FIGURE 4: Schematic overview of host innate responses to bacterial corneal pathogens, which involve the loss of corneal immune privilege.
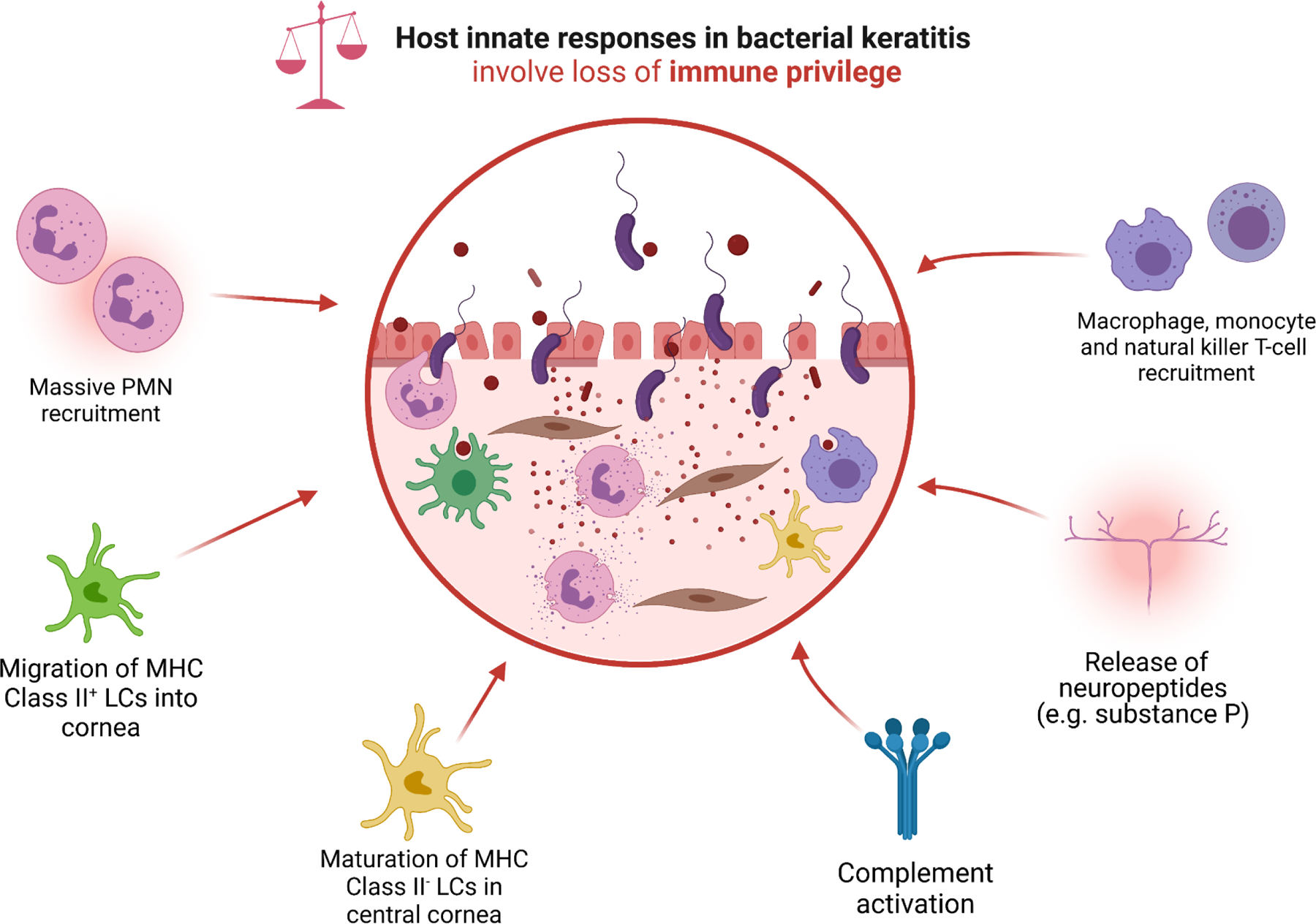
Pattern recognition receptors (PRRs), predominantly toll-like receptors (TLRs), ligate with pathogen-associated molecular patterns (PAMPs) including bacterial lipoteichoic acid and lipopolysaccharides. PRR-binding leads to the upregulation of pro-inflammatory transcription factors such as NF-κB, with subsequent cellular release of pro-inflammatory cytokines (TNF-α, IL-1, IL-6, IL-8, IL12, IL-18, IFNs and MIF), chemokines (CXCL-1, CXCL-2, CXCL-5, CCL-4, CCL-5, IL-18, MCP-1), endothelial adhesion molecules (ICAM-1, MAC-1, PECAM-1, VCAM-1, E-selectin, and P-selectin). Several cell types (e.g., corneal epithelial cells) also inappropriately upregulate the production and release of digestive MMPs, including MMP-1, MMP-2, MMP-3, and MMP-9. This pro-inflammatory storm of cytokines induces massive neutrophil recruitment; migration of MHC Class II+ LCs from the corneal limbus, conjunctiva, and surrounding vascular beds into the stroma; maturation of resident stromal MHC Class II− LCs; recruitment of macrophages and monocytes; activation of complement; and release of neuropeptides such as substance P. The activation of LCs serves as a bridge to the adaptive immune response, which is characterized by recruitment of Th1-predominant helper-T cells that preside over the persistence of PMNs, and are associated with severe disease phenotypes (e.g., corneal perforation).
