Abstract
Background
This review provides an estimate of the global prevalence of depression and anxiety symptoms among doctors, based on analysis of evidence from the first year of the COVID-19 pandemic.
Methods
A systematic review was conducted to identify suitable studies. Final searches were conducted on 3rd March 2021. Papers were initially screened by title and abstract, based on pre-agreed inclusion criteria, followed by full-text review of eligible studies. Risk of bias was assessed using the Joanna Briggs Checklist for Prevalence Studies. Data from studies rated as low or medium risk of bias were pooled using a random-effects meta-analysis. Sensitivity and subgroup analyses were conducted to explore heterogeneity.
Results
Fifty-five studies were included after full-text review. Of these, thirty studies were assessed as low or medium risk of bias and were included in primary analyses. These comprised twenty-six studies of depression (31,447 participants) and thirty studies of anxiety (33,281 participants). Pooled prevalence of depression and anxiety was 20.5% (95% CI 16.0%-25.3%) and 25.8% (95% CI 20.4%-31.5%) respectively.
Interpretation
Evidence from the first year of the pandemic suggests that a significant proportion of doctors are experiencing high levels of symptoms of depression and anxiety, although not conclusively more so than pre-pandemic levels. Differences in study methodology and variation in job demands may account for some of the observed heterogeneity.
Limitations
Findings must be interpreted with caution due to the high heterogeneity and moderate risk of bias evident in the majority of included studies.
Keywords: Doctors, Physicians, Covid-19, Coronavirus, depression, anxiety
1. Introduction
On the 30th January 2020 the world health organisation (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak a Public Health Emergency of International Concern, its highest level of alarm. An unparalleled global response followed, with local and national ‘lockdowns’, quarantines, travel restrictions, and physical distancing measures introduced in attempts to curb transmission rates. At the time of writing, there have been over 114 million confirmed cases and more than 2.5 million reported COVID-associated deaths (WHO, 2021).
In response to the unprecedented pressure on global health systems, there has been enhanced focus on the mental wellbeing of healthcare staff. In April 2020, The Lancet published a position paper outlining their suggested research priorities for the pandemic:
“The immediate research priorities are to monitor and report rates of anxiety, depression, self-harm, suicide, and other mental health issues both to understand mechanisms and crucially to inform interventions. This should be adopted across the general population and vulnerable groups, including front-line workers.”
(Holmes et al., 2020, p5)
Poor mental health and wellbeing among healthcare staff has organisational implications for patient safety, experience, and satisfaction (Wallace et al., 2009), in addition to financial costs, impact on productivity, and the direct effects on the individual (Royal College of Psychiatrists, 2015). High pressured working environments, heavy workload, long hours, limited resources, organisational restructuring, and a culture of blame and fear have all been implicated as contributory factors (Wilkinson, 2015; Lemaire and Wallace, 2017); all factors that have become increasingly salient within the context of the current global crisis.
The Job Demand-Resources (JD-R) model of occupational stress (Demerouti et al., 2001) offers a framework to understand these problems. The model hypothesises that as job demands increase so too does emotional strain, which negatively affects performance. Whereas greater access to job resources is associated with enhanced engagement and performance. Job demands are conceptualised as the physical, psychological, social, and organisational features of a job that require sustained physical and/or psychological effort. Examples of job demands are high workload or emotionally demanding interactions with patients. Job resources are defined as the physical, psychological, social, or organizational aspects of a job that facilitate achievement of work-based goals, reduce job demands, and stimulate personal growth, learning, and development. Examples of job resources are performance feedback, autonomy, and skill variety. The theory suggests that job demands are associated with health-impairments (e.g., poor mental or physical health), whereas job resources are associated with engagement and motivational processes (Bakker and Demerouti, 2017). The current pandemic can be considered a universal job demand on health care systems across the world. However, there will also be additional localised variability in job demands and resources. For example, insufficient staffing levels and underfunded services may create additional strain for healthcare workers.
