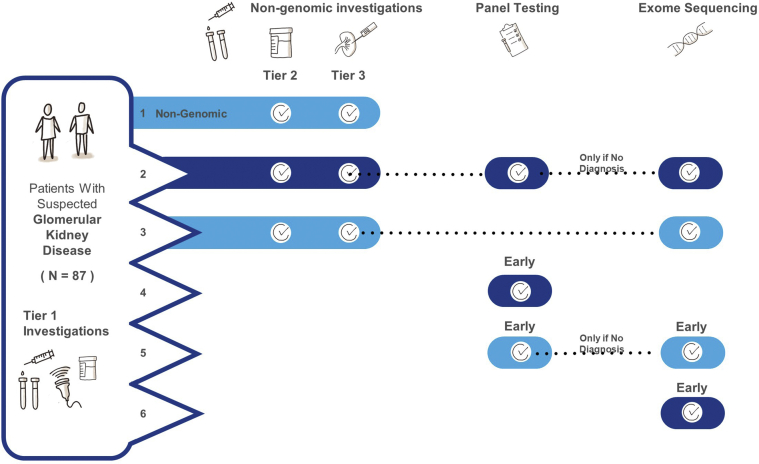
Figure 1.
Diagnostic trajectory and resulting diagnostic yields for standard care and integrating genomic sequencing using 5 models. Adult and pediatric patients were modeled separately for all pathways.
Model 1: Nongenomic investigation (NGI) pathway: a team of 8 nephrologists (including 4 who were not involved with the study) generated a standard care (NGIs) pathway for patients with glomerular disease. These pathways were based on standard order sets in the electronic medical record used in the study site, published guidelines, and literature. Where there was debate regarding standard practice, this was resolved by discussion among the team. Investigations were divided into 3 tiers: (i) baseline investigations that established the clinical differential of glomerular disease and/or required before genomic testing, (ii) complex noninvasive investigations, and (iii) complex invasive investigations.
Model 2: All NGIs are exhausted first, followed by panel testing; if panel testing was nondiagnostic, exome sequencing (ES) would be performed as the final test.
Model 3: All NGIs are exhausted first, followed by ES.
Model 4: Patients had early genomic sequencing (after Tier 1 tests), in the form of panel testing only, followed by ES in unresolved cases.
Model 5: Patients had early panel testing only.
Model 6: Early ES (following Tier 1 tests) in all patients