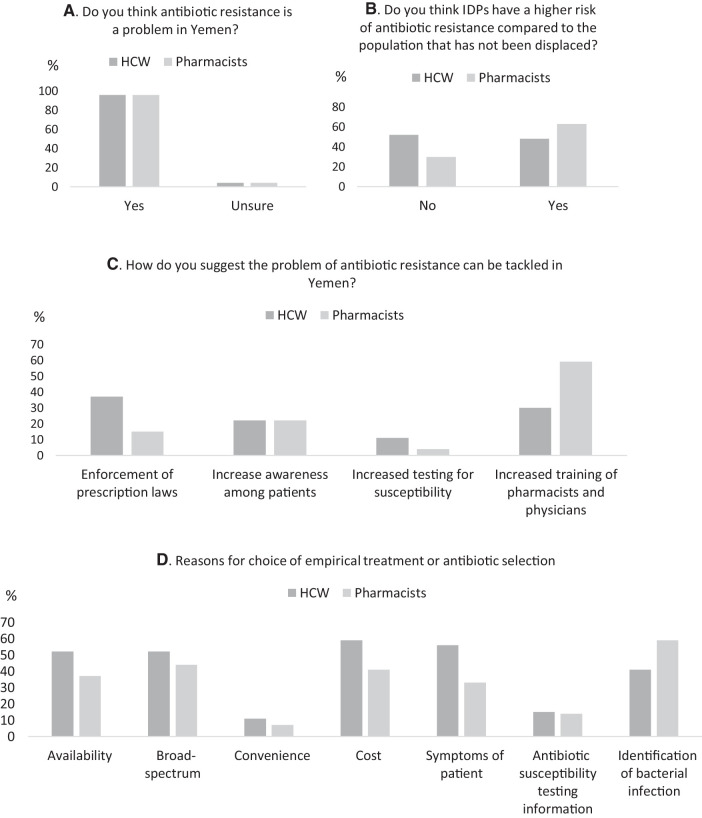
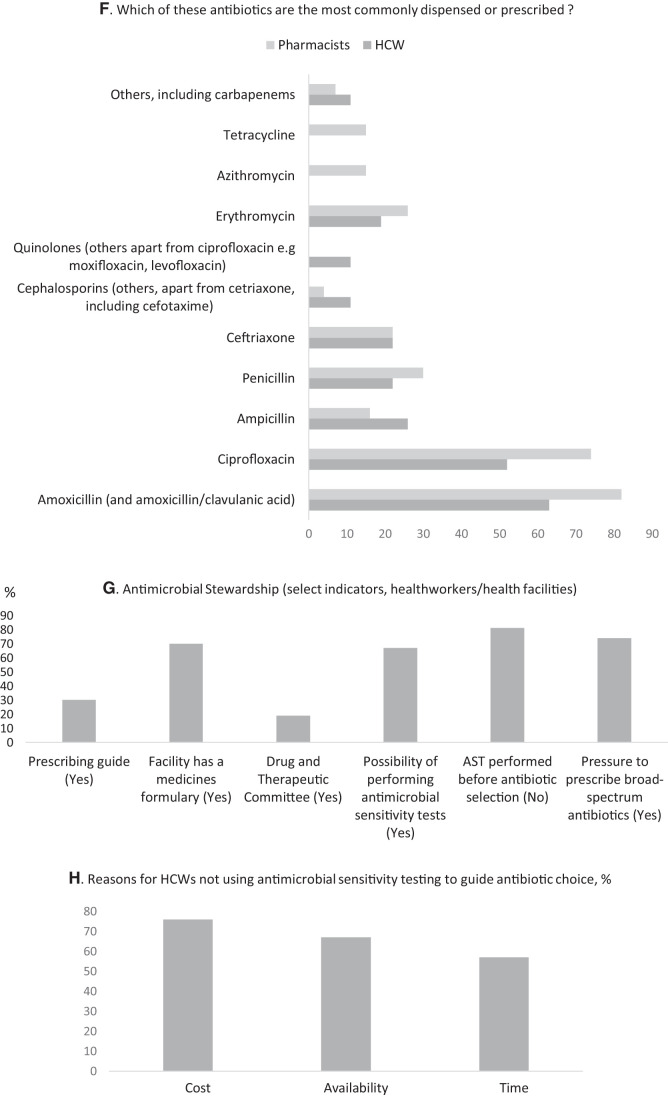
Figure 1.
Summary of select results from a survey assessing antimicrobial resistance, use, and stewardship in healthcare workers (HCW) and pharmacists in Yemen. (A, B, and C) Antimicrobial resistance (AMR): The majority of respondents (96%) thought AMR to be a problem in Yemen (A) but were more split in terms of if IDPs had the greater risk (B). Among solution options to tackling AMR, both respondents ranked the use of increased antimicrobial sensitivity testing the lowest and ranked increased training of pharmacists and physicians (HCW) the highest. (D, E, and F) Antimicrobial use: There were several overlapping reasons for choice of empirical treatment or empirical antibiotic selection both in prescribing physicians and dispensing pharmacists with cost (price patient can afford), signs and symptoms (including “identification of bacterial infection”) of patient and availability with a preference for broad-spectrum antibiotics. In terms of antibacterial agents, amoxicillin (including amoxicillin/clavulanic acid) was the most commonly prescribed or dispensed followed by ciprofloxacin. (G and H) Antimicrobial stewardship: Among select criteria, physicians reported to be under pressure to prescribe broad-spectrum antibiotics, and even where there was the possibility to perform antimicrobial sensitivity tests, these were not used to guide prescribing in the majority of cases. The reason for this was largely cost (H).