Medics form an essential part of the global frontline pandemic response. Studies conducted outside of global crises have highlighted that medical students and doctors are already at increased risk of psychological distress, depression, anxiety, burnout, and suicidality, compared with the general population (De Sio et al., 2020; Dong et al., 2020; Tian-Ci Quek, 2019; Hayes et al., 2017; Dai et al., 2015; Dyrbye et al., 2006). As a result, there have been calls to improve the conceptual definition and measurement of wellbeing in medics (Brady et al., 2018; Wallace et al., 2009).
Studies conducted during the 2003 outbreak of severe acute respiratory syndrome (SARS) indicated significant psychological distress in 18% to 57% of health care workers (Tam et al., 2004; Chan and Huak, 2004; Phua et al., 2005; Nickell et al., 2004; Maunder et al., 2004). A study conducted one to two years post-SARS outbreak found high levels of burnout, psychological distress, and posttraumatic stress in healthcare workers (Maunder et al., 2006). However, a similar study by Lancee et al. (2008) found incidence of new episodes of psychiatric disorders in community populations were similar to, or higher than, those observed in health care workers two years post-outbreak.
Although a number of studies have focused on the prevalence of mental health outcomes in doctors during the current COVID-19 pandemic, to the author's knowledge, there have been no systematic reviews conducted to analyze and synthesize data relating exclusively to doctors. Some meta-analyses of healthcare workers of multiple professions have included doctors (Santabárbara et al., 2021; Pappa et al., 2020; Salari et al., 2020; Luo et al., 2020), and sub-group analyses provide some evidence of high levels of psychological distress among medics. However, outcomes from these analyses are limited by review design (e.g., rapid reviews), and underpowered sub-group meta-analyses for doctors. In addition, given the rate of publications during the pandemic, an up-to-date review is needed.
The current review will focus on the prevalence of symptoms of depression and anxiety during the COVID-19 pandemic. Previous meta-analyses have estimated the global prevalence of major depressive disorder and anxiety disorders to be 4.7% (4.4–5.0%) (Ferrari et al., 2013) and 7.3% (4.8–10.9%) (Baxter et al., 2013) respectively. The core features of depression are persistent depressed mood and anhedonia; other symptoms included psychomotor agitation or retardation, appetite changes, sleep problems, fatigue, feelings of low self-worth, poor concentration, and suicidal ideation (American Psychiatric Association 2013) Anxiety is characterized by psychological and somatic symptoms, including autonomic arousal (e.g., palpitations, sweating, trembling, dry mouth, difficulty breathing, chest pain, nausea), restlessness, fatigue, difficulty concentrating, irritability, and sleep problems (American Psychiatric Association 2013). Depression and anxiety are associated with impairments in cognitive functioning, including poorer performance on tests of memory, attention, executive function and motor function (Rock et al., 2014; Hallion et al., 2017; Moran, 2016; Eysenck et al., 2007; Runswick et al., 2018; Wilson, 2012). These cognitive, physiological, and behavioural consequences may be of particular concern among medical doctors, given the potential implications for professional competence and patient safety, as well as personal wellbeing.
The aim of this systematic review and meta-analysis is to analyze the evidence emerging from the first year of the COVID-19 pandemic to answer the following research questions:
-
•
What is the global prevalence of depression and anxiety symptoms among doctors during the COVID-19 pandemic?
-
•
What factors might explain differences in the prevalence of depression and anxiety symptoms among doctors during the COVID-19 pandemic?
2. Methods
This systematic review and meta-analysis was conducted in accordance with PRISMA (Page et al., 2021) and MOOSE (Meta-analyses of Observational Studies in Epidemiology) guidelines (Stroup et al., 2000). The review protocol was registered with PROSPERO and is available online (CRD42021228667).
2.1. Eligibility criteria
The CoCoPop framework (Condition, Context, Population), for prevalence and incidence reviews, was used to develop the following inclusion criteria: