.L., Whitfield K.E., editors. Springer; 2007. Census disability rates among older people by race/ethnicity and type of Hispanic origin; pp. 26–39. [DOI] [Google Scholar]
- Monteverde M., Noronha K., Palloni A., Novak B. Obesity and excess mortality among the elderly in the United States and Mexico. Demography. 2010;47(1):79–96. doi: 10.1353/dem.0.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics (NCHS) U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Hyattsville, MD: 1999-2016. National health and nutritional examination survey.https://wwwn.cdc.gov/nchs/nhanes/ [Google Scholar]
- National Center for Health Statistics (NCHS) 2013. National health and nutrition examination survey: Analytic guidelines, 1999-2010.https://stacks.cdc.gov/view/cdc/21305 [PubMed] [Google Scholar]
- National Center for Health Statistics (NCHS) 2018. National health and nutrition examination survey: Analytic guidelines, 2011-2016.https://wwwn.cdc.gov/nchs/data/nhanes/analyticguidelines/11-16-analytic-guidelines.pdf [Google Scholar]
- Oaxaca R. Male-female wage differentials in urban labor markets. International Economic Review. 1973;14(3):693–709. doi: 10.2307/2525981. JSTOR. [DOI] [Google Scholar]
- Ogden C.L., Fryar C.D., Martin C.B., Freedman D.S., Carroll M.D., Gu Q., Hales C.M. Trends in obesity prevalence by race and Hispanic origin—1999-2000 to 2017-2018. JAMA, 324(12) 2020 doi: 10.1001/jama.2020.14590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omran A.R. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Memorial Fund Quarterly. 1971;49(4):509–538. doi: 10.2307/3349375. [DOI] [PubMed] [Google Scholar]
- Orrenius P.M., Zavodny M. Do immigrants work in riskier jobs? Demography. 2009;46(3):535–551. doi: 10.1353/dem.0.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palloni A., Arias E. Paradox lost: Explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annual Review of Sociology. 2015;41(1):311–330. doi: 10.1146/annurev-soc-073014-112305. [DOI] [Google Scholar]
- Popkin B.M. In: Nutrition and health in developing countries. Semba R.D., Bloem M.W., editors. Humana Press; 2001. The nutrition transition and its relationship to demographic change; pp. 427–445. [DOI] [Google Scholar]
- Popkin B.M., Adair L.S., Ng S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutrition Reviews. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portes A., Zhou M. The new second generation: Segmented assimilation and its variants. The Annals of the American Academy of Political and Social Science. 1993;530(1):74–96. doi: 10.1177/0002716293530001006. [DOI] [Google Scholar]
- Riosmena F., Wong R., Palloni A. Migration selection, protection, and acculturation in health: A binational perspective on older adults. Demography. 2013;50(3):1039–1064. doi: 10.1007/s13524-012-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera J.A., Barquera S., González-Cossío T., Olaiz G., Sepúlveda J. Nutrition transition in Mexico and in other Latin American countries. Nutrition Reviews. 2004;62:S149–S157. doi: 10.1111/j.1753-4887.2004.tb00086.x. [DOI] [PubMed] [Google Scholar]
- Roybal-Allard, L. (2019, June 10). H.R.6-116th Congress (2019-2020): American Dream and Promise Act of 2019 (2019/2020) [Legislation]. https://www.congress.gov/bill/116th-congress/house-bill/6.
- Singh G.K., Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: An analysis of two national data bases. Human Biology. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- Southern Poverty Law Center . 2010. Injustice on our plates.https://www.splcenter.org/20101107/injustice-our-plates [Google Scholar]
- Thow A.M. Trade liberalisation and the nutrition transition: Mapping the pathways for public health nutritionists. Public Health Nutrition. 2009;12(11):2150–2158. doi: 10.1017/S1368980009005680. [DOI] [PubMed] [Google Scholar]
- Turra C.M., Elo I.T. The impact of salmon bias on the hispanic mortality advantage: New evidence from social security data. Population Research and Policy Review. 2008;27(5):515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hook J., Quiros S., Frisco M.L., Fikru E. It is hard to swim upstream: Dietary acculturation among Mexican-origin children. Population Research and Policy Review. 2016;35:177–196. doi: 10.1007/s11113-015-9381-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele T.J., Robinson W.R. On causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology. 2014;25(4):473–484. doi: 10.1097/EDE.0000000000000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viruell-Fuentes E.A., Miranda P.Y., Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. Social Science & Medicine. 2012;75(12):2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- Williams D.R. Stress and the mental health of populations of color: Advancing our understanding of race-related stressors. Journal of Health and Social Behavior. 2018;59(4):466–485. doi: 10.1177/0022146518814251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) 2018. Mexico. Noncommunicable diseases (NCD)country profiles.https://www.who.int/nmh/countries/mex_en.pdf?ua=1 Retrieved June 14, 2021, from. [Google Scholar]
- World Health Organization (WHO) 2018. United States of America.Noncommunicable diseases (NCD) country profiles.https://www.who.int/nmh/countries/usa_en.pdf?ua=1 Retrieved June 14, 2021, from. [Google Scholar]
- Zhang Z., Hayward M.D., Lu C. Is there a hispanic epidemiologic paradox in later life? A closer look at chronic morbidity. Research on Aging. 2012;34(5):548–571. doi: 10.1177/0164027511429807. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.