Abstract
Introduction
To assess the differences between the horizontal white-to-white (WTW) and horizontal sulcus-to-sulcus (STS) diameter measurements, their related factors, and their effects on vault after implantable Collamer lens (ICL) implantation.
Methods
This retrospective study included 429 eyes of 429 patients (145 men and 284 women with a mean age of 29.22 ± 8.06 years) who underwent ICL implantation. The choice of the ICL size depended on the WTW diameter and anterior chamber depth (ACD). The information of WTW diameter, STS diameters, ACD, and their relationships on vault were analyzed.
Results
Horizontal STS and WTW diameters were correlated (r = 0.71, P < 0.001). The mean difference between the STS and WTW diameters was −0.02 ± 0.33 (−1.36 to 1.11) mm. The average vaults of the △STS–WTW < −0.1 group, – 0.1 ≤ △STS–WTW ≤ 0.1 group, and △STS–WTW > 0.1 group were 558.36 ± 163.58 (250–1100) μm, 513.10 ± 121.42 (190–850) μm, and 469.01 ± 133.23 (120–750) μm, respectively. There were significant differences between these groups (P < 0.05). △STS-WTW was correlated with the horizontal STS diameter (r = 0.30, P < 0.001), the WTW diameter (r = −0.17, P = 0.001), and the ACD (r = 0.17, P < 0.001). When the WTW diameter was further away from 11.08 to 12.51 mm or the ACD was further away from 2.81 to 3.74 mm, the difference between the STS and WTW diameters was larger and the correlation between the STS and WTW diameters was weaker.
Conclusions
The difference between the WTW and STS diameters was larger for cases with a WTW diameter or anterior chamber depth outside a certain range; this may be associated with an undesirable vault after ICL implantation. Special attention should be paid to these patients.
Keywords: High myopia, Implantable Collamer lens, Sulcus-to-sulcus, Vault, White-to-white
Key Summary Points
| This is the first large-sample study on the effects of the difference between the white-to-white (WTW) and sulcus-to-sulcus (STS) diameters on vault and its related factors, and it provides clinical and practical value for the selection of implantable Collamer lens (ICL) size. |
| In this study, we found that there was no strong correlation between the WTW and STS diameters. |
| Errors can occur in choosing ICL sizes by the WTW-based prediction of the horizontal ciliary sulcus diameter, which may increase the risk of unsatisfactory intraocular lens vault and instability. |
| The difference between the WTW and STS diameters was large for cases with a WTW diameter or anterior chamber depth out of range; this may be associated with an undesirable vault after ICL implantation. Special attention should be paid to these patients. |
Introduction
In recent years, phakic intraocular lenses, especially the implantable Collamer lens (ICL), have been widely used in the clinic because of the wide refractive correction range [1–3]. The ICL is a type of intraocular lens made of hydrophilic collagen copolymer, with good compatibility. It has been proven to be safe and effective for the correction of moderate and high myopia [4–6]. The appropriate choice of ICL size is the cornerstone for its long-term safety and stability in the eye [7–10]. An oversized ICL can rub the iris, cause depigmentation, and generate angle closure and high intraocular pressure. An undersized ICL can easily lead to intraocular lens rotation, anterior subcapsular opacification, and cataract [11]. Because four haptics of the ICL need to be placed in the ciliary sulcus, the accurate measurement of sulcus-to-sulcus (STS) diameter has an important effect on the choice of the ICL size [12]. However, the repeatability of STS measurement is poor, and patients are not comfortable during the examination, whereas WTW measurement is easy and has good repeatability [13]. Therefore, increasing the value of the horizontal corneal diameter by 0.5–1.0 mm based on the anterior chamber depth (ACD) is traditionally used to estimate the diameter of the ciliary sulcus [12]. However, the vault of the ICL size based on the WTW diameter has been found not to be ideal in several cases [14].
The purpose of this study was to evaluate the consistency between the STS and WTW diameters, analyze the differences between the STS and WTW diameters and their effects on the vault, and analyze the related factors to provide a basis for the selection of the appropriate ICL size.
Methods
Compliance with Ethics Guidelines
This retrospective study adhered to the Declaration of Helsinki and was approved by the Ethical Committee Review Board of the Fudan University Eye and ENT Hospital (2016038).
