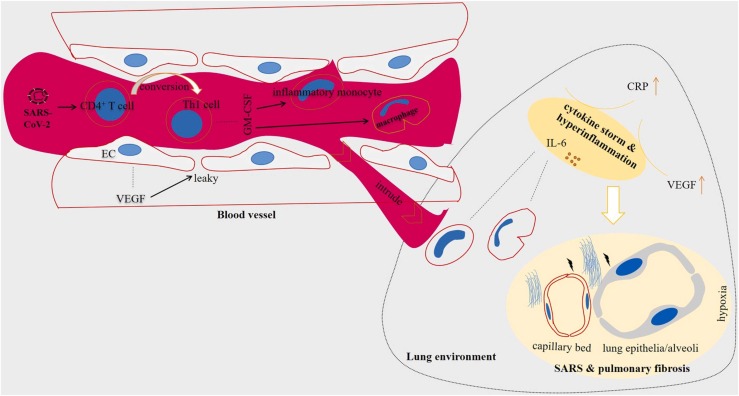
Fig. 2.
Cytokine storm in patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Patients experience a hyperinflammatory state called cytokine storm. SARS-CoV-2 stimulates the activity of CD4+ T cells and their conversion into T helper (Th)−1 cells. The pathogenic Th1 cells release a number of factors including granulocyte-macrophage colony-stimulating factor (GM-CSF) that act for stimulation of inflammatory monocytes and macrophages. The inflammatory monocytes and macrophages intrude lung environment through leaky vessels mediated by vascular endothelial growth factor (VEGF) released from endothelial cells (ECs) of blood vessels. Among a number of factors released from monocytes, over-release of interleukin (IL)−6 takes important roles in the excessive cytokine release. High presence of IL-6 in the area will turn the tissue nearby into developing hypoxia and further damages to lung alveoli and capillary bed, manifested by EC disruption. This will hamper efficient delivery of oxygen, thereby causing shortness of breath, chest thickness and respiratory failure. Fibrotic lungs seen in imaging systems is a result of tissue damage in lung parenchyma. The hypoxic environment also facilitates promotion of coagulopathy-related events.