Abstract
Objective: To investigate the application of traditional Chinese medicine (TCM) syndrome differentiation in identification of body constitution of hypertensive and diabetic patients. Methods: A total of 110 hypertensive patients with diabetes treated in our hospital were enrolled in this study, and were divided into a study group (SG, n=60) and a control group (CG, n=50) according to different intervention methods. Patients in the CG received conventional western medical intervention for hypertension and diabetes, while patients in the SG received body constitution-identified TCM syndrome differentiation intervention additionally. The changes of blood pressure and plasma glucose during the intervention were compared between the two groups, the clinical effect and quality of life of the two groups were evaluated, and multivariate stepwise Logistic regression analysis on influencing factor of TCM body constitution was conducted. Results: Compared with that before intervention, the proportion of gentleness constitution in the SG showed a significant increase (P<0.05) after intervention. Dynamic analysis during the intervention showed that patients in the SG had lower systolic blood pressure (SBP), diastolic blood pressure (DBP), lower level of fasting plasma glucose (GLU) and 2-h postprandial plasma glucose (2hPG) than the CG from 1 to 12 months after intervention (P<0.05). Patients in the SG scored higher than the CG on all SF-36 dimensions after intervention (P<0.05). Multivariate stepwise Logistic regression analysis showed that dampness-heat constitution, blood-stasis constitution, Yin-deficiency constitution and phlegm-dampness constitution were the main risk factors for hypertension with diabetes (P<0.05). Conclusion: Body constitution-identified TCM syndrome differentiation treatment for hypertensive patients with diabetes is effective, which can significantly improve the plasma glucose and blood pressure indices of patients. Dampness-heat constitution, blood-stasis constitution, Yin-deficiency constitution and phlegm-dampness constitution are the risk factors for hypertension with diabetes.
Keywords: Traditional Chinese medicine syndrome differentiation, hypertension, diabetes, body constitution identification, application
Introduction
With the improvement of the living standard and adjustment of dietary structure of Chinese residents in recent years, the prevalence of various cardiovascular and cerebrovascular diseases is increasing year by year, which has brought severe burden to the society and also posed a serious threat to the life and health of the residents [1]. Both diabetes and hypertension are the main risk factors for cardiovascular and cerebrovascular diseases, and domestic epidemiological surveys show that the prevalence of hypertension among people over 18 years old in China is as high as 25.2%, and there are approximately 200 million patients of hypertension and 114 million patients of diabetes in China [2,3]. Other studies have shown that the prevalence of diabetes among people over 20 years old in China is about 9.7%, the proportion of people with impaired fasting plasma glucose (GLU) and glucose tolerance (i.e. pre-diabetes) is about 15.5%, and China has currently become another country with a high prevalence of diabetes in the world [4,5].
Diabetes and hypertension can occasionally occur together, and World Health Organization survey found that about 20%-40% of diabetic patients also suffered from hypertension [6], and a 6-year follow-up of 12220 patients showed that the concurrent rate of diabetes was as high as 22.4% in the hypertensive group and 32.4% in those over 60 years old [7]. Clinical practice has indicated [8,9] that both hypertension and diabetes are independent risk factors for onset of cardiovascular and cerebrovascular events, and the impairment of vascular function in hypertensive patients with diabetes is significantly more severe than those with hypertension or diabetes alone, and the reason might be that they can act synergistically to increase the incidence of cardiovascular lesions, cerebrovascular lesions, and small vessel lesions.
Early attention and intervention are of great significance to improve the prognosis of hypertensive patients with diabetes and reduce the risk of cardiovascular and cerebrovascular events [10]. The theory of traditional Chinese medicine (TCM) body constitution quotes the TCM holistic concept, which advocates taking the individual as the study’s starting point and analyzing the pathophysiological characteristics of people with different body constitution types to analyze the disease response and status, nature of lesions and development trend and give treatment based on the TCM syndrome differentiation theory [11]. This intervention has achieved good results in clinical practice, and the results of a follow-up study on stroke patients have shown that syndrome differentiation treatment based on TCM body constitution theory has good clinical intervention effect and can significantly improve neurological function and quality of life of stroke patients, which is of high clinical application [12]. The purpose of this study was to investigate the feasibility and effectiveness of body constitution-identified TCM syndrome differentiation treatment in hypertensive patients with diabetes, so as to provide clinical reference for improving the prognosis of such patients.
Materials and methods
General data
A total of 110 hypertensive patients with diabetes treated in Beijing University of Chinese Medicine from January 2018 to January 2020 were enrolled in this study, and were divided into a study group (SG, n=60) and a control group (CG, n=50) according to different intervention methods.
Inclusion criteria
(1) All participants met the diagnostic criteria for hypertension and diabetes [13]; (2) Subjects had clear consciousness and were able to cooperate with the study; (3) The clinical data were complete; (4) Subjects gave informed consent to the study and signed an informed consent form; (5) Subjects voluntarily accepted the test and survey; (6) Subjects aged 30-80 years; (7) The study has been reported and approved for implementation by the Ethics Committees of Beijing University of Chinese Medicine.
Exclusion criteria
(1) Individuals diagnosed with secondary hypertension; (2) Individuals diagnosed with a mental illness; (3) Individuals diagnosed with any other systemic disease such as primary liver, kidney and lung disease; (4) Individuals who had not given informed consent; (5) Individuals with alcohol or drug dependence; (6) Individuals who had participated in and had not completed any other clinical studies; (7) Individuals voluntarily requested to withdraw from the study; (8) Individuals lost to follow-up during the study.
Intervention method
Study content
The general clinical data of the two groups were collected, mainly including gender, age, occupation, past medical history, family history, smoking history, alcohol drinking history, height, weight, etc.
Intervention method
The CG received conventional interventions for hypertension and diabetes, including conventional health education, low-salt and low-fat diet, smoking and alcohol cessation, regular exercise, etc., and regular medication (hypoglycemic and antihypertensive drugs) under medical supervision according to the actual conditions of patients.
In addition to interventions in the CG, the SG received body constitution-identified TCM syndrome differentiation treatment. Firstly, the physicians were trained in TCM body constitution identification, and the TCM body constitution scale was defined (according to the “Classification and Determination of Physical Constitutions in TCM” by the Chinese Medical Association in 2009 [14]). Each subscale comprises 8 questions with a total score of 40, and each item was given a score from 1-5. Patients with a score of ≥ 30 on the scale were considered to have the corresponding constitution, and in case of two or more scale scores ≥ 30, the scale with the highest score prevailed. If the gentleness constitution score was ≥ 30, all items were retested. The physicians were required to master the wording for questionnaire and know the precautions for investigation. The investigation was carried out in a face-to-face manner. In the premise of informed consent of patients, on-site questionnaires were organized uniformly, and the collected data were then sorted out. According to the scale scores, the participant’s body constitution was identified, based on which syndrome differentiation treatment was given. The specific measures were as follows: Rhizoma Dioscoreae and Semen Lablab Album were taken for Qi deficiency, Semen Juglandis and Cortex Eucommiae were taken for Yang deficiency, Fructus Lycii and Fructus Mori were taken for Yin-deficiency constitution, Exocarpium Citri Rubrum and Poria were taken for Phlegm-dampness constitution, Semen Coicis and Exocarpium Benincasae were taken for dampness-heat constitution, fructus crataegi and Radix et Rhizoma Salviae Miltiorrhizae were taken for Blood-stasis constitution, Fructus Citri Sarcodactylis and Fructus Citri were taken or Qi-depression constitution, and Adix Et Rhizoma Ginseng and Radix Astragali were taken for special diathesis constitution [15]. In addition to dietary therapy, the main TCM-based intervention was acupuncture and moxibustion, with Shenmen and Erjian as primary acupuncture points, and with Fengxi and Fei for Special diathesis constitution, Neifenmi and Gan for Qi-depression constitution, Ganshen for Blood-stasis constitution, Sanjiao for Phlegm-dampness constitution, Pangguang and Pizhixia for Dampness-heat constitution, Jiaogan and Neifenmi for Yin-deficiency constitution, Shenshangxian for Yang-deficiency constitution, and Wei and Fei for Qi-deficiency constitution as adjunct acupuncture points.
Observation indices and evaluation criteria
The main observation indices include four major points: (1) Change in TCM-identified body constitution of the two groups before and after intervention. The TCM-identified body constitution and proportion thereof in two groups before intervention and after 12 months of intervention were summarized, and the inter-group and intra-group differences before and after intervention were compared. (2) Change in blood pressure and plasma glucose of the two groups during intervention. The blood pressure was assessed against two indices of systolic blood pressure (SBP) and diastolic blood pressure (DBP). The testing was carried out in strict with the requirements of the “Chinese Guidelines for Measurement of Blood Pressure” [16], i.e., the patients should not do strenuous activities and eat or drink anything 30 min before test, kept a state of calm relaxation, sit for 5 min and then took their blood pressure in a sitting position, and the right upper arm should be at the level of the sphygmomanometer and heart. Each index was tested three times and the average value was taken as the measurement result, and the plasma glucose was also tested three times consecutively and the average value was taken as the result. (3) Change in quality of life of the two groups before and after intervention. The assessment tool was SF-36 scale [17], which includes 8 aspects such as physical functioning, vitality and emotional functioning, and can be distinguished into 3 major parts: physical functioning, mental functioning and living functioning, and the higher scale score indicates the higher quality of life of the subjects. (4) Multivariate Logistic regression analysis of TCM body constitution in hypertensive patients with diabetics.
Statistical methods
The collected data were entered into the EXCEL table and analyzed using SPSS 22.0 software. The data were analyzed by normal distribution test, and if the data were normally distributed, the counting data were described by constituent ratio and rate. Analysis on inter-group difference was performed by Chi-square test, the measurement data were expressed as (mean ± standard deviation). Analysis on inter-group difference was performed by t-test, and influencing factor of body constitution in case group was analyzed by Logistic regression. P<0.05 was considered statistically significant, and GraphPad Prism 8 was adopted as the graphical software [18].
Results
Comparison of differences in general clinical data between two groups
The general clinical data such as gender, age, mean weight, mean duration of illness, smoking history, and alcohol drinking history of the two groups were summarized separately, meanwhile inter-group differences were compared. The results showed that the differences in general clinical data were not significant between the two groups (P>0.05), suggesting that the two groups were comparable (Table 1).
Table 1.
Comparison of general clinical indices between the two groups (X ± S)/[n (%)]
| General clinical data | Study group (n=60) | Control group (n=50) | t/X2 | P | |
|---|---|---|---|---|---|
| Gender | Male | 37 | 28 | 0.547 | 0.362 |
| Female | 23 | 22 | |||
| Average age (years) | 45.98±4.33 | 46.01±4.29 | 0.036 | 0.987 | |
| Average weight (kg) | 64.29±3.91 | 64.34±3.89 | 0.066 | 0.917 | |
| Average duration of disease (year) | 2.89±0.28 | 2.93±0.18 | 0.871 | 0.317 | |
| Smoking history | Yes | 10 | 10 | 0.652 | 0.204 |
| No | 50 | 40 | |||
| Alcohol drinking history | Yes | 15 | 11 | 0.712 | 0.136 |
| No | 45 | 39 | |||
Analysis of changes in TCM body constitution of the two groups before and after intervention
Statistical analysis was conducted on TCM-identified body constitution of the two groups before intervention and after 12 months of intervention. The inter-group and intra-group differences before and after intervention were compared. The results showed that the inter-group difference in proportion of each TCM-identified body constitution type was not significant (P>0.05) before intervention, while after intervention, the proportion of gentleness constitution in the SG was increased from 5.00% to 18.33%, and the intra-group difference was significant (P<0.05) before and after intervention. The proportion of other body constitution types changed before and after intervention, but the difference was not significant (P>0.05) (Table 2).
Table 2.
Analysis of changes in TCM-identified body constitution of the two groups before and after intervention [n (%)]
| TCM body constitution | Study group (n=60) | X2 | P | Control group (n=50) | X2 | P | ||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Before intervention | After intervention | Before intervention | After intervention | |||||
| Gentleness constitution | 3 (5.00) | 11 (18.33)* | 5.175 | 0.023 | 2 (4.00) | 4 (8.00) | 0.709 | 0.4 |
| Qi-deficiency constitution | 15 (25.00) | 14 (23.33) | 0.045 | 0.831 | 12 (24.00) | 14 (28.00) | 0.208 | 0.648 |
| Yang-deficiency constitution | 11 (18.33) | 10 (16.67) | 0.058 | 0.81 | 10 (20.00) | 12 (24.00) | 0.233 | 0.629 |
| Yin-deficiency constitution | 9 (15.00) | 8 (13.33) | 0.069 | 0.793 | 8 (16.00) | 6 (12.00) | 0.332 | 0.564 |
| Phlegm-dampness constitution | 6 (10.00) | 5 (8.33) | 0.1 | 0.752 | 5 (10.00) | 4 (8.00) | 0.122 | 0.727 |
| Dampness-heat constitution | 5 (8.33) | 4 (6.67) | 0.12 | 0.729 | 5 (10.00) | 5 (10.00) | 0.0 | 1.0 |
| Blood-stasis constitution | 5 (8.33) | 4 (6.67) | 0.12 | 0.729 | 3 (6.00) | 3 (6.00) | 0.0 | 1.0 |
| Qi-depression constitution | 5 (8.33) | 4 (6.67) | 0.12 | 0.729 | 4 (8.00) | 2 (4.00) | 0.709 | 0.4 |
| Special diathesis constitution | 1 (1.67) | 0 (0.00) | 1.008 | 0.315 | 1 (2.00) | 0 (0.00) | 1.01 | 0.315 |
P<0.05 compared with that before intervention.
Dynamic analysis of changes in blood pressure and plasma glucose of the two groups during the intervention
During the intervention, patients in both groups were retested once a month to record the changes in blood pressure and plasma glucose and inter-group comparison was performed. The results showed that the inter-group differences in SBP, DBP, GLU and 2-h postprandial plasma glucose (2Hpg) before intervention were not significant (P>0.05). After intervention, the above indices of the two groups showed a slow decline trend, and the SBP, DBP, GLU and 2hPG of the two groups were reduced significantly after 12 months of intervention compared with those before intervention, and the difference before and after intervention was statistically significant (P<0.05). Meanwhile, the comparison of inter-group difference during the intervention showed that the SBP, DBP, GLU and 2hPG of patients in the SG were all significantly lower than those of patients in the CG from the first month of intervention, and the difference in inter-group comparison was statistically significant (P<0.05) (Figures 1, 2).
Figure 1.

Dynamic analysis of changes in blood pressure of the two groups during the intervention. The blood pressure in both groups from 1 month to 12 months of intervention was dynamically assessed and the inter-group difference was compared. The results showed that SBP (A) and DBP (B) of the study group were significantly lower than those of the control group at each observation point between 1 month and 12 months of intervention (P<0.05). # represents a statistically significant difference between groups for the same index at the same time.
Figure 2.
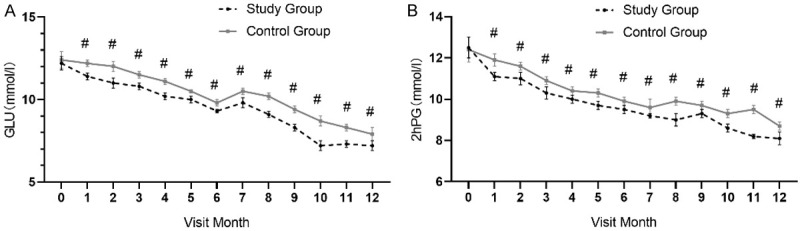
Dynamic analysis of changes in plasma glucose of the two groups during the intervention. The plasma glucose of both groups from 1 month to 12 months of the intervention was dynamically assessed and the inter-group difference was compared. The results showed that the GLU (A) and 2hPG (B) of the study group were significantly lower than those of the control group at each observation point between 1 month and 12 months of intervention (P<0.05). # represents a statistically significant difference between groups for the same index at the same time.
Analysis of changes in quality of life scores of the two groups before and after intervention
The SF-36 scale was used to assess the quality of life of the two groups before intervention and 12 months after intervention. The results showed that the inter-group difference in SF-36 scale score of each dimension before intervention were not statistically significant (P>0.05). The post-intervention comparison showed that the SF-36 scale scores of all dimensions in the SG were all significantly higher than those in the CG, with significant inter-group difference (P<0.05), and comparison of intra-group differences before and after intervention showed that the SF-36 scale score in the SG after intervention was significantly higher than that before intervention (P<0.05) (Figure 3).
Figure 3.
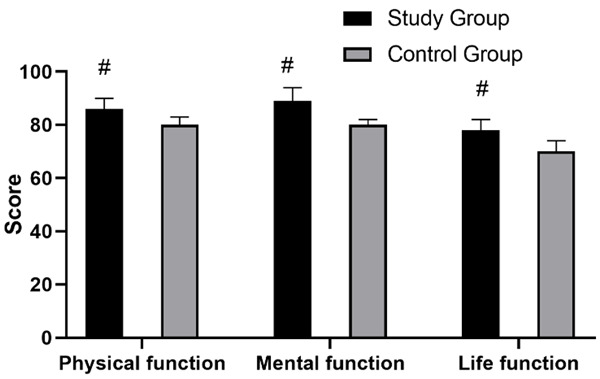
Comparison of quality of life scores between the two groups after intervention. The SF-36 scale scores of physical functioning, mental functioning and living functioning of the study group were all significantly higher than those of the control group after intervention, and the inter-group difference was statistically significant (P<0.05). # represents a statistically significant difference between groups for the same index.
Multivariate stepwise Logistic regression analysis of influencing factor of TCM body constitution
Multiple regression analysis was conducted on TCM body constitution types associated with the occurrence of hypertension with diabetes, with 9 TCM body constitution types as independent variables, where yes =1 and no =0, and hypertension with diabetes as dependent variables, where hypertension with diabetes was 1 and normal individuals was 0. Multiple Logistic regression analysis of hypertension with diabetes was conducted with TCM body constitution types as the independent variables, and at the level of P<0.05, 4 body constitution types in the order of dampness-heat constitution, blood-stasis constitution, Yin-deficiency constitution and phlegm-dampness constitution ranked from the highest to the lowest degree of influence were included in the regression equation, suggesting that the above 4 body constitution types were the main risk factors for hypertension with diabetes (Table 3).
Table 3.
Multivariate stepwise Logistic regression analysis of influencing factor of TCM body constitution in hypertension with diabetes
| Variable | β | S.E | Walds | OR (95% CI) | P |
|---|---|---|---|---|---|
| Dampness-heat constitution | 0.026 | 2.123 | 5.421 | 1.034 (1.002-1.071) | <0.001 |
| Blood-stasis constitution | 1.782 | 0.786 | 6.532 | 1.719 (1.281-2.011) | <0.001 |
| Yin-deficiency constitution | 0.072 | 0.034 | 5.221 | 1.073 (1.011-1.213) | <0.001 |
| Phlegm-dampness constitution | 0.043 | 0.013 | 8.645 | 1.043 (1.011-1.076) | <0.001 |
Discussion
Both hypertension and diabetes are common medical diseases [19]. Epidemiological investigation shows that changes in dietary structure and lifestyle of the population in recent years have led to a significant increase in the incidence of hypertension and diabetes compared with the past [20]. It is found that the risk of cardiovascular and cerebrovascular diseases will increase geometrically in individuals with diabetes and hypertension, with a significant increase in vascular damage as well as incidence of various macrovascular and microvascular complications such as coronary heart disease, cerebrovascular disease, renal atherosclerosis, and diabetic retinopathy [21]. The intervention principle of western medicine for these conditions is mostly passive control of blood pressure and plasma glucose. Studies have shown that the use of antidiabetic and antihypertensive drugs can significantly reduce the incidence of myocardial infarction and major cardiovascular events [22], while some studies have found that the effect of single use of western medicine is unstable and adverse effects of long-term medication are obvious [23].
In this study, we investigated the effect of body constitution-identified TCM syndrome differentiation treatment on hypertensive patients with diabetes. Before intervention, the gentleness constitution type and imbalanced constitution type accounted for 5.00% and 95.00% respectively in the SG (n=60 patients), and the proportion were 4.00% and 96.00% in the CG (n=50). The difference in TCM body constitution proportion between the two groups before intervention was not significant (P>0.05). After TCM syndrome differentiation treatment, the proportion of gentleness constitution in the SG increased to 18.33%, which was significantly higher than 8.00% in the CG, and the inter-group difference was significant, indicating that syndrome differentiation treatment effectively improved the viscera function of the study subjects. A similar study on 100 hypertensive patients with type 2 diabetes showed that the proportion of gentleness constitution in the SG receiving syndrome differentiation treatment increased from 4.00% to 20.00% after intervention, and the increasing amplitude was even higher than that in this study [24]. The authors of this study proposed that body constitution is a relatively stable state of the human body, closely related to the individual’s innate and acquired diathesis, and can be reflected in the patient’s mental structure, physical function and psychological state, etc. Through analysis of individual’s physiological and pathological state, the body constitution-identified syndrome differentiation treatment can investigate the body’s response to disease and disease development trend and then carry out targeted interventions. Numerous studies have shown the effectiveness of syndrome differentiation treatment for various disorders such as hypertension, hypertensive nephropathy, diabetes, and diabetic nephropathy [25], which is consistent with the finding that the indices of DBP, SBP, GLU and 2hPG in the SG were all significantly lower than those in the CG during the intervention, suggesting that body constitution-identified syndrome differentiation treatment is more effective than western medical intervention alone in controlling diseases. The comparison of quality of life between the two groups indicated that the good intervention improved patients’ physical, mental and living functioning, and the feasibility of body constitution-identified syndrome differentiation treatment was better for improvement of patients’ quality of life.
The study also analyzed the characteristics of TCM body constitution types in hypertensive patients with diabetes, and the results showed that dampness-heat constitution, blood-stasis constitution, Yin-deficiency constitution and phlegm-dampness constitution were the major risk factors for hypertension with diabetes. Some scholars have pointed out that the current diet structure of Chinese residents is poor, and bad dietary habits such as high salt and high fat are the main risk factors leading to various chronic diseases [26]. Another study analyzed the body constitution of primary hypertension and found that 16.3% of patients had Qi-deficiency constitution, 19.56% of patients had Yang-deficiency constitution, 29.35% of patients had phlegm-dampness constitution, 15.22% of patients had Yin-deficiency constitution, 7.61% of patients had dampness-heat constitution, 6.52% of patients had blood-stasis constitution, 4.35% of patients had Qi-depression constitution, and 1.09% of patients had special diathesis constitution, and the scholars of the research concluded that phlegm-dampness constitution, Yin-deficiency constitution and Yang-deficiency constitution accounted for a higher proportion of the study subjects, and body constitution might also be a factor influencing the occurrence of hypertension [27]. We proposed that dizziness and thirst are related to the individual’s dietary preference, as recorded in the “Internal Canon of Medicine”, and current salty, oily, and salty & spicy diet in China, and excessive consumption of fatty, sweet, rich and greasy products will significantly affect spleen and stomach transportation and transformation, leading to an increase in phlegm and dampness, which will accumulate in the Middle Jiao and lead to thirst, meanwhile, flow of dampness-turbidity into vessels in conjunction with phlegm-stasis will lead to the narrowing of vessels, resulting in poor flow of qi and blood, which is manifested in increased blood pressure. This is also the main reason why individuals with phlegm-dampness constitution, dampness-heat constitution, blood-stasis constitution and Yin-deficiency constitution are prone to hypertension with diabetes.
In conclusion, the effect of body constitution-identified TCM syndrome differentiation treatment for hypertension and diabetes is better, which can significantly improve the plasma glucose and blood pressure indices of patients. Dampness-heat constitution, blood-stasis constitution, Yin-deficiency constitution and phlegm-dampness constitution are the risk factors for hypertension with diabetes. This study also has some limitations. The included sample were from single source and the research time is relatively concentrated, which may affect the research results to some extent and lead to bias. A large-sample and multi-center survey is needed to validate the conclusions above.
Disclosure of conflict of interest
None.
References
- 1.Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol. 2018;34:575–584. doi: 10.1016/j.cjca.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ohishi M. Hypertension with diabetes mellitus: physiology and pathology. Hypertens Res. 2018;41:389–393. doi: 10.1038/s41440-018-0034-4. [DOI] [PubMed] [Google Scholar]
- 3.Yamazaki D, Hitomi H, Nishiyama A. Hypertension with diabetes mellitus complications. Hypertens Res. 2018;41:147–156. doi: 10.1038/s41440-017-0008-y. [DOI] [PubMed] [Google Scholar]
- 4.Tatsumi Y, Ohkubo T. Hypertension with diabetes mellitus: significance from an epidemiological perspective for Japanese. Hypertens Res. 2017;40:795–806. doi: 10.1038/hr.2017.67. [DOI] [PubMed] [Google Scholar]
- 5.Nistala R, Savin V. Diabetes, hypertension, and chronic kidney disease progression: role of DPP4. Am J Physiol Renal Physiol. 2017;312:F661–F670. doi: 10.1152/ajprenal.00316.2016. [DOI] [PubMed] [Google Scholar]
- 6.Alloubani A, Saleh A, Abdelhafiz I. Hypertension and diabetes mellitus as a predictive risk factors for stroke. Diabetes Metab Syndr. 2018;12:577–584. doi: 10.1016/j.dsx.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Strain WD, Paldánius PM. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc Diabetol. 2018;17:57. doi: 10.1186/s12933-018-0703-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mortada I. Hyperuricemia, type 2 diabetes mellitus, and hypertension: an emerging association. Curr Hypertens Rep. 2017;19:69. doi: 10.1007/s11906-017-0770-x. [DOI] [PubMed] [Google Scholar]
- 9.Tsimihodimos V, Gonzalez-Villalpando C, Meigs JB, Ferrannini E. Hypertension and diabetes mellitus: coprediction and time trajectories. Hypertension. 2018;71:422–428. doi: 10.1161/HYPERTENSIONAHA.117.10546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pavlou DI, Paschou SA, Anagnostis P, Spartalis M, Spartalis E, Vryonidou A, Tentolouris N, Siasos G. Hypertension in patients with type 2 diabetes mellitus: targets and management. Maturitas. 2018;112:71–77. doi: 10.1016/j.maturitas.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 11.Maciorkowska M, Musiałowska D, Małyszko J. Adropin and irisin in arterial hypertension, diabetes mellitus and chronic kidney disease. Adv Clin Exp Med. 2019;28:1571–1575. doi: 10.17219/acem/104551. [DOI] [PubMed] [Google Scholar]
- 12.Daly B, Toulis KA, Thomas N, Gokhale K, Martin J, Webber J, Keerthy D, Jolly K, Saravanan P, Nirantharakumar K. Increased risk of ischemic heart disease, hypertension, and type 2 diabetes in women with previous gestational diabetes mellitus, a target group in general practice for preventive interventions: a population-based cohort study. PLoS Med. 2018;15:e1002488. doi: 10.1371/journal.pmed.1002488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta R, Misra A. Contentious issues and evolving concepts in the clinical presentation and management of patients with COVID-19 infectionwith reference to use of therapeutic and other drugs used in co-morbid diseases (hypertension, diabetes etc) Diabetes Metab Syndr. 2020;14:251–254. doi: 10.1016/j.dsx.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bensimhon HF, Cavender MA. Hypertension treatment in diabetes: focus on heart failure prevention. Heart Fail Clin. 2019;15:551–563. doi: 10.1016/j.hfc.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 15.González Albarrán O, Ramírez L. Management of diabetes in patients with hypertension. Hipertens Riesgo Vasc. 2017;34(Suppl 2):30–34. doi: 10.1016/S1889-1837(18)30073-4. [DOI] [PubMed] [Google Scholar]
- 16.Yildiz M, Esenboğa K, Oktay AA. Hypertension and diabetes mellitus: highlights of a complex relationship. Curr Opin Cardiol. 2020;35:397–404. doi: 10.1097/HCO.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 17.Sasaki T, Tsuboi N, Okabayashi Y, Haruhara K, Kanzaki G, Koike K, Takahashi H, Ikegami M, Shimizu A, Yokoo T. Synergistic impact of diabetes and hypertension on the progression and distribution of glomerular histopathological lesions. Am J Hypertens. 2019;32:900–908. doi: 10.1093/ajh/hpz059. [DOI] [PubMed] [Google Scholar]
- 18.Thomas G. Hypertension management in chronic kidney disease and diabetes: lessons from the systolic blood pressure intervention trial. Cardiol Clin. 2019;37:307–317. doi: 10.1016/j.ccl.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Ponirakis G, Petropoulos IN, Alam U, Ferdousi M, Asghar O, Marshall A, Azmi S, Jeziorska M, Mahfoud ZR, Boulton AJM, Efron N, Nukada H, Malik RA. Hypertension contributes to neuropathy in patients with type 1 diabetes. Am J Hypertens. 2019;32:796–803. doi: 10.1093/ajh/hpz058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jacob AM, Muruganathan A, Datta M, Viswanathan V. Prevalence of hypertension among urban poor with and without diabetes - a study from South India. J Assoc Physicians India. 2019;67:41–45. [PubMed] [Google Scholar]
- 21.Wallace K, Zhao X, Misra R, Sambamoorthi U. The humanistic and economic burden associated with anxiety and depression among adults with comorbid diabetes and hypertension. J Diabetes Res. 2018;2018:4842520. doi: 10.1155/2018/4842520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xie F, Xie L, Li X, Lu LX, Ma Y, Zhan QL, Zhong ZH. Prevalence and risk factors of hypertension combined with diabetes in middle and elder population in Nan’an district of Chongqing. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40:666–669. doi: 10.3760/cma.j.issn.0254-6450.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 23.Foguet-Boreu Q, Violán C, López Jiménez T, Pons-Vigués M, Rodríguez-Blanco T, Valderas JM, Guisado Clavero M, Pujol-Ribera E. Pharmacological control of diabetes and hypertension comorbidity in the elderly: a study of “real world” data. Prim Care Diabetes. 2017;11:348–359. doi: 10.1016/j.pcd.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Saxton SN, Clark BJ, Withers SB, Eringa EC, Heagerty AM. Mechanistic links between obesity, diabetes, and blood pressure: role of perivascular adipose tissue. Physiol Rev. 2019;99:1701–1763. doi: 10.1152/physrev.00034.2018. [DOI] [PubMed] [Google Scholar]
- 25.Shalimova A, Fadieienko G, Kolesnikova O, Isayeva A, Zlatkina V, Nemtsova V, Prosolenko K, Psarova V, Kyrychenko N, Kochuieva M. The role of genetic polymorphism in the formation of arterial hypertension, type 2 diabetes and their comorbidity. Curr Pharm Des. 2019;25:218–227. doi: 10.2174/1381612825666190314124049. [DOI] [PubMed] [Google Scholar]
- 26.Wang Z, do Carmo JM, Aberdein N, Zhou X, Williams JM, da Silva AA, Hall JE. Synergistic interaction of hypertension and diabetes in promoting kidney injury and the role of endoplasmic reticulum stress. Hypertension. 2017;69:879–891. doi: 10.1161/HYPERTENSIONAHA.116.08560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.López-Jaramillo P, Barbosa E, Molina DI, Sanchez R, Diaz M, Camacho PA, Lanas F, Pasquel M, Accini JL, Ponte-Negretti CI, Alcocer L, Cobos L, Wyss F, Sebba-Barroso W, Coca A, Zanchetti A Latin American Society of Hypertension Consensus Expert Group. Latin American Consensus on the management of hypertension in the patient with diabetes and the metabolic syndrome. J Hypertens. 2019;37:1126–1147. doi: 10.1097/HJH.0000000000002072. [DOI] [PubMed] [Google Scholar]