Study Population
The inclusion criteria were as follows: reasonable desire for treatment, stable refraction (the increase in diopters [D] within 2 years before surgery was less than 0.50 D per year), and age between 20 and 40 years.
The exclusion criteria were as follows: complications occurred during surgery; failure to understand the risks of surgery or unrealistic expectations of surgical outcomes; corneal degeneration or endothelial cell density of < 2000 cells/mm2; ACD of < 2.8 mm; refractive media opacity that severely disturbed vision; history of autoimmune diseases such as systemic lupus erythematosus, rheumatoid arthritis, multiple sclerosis, or diabetes; and history of ocular diseases (uveitis, cataract, glaucoma, or retinal detachment) other than myopia and astigmatism.
The preoperative WTW and STS diameters, ACD, and 1-month postoperative vault were collected.
Implantable Collamer Lens
The EVO Visian ICL (Staar Surgical, Nidau, Switzerland) is a plate-haptic single-piece intraocular lens made of Collamer. It has a central convex-concave optical zone and incorporates a forward vault to minimize its contact with the crystalline lens. A 360-μm central hole is included to improve aqueous humor circulation, which eliminates the need for preoperative laser peripheral iridotomy. The EVO ICL provides myopic spherical correction from −0.50 to −18.00 D and cylindrical correction of up to −5.00 D. There are four sizes: 12.1 mm, 12.6 mm, 13.2 mm, and 13.7 mm. The size (length) of the implanted ICL was determined based on the WTW diameter and ACD of the patients. The selection of the type of ICL was similar to that used in the previous study by our team [8].
Surgical Procedure
All surgeries were performed by experienced surgeons (XW and XZ). The implantation of ICL and the surgical procedures were the same as those in our previous studies [8, 12].
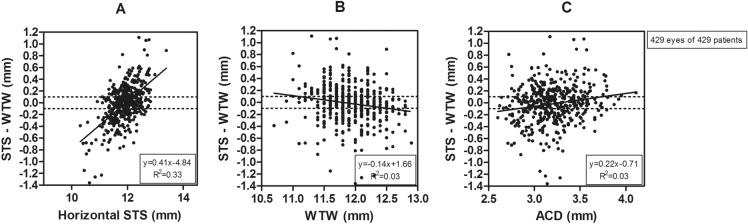
Measurement of the White-to-White Diameter
The WTW diameter was measured using an IOLMaster 500 PCI optical biometer. The IOLMaster is a noncontact three-dimensional anterior segment system. Without manipulation of the eyelid position, the WTW diameter was automatically measured horizontally. The IOLMaster measures the WTW diameter based on a digital image of the anterior segment that it acquires. The instrument digitally locates the limbus based on a sudden change in contrast from the bright sclera to the dark cornea (Fig. 1).
Fig. 1.
IOLMaster image with the distance of the white line marking the white-to-white (WTW) diameter
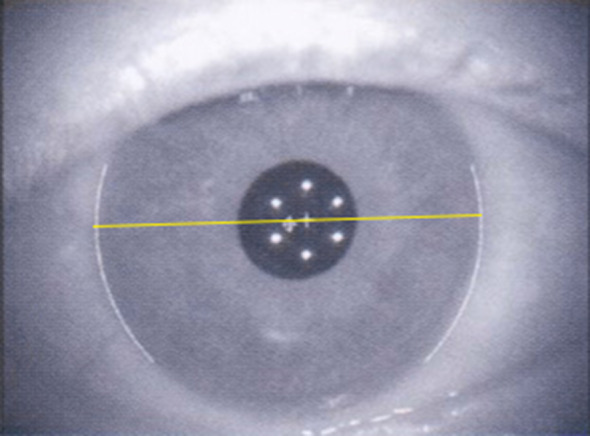
Measurement of the Sulcus-to-Sulcus Diameter
The patient, in a reclined position, was asked to fixate with the fellow eye on a ceiling target (approximate height 4 m) to maintain fixation and avoid accommodation; the pupils were left un-dilated. The STS diameters were measured using an ultrasound biomicroscopy measurement system (UBM, AVISO V:4.0.2, Quantel Medical, France) equipped with a 50-MHz transducer. The probe of the 50-MHz transducer enables an exploration width of 16.0 mm with an axial resolution of up to 35 mm and a lateral resolution of 60 mm in the anterior segment and a penetration of 9.0–11.0 mm. Cross-sectional images were obtained on the following two meridians: vertical (up-down, 90°) and horizontal (nasal-temporal 180°). The STS diameters were measured offline in the images with the widest pupil diameter (Fig. 2).
Fig. 2.
Aviso 50 MHz ultrasound biomicroscopy (UBM) image with the horizontal line marking the sulcus-to-sulcus (STS) diameter
Measurement of Vault
The measurement of the vault after ICL implantation was similar to that in the previous research by our team with corneal topography (Pentacam HR, type 70900; Oculus Optikgeräte GmbH, Wetzlar, Germany) [8].
Statistical Analysis
All statistical analyses were performed using SPSS version 20.0 (IBM Corp., Armonk, NY, USA), and the results were expressed as mean ± SD. Spearman and Pearson correlation analysis was performed to investigate the relationships between the anterior segment biometry variables. One-way analysis of variance was used to compare the results of the three groups. Statistical significance was set at P < 0.05.
Results
Patient Demographics
A total of 429 eyes of 429 patients (145 men and 284 women) aged 29.22 ± 8.06 years were analyzed. The baseline characteristics are presented in Table 1, with a summary based on refraction and anterior segment biometry. The mean SE ± standard deviation (SD) of these eyes was −13.09 ± 4.66 D. The mean sphere and cylinder refractive corrections were −12.24 ± 4.53 D and −1.71 ± 1.19 D, respectively.
Table 1.
Patient characteristics
| Parameter | Mean ± SD | Range |
|---|---|---|
| Age (years) | 29.66 ± 7.51 | 19–48 |
| Spherical equivalent refraction (D) | –13.09 ± 4.66 | –3.88 to –29.38 |
| Spherical refraction (D) | –12.24 ± 4.53 | –3.50 to –28.50 |
| Cylindrical refraction (D) | –1.71 ± 1.19 | 0.00 to –6.25 |
| WTW (mm) | 11.92 ± 0.38 | 10.70–12.90 |
| Horizontal STS (mm) | 11.90 ± 0.46 | 10.31–13.39 |
| Vertical STS (mm) | 12.46 ± 0.68 | 10.67–13.75 |
| Horizontal STS − WTW (mm) | –0.02 ± 0.33 | –1.36 to 1.11 |
| ACD (mm) | 3.20 ± 0.26 | 2.60–4.11 |
| ICL size (mm) | 13.04 ± 0.43 | 12.1–13.7 |
WTW horizontal white-to-white diameter, STS sulcus-to-sulcus distance, ACD anterior chamber depth, ICL implantable Collamer lens
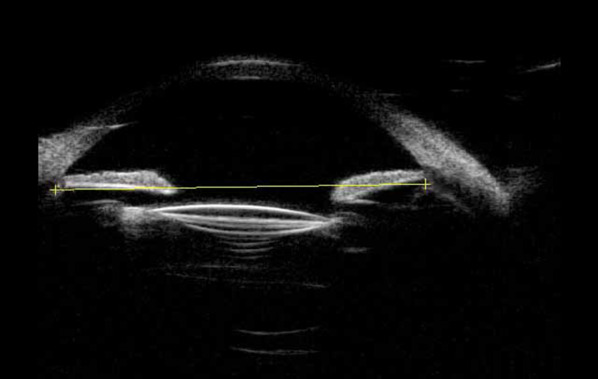
Sulcus-to-Sulcus versus White-to-White
The relationship between the horizontal WTW and STS diameters is demonstrated in Fig. 3. Both horizontal and vertical STS diameters were positively correlated with the WTW diameter (Pearson correlation coefficient; horizontal STS: r = 0.71, P < 0.001; vertical STS: r = 0.63, P < 0.001). The regression equations were as follows: y = 0.86x + 1.66 and y = 0.81x + 2.84. The best-fit line of the horizontal STS/WTW and the equivalence line intersected at the point of WTW = 11.86; the bias increased as the WTW diameter moved further from 11.86 mm.
Fig. 3.
Representation of the relationship between the WTW and STS diameters. STS sulcus-to-sulcus, WTW white-to-white
Effect of the Difference on the Vault
The average vault of the three groups was 514.01 ± 145.15 μm. The mean difference between the horizontal STS and WTW diameters (△STS–WTW) was −0.02 ± 0.33 (−1.36 to 1.11) mm. Based on the value of △STS–WTW, the eyes were divided into three groups: group A (146 eyes): △STS–WTW < −0.1, in which the WTW diameter was longer than the STS diameter, and the ICL may be large; group B (142 eyes): −0.1 ≤ △STS–WTW ≤ 0.1, where the WTW diameter was almost equal to the STS diameter, and the ICL may be moderate; and group C (141 eyes): △STS–WTW > 0.1, which means that the WTW diameter was longer than the STS diameter, and the ICL designed by WTW may be small. The vaults of group A, B, and C were 558.36 ± 163.58 (250–1100) μm, 513.10 ± 121.42 (190–850) μm, and 469.01 ± 133.23 (120–750) μm, respectively. There were significant differences between the three groups (P < 0.05). The eyes with ideal vaults of 250–750 μm were 89.04% in group A, 97.18% in group B, and 91.49% in group C. In group A, lower △STS–WTW values were associated with higher vaults (P < 0.05). In group C, greater △STS–WTW values were associated with lower vaults (P < 0.05).
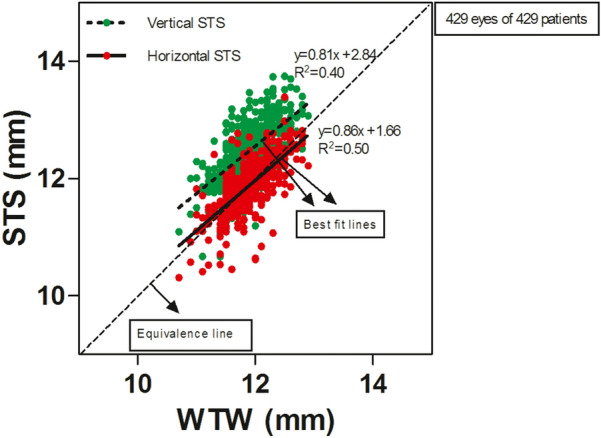
The Related Factors of △STS–WTW
The difference between the STS and WTW diameters was positively correlated with the horizontal STS diameter (r = 0.30, P < 0.001), negatively correlated with the WTW diameter (r = −0.17, P = 0.001), and positively correlated with ACD (r = 0.17, P < 0.001) (Fig. 4). The difference between the STS and WTW diameters was not correlated with other ocular parameters.
Fig. 4.
Correlations between the △STS–WTW values and horizontal STS diameter (A), WTW diameter (B), and anterior chamber depth (C). STS sulcus-to-sulcus, WTW white-to-white, ACD anterior chamber depth
The best line of fit of STS–WTW/horizontal STS and the △STS–WTW = −0.1 or 0.1 line intersected at the point of STS = 11.69 and 12.19, respectively. An increase in deviation of the STS diameter from 11.69 to 12.19 mm was associated with increased bias of △STS–WTW and a weaker correlation between STS and WTW. The best line of fit of STS–WTW/WTW and the △STS–WTW = −0.1 or 0.1 line intersected at the point of WTW = 11.08 and 12.51, respectively. Similarly, an increase in deviation of the WTW diameter from 11.08 to 12.51 mm was associated with increased bias of △STS–WTW and a weaker correlation between the STS and WTW diameters. The best line of fit of STS–WTW/ACD and the △STS–WTW = −0.1 or 0.1 line intersected at the point of ACD = 2.81 and 3.74, respectively. Lastly, an increase in deviation of ACD from 2.81 to 3.74 mm was also associated with increased bias of △STS–WTW and a weaker correlation between the STS and WTW diameters.
Discussion
Although the STS diameter is the deciding factor for choosing the size of the ICL, STS measurement has poor repeatability [13]. Thus, the WTW diameter has always been the gold standard for the selection of ICL size. However, the vault outcomes were sometimes unexpected. This is the first large-sample study on the effect of the difference between the WTW and STS diameters on vault and its related factors, and it provides clinical and practical value for the selection of ICL size.
In this study, we found that there was a correlation between the WTW and STS diameters, but the correlation was not that strong. The intersection point of the WTW and STS diameters was 11.86 mm. A greater deviation of the WTW diameter from 11.86 mm was associated with a greater difference between the WTW and STS diameters. Previous studies [13, 15] have also found that the correlation between the WTW and STS diameters is not strong. Studies [16, 17] have even found that the WTW and STS diameters are not correlated at all. Therefore, the effect of the difference between the WTW and STS diameters on the selection of the ICL size and vault is worthy of further discussion.
The results show that when △STS–WTW is < 0.1, the vault is slightly higher than the ideal one. This indicates that when the WTW diameter is greater than the STS diameter, the selection of ICL based on the WTW diameter may be too large, and a greater difference between the WTW and STS diameters is associated with a higher vault after the surgery. For −0.1 ≤ △STS–WTW ≤ 0.1, the vault is moderate, and 97.18% of the eyes had the ideal range of vault. This indicates that when the difference between the WTW and STS diameters is limited, the ICL model designed based on the WTW diameter is suitable. For △STS–WTW > 0.1, the vault is slightly lower than the ideal one, which indicates that when the WTW is smaller than the STS, the ICL model designed based on the WTW diameter may be small, and a greater difference between the WTW and STS diameters is associated with a lower vault. Therefore, when the deviation between the WTW and STS diameters is not high, the size of the ICL can be based on the WTW diameter in clinical practice. However, when the deviation between the WTW and STS diameters is high, selecting the size of the ICL based on the WTW diameter is not a suitable option. For these cases, we can refer to the STS diameter or select the size of the ICL based on the STS diameter. We will explore this further in our follow-up research.
The mechanism leading to a difference between the WTW and STS diameters deserves attention. The results showed that there was a correlation between the values of △STS–WTW and the preoperative WTW diameter, STS diameter, and ACD. An increase in the deviation of the WTW diameter from 11.08 to 12.51 mm, the STS diameter from 11.69 to 12.19 mm, and the ACD from 2.81 to 3.74 mm were associated with a decreased correlation between the WTW and STS diameters. The results of this study are consistent with previous findings [11, 13, 15]. Therefore, for cases with a WTW diameter or anterior chamber depth beyond a certain range, the possibility of a large difference between the WTW and STS increases. Furthermore, it is not suitable to design the ICL size based merely on the WTW diameter, and STS diameter should be taken into consideration as the main factor. For such patients, repeated STS measures can help to ensure repeatability.
The results also show that the vertical diameter of the ciliary sulcus is greater than the horizontal diameter, which is consistent with the findings of previous studies [18, 19]. This suggests that if the vault is slightly lower than the ideal one for the horizontal placement of the ICL, the ideal vault may be obtained by vertical or oblique axis placement of the ICL. Postoperative ICL rotation and the occurrence of complications related to low vault can be reduced with the help of a special design (vertical or oblique axis).
There were several limitations in this study. Firstly, the subjects were all Asian, whose horizontal corneal diameter is usually smaller than that of other ancestries [20]. Secondly, there was no control group to compare the design of the ICL models based on the STS diameter. Moreover, the results of ICL placement in the vertical or oblique axial position were not reported. These two limitations will be addressed in our future research. Thirdly, the repeatability and accuracy of STS measured by UBM were not evaluated. However, previous studies [21, 22] confirmed that high accuracy and good repeatability could be achieved by the full-scale 50-MHz UBM, and the UBM could measure the municipal sulcus diameter and be used for determining the ICL size directly. Repeated measurements by different professional and experienced testers were carried out for several patients, and the error of STS was about 0.03 mm. Therefore, the STS manually measured by UBM in this study was considered to be reliable.
Conclusions
In conclusion, the use of WTW-based prediction of the horizontal ciliary sulcus diameter is not ideal in some cases, as it may lead to poorly fit ICL sizes, increasing the risk of unsatisfactory intraocular lens vault and instability. The difference between the WTW and STS diameters was larger for the cases with an out-of-range WTW diameter or anterior chamber depth. Special attention should be paid to these patients. For cases with an out-of-range WTW diameter or anterior chamber depth, the difference between the WTW and STS diameters was larger, and WTW-based ICL selection may be associated with an undesirable vault after ICL implantation.
Acknowledgements
Funding
Funding for this study, including the journal’s rapid service fees, came from the following: (1) National Natural Science Foundation of China (Grant No. 81770955); (2) Joint Research Project of New Frontier Technology in Municipal Hospitals (Grant No. SHDC12018103); (3) Project of Shanghai Science and Technology (Grant No. 20410710100); (4) Major Clinical Research Project of Shanghai Shenkang Hospital Development Center (Grant No. SHDC2020CR1043B); (5) Project of Shanghai Xuhui District Science and Technology (Grant No. 2020–015); (6) Shanghai Science and Technology Commission (Grant No. 19140900700); (7) Shanghai Sailing Program (Grant No. 20YF1405000); and (8) National Natural Science Foundation of China for Young Scholars (Grant No. 82000929).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
The authors were involved in the conception or design of the work, the acquisition, analysis or interpretation of data for the work (Xun Chen, Tian Han, Wuxiao Zhao, Xuanqi Wang, Yilin Xu, Mingrui Cheng, Xianying Wang, Xingtao Zhou); drafting the work or revising it critically for important intellectual content (Xun Chen, Tian Han); final approval of the version to be published (Xun Chen, Tian Han, Wuxiao Zhao, Xuanqi Wang, Yilin Xu, Mingrui Cheng, Xianying Wang, Xingtao Zhou); agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved (Xun Chen, Tian Han, Wuxiao Zhao, Xuanqi Wang, Yilin Xu, Mingrui Cheng, Xianying Wang, Xingtao Zhou).
Disclosures
Xun Chen, Tian Han, Wuxiao Zhao, Xuanqi Wang, Yilin Xu, Mingrui Cheng, Xianying Wang, and Xingtao Zhou all confirm that they have no conflicts of interest to declare.
Compliance with Ethics Guidelines
Ethics Committee of the Fudan University Eye and ENT Hospital (2016038).
Data Availability
Data and materials are available upon request from the corresponding author at doctxiaoyingwang@163.com or doctzhouxingtao@163.com.
Footnotes
Xun Chen and Tian Han contributed equally and are considered co-first authors.
Contributor Information
Xiaoying Wang, Email: doctxiaoyingwang@163.com.
Xingtao Zhou, Email: doctzhouxingtao@163.com.
References
- 1.Bredow L, Biermann J, Tomalla M, Schilgen G, Grossmann W, Reinhard T. Pilot study of a new posterior chamber phakic intraocular lens (epi.lens) for high myopia. J Refract Surg. 2011;27:858–862. doi: 10.3928/1081597X-20111017-01. [DOI] [PubMed] [Google Scholar]
- 2.Gasser L, Biermann J, Reinhard T. New posterior chamber phakic intraocular lens for high myopia: three-year results. J Cataract Refract Surg. 2015;41:1610–1615. doi: 10.1016/j.jcrs.2014.11.052. [DOI] [PubMed] [Google Scholar]
- 3.Siedlecki J, Schmelter V, Mayer WJ, Schworm B, Priglinger SG, Dirisamer M, Luft N. SMILE versus implantable collamer lens implantation for high myopia: a matched comparative study. J Refract Surg. 2020;36:150–159. doi: 10.3928/1081597X-20200210-02. [DOI] [PubMed] [Google Scholar]
- 4.Sanders D, Vukich JA. Comparison of implantable collamer lens (ICL) and laser-assisted in situ keratomileusis (LASIK) for low myopia. Cornea. 2006;25:1139–1146. doi: 10.1097/ICO.0b013e31802cbf3c. [DOI] [PubMed] [Google Scholar]
- 5.Sanders DR, Sanders ML. Comparison of the toric implantable collamer lens and custom ablation LASIK for myopic astigmatism. J Refract Surg. 2008;24:773–778. doi: 10.3928/1081597X-20081001-02. [DOI] [PubMed] [Google Scholar]
- 6.Tsiklis NS, Kymionis GD, Karp CL, Naoumidi T, Pallikaris AI. Nine-year follow-up of a posterior chamber phakic IOL in one eye and LASIK in the fellow eye of the same patient. J Refract Surg. 2007;23:935–937. doi: 10.3928/1081-597X-20071101-12. [DOI] [PubMed] [Google Scholar]
- 7.Kamiya K, Shimizu K, Komatsu M. Factors affecting vaulting after implantable collamer lens implantation. J Refract Surg. 2009;25:259–264. doi: 10.3928/1081597X-20090917-10. [DOI] [PubMed] [Google Scholar]
- 8.Chen X, Miao H, Naidu RK, Wang X, Zhou X. Comparison of early changes in and factors affecting vault following posterior chamber phakic Implantable Collamer Lens implantation without and with a central hole (ICL V4 and ICL V4c) BMC Ophthalmol. 2016;16:161. doi: 10.1186/s12886-016-0336-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidinger G, Lackner B, Pieh S, Skorpik C. Long-term changes in posterior chamber phakic intraocular collamer lens vaulting in myopic patients. Ophthalmology. 2010;117:1506–1511. doi: 10.1016/j.ophtha.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 10.Trancon AS, Manito SC, Sierra OT, Baptista AM, Serra PM. Determining vault size in implantable collamer lenses: preoperative anatomy and lens parameters. J Cataract Refract Surg. 2020;46:728–736. doi: 10.1097/j.jcrs.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 11.Lee DH, Choi SH, Chung ES, Chung TY. Correlation between preoperative biometry and posterior chamber phakic Visian Implantable Collamer Lens vaulting. Ophthalmology. 2012;119:272–277. doi: 10.1016/j.ophtha.2011.07.047. [DOI] [PubMed] [Google Scholar]
- 12.Zhang X, Chen X, Wang X, Yuan F, Zhou X. Analysis of intraocular positions of posterior implantable collamer lens by full-scale ultrasound biomicroscopy. BMC Ophthalmol. 2018;18:114. doi: 10.1186/s12886-018-0783-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guber I, Bergin C, Perritaz S, Majo F. Correcting interdevice bias of horizontal White-to-White and Sulcus-to-Sulcus measures used for implantable collamer lens sizing. Am J Ophthalmol. 2016;161:116–125. doi: 10.1016/j.ajo.2015.09.037. [DOI] [PubMed] [Google Scholar]
- 14.Montes-Mico R, Ruiz-Mesa R, Rodriguez-Prats JL, Tana-Rivero P. Posterior-chamber phakic implantable collamer lenses with a central port: A review. Acta Ophthalmol. 2021;99:e288–e301. doi: 10.1111/aos.14599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kawamorita T, Uozato H, Kamiya K, Shimizu K. Relationship between ciliary sulcus diameter and anterior chamber diameter and corneal diameter. J Cataract Refract Surg. 2010;36:617–624. doi: 10.1016/j.jcrs.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 16.Werner L, Izak AM, Pandey SK, Apple DJ, Trivedi RH, Schmidbauer JM. Correlation between different measurements within the eye relative to phakic intraocular lens implantation. J Cataract Refract Surg. 2004;30:1982–1988. doi: 10.1016/j.jcrs.2003.10.041. [DOI] [PubMed] [Google Scholar]
- 17.Oh J, Shin HH, Kim JH, Kim HM, Song JS. Direct measurement of the ciliary sulcus diameter by 35-megahertz ultrasound biomicroscopy. Ophthalmology. 2007;114:1685–1688. doi: 10.1016/j.ophtha.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 18.Reinstein DZ, Archer TJ, Silverman RH, Rondeau MJ, Coleman DJ. Correlation of anterior chamber angle and ciliary sulcus diameters with white-to-white corneal diameter in high myopes using artemis VHF digital ultrasound. J Refract Surg. 2009;25:185–194. doi: 10.3928/1081597X-20090813-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim KH, Shin HH, Kim HM, Song JS. Correlation between ciliary sulcus diameter measured by 35 MHz ultrasound biomicroscopy and other ocular measurements. J Cataract Refract Surg. 2008;34:632–637. doi: 10.1016/j.jcrs.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 20.Hickson-Curran S, Brennan NA, Igarashi Y, Young G. Comparative evaluation of Asian and white ocular topography. Optom Vis Sci. 2014;91:1396–1405. doi: 10.1097/OPX.0000000000000413. [DOI] [PubMed] [Google Scholar]
- 21.Li DJ, Wang NL, Chen S, Li SN, Mu DP, Wang T. Accuracy and repeatability of direct ciliary sulcus diameter measurements by full-scale 50-megahertz ultrasound biomicroscopy. Chin Med J (Engl) 2009;122:955–959. [PubMed] [Google Scholar]
- 22.Qureshi A, Chen H, Saeedi O, Kaleem MA, Stoleru G, Margo J, Kalarn S, Alexander JL. Anterior segment ultrasound biomicroscopy image analysis using ImageJ software: Intra-observer repeatability and inter-observer agreement. Int Ophthalmol. 2019;39:829–837. doi: 10.1007/s10792-018-0882-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and materials are available upon request from the corresponding author at doctxiaoyingwang@163.com or doctzhouxingtao@163.com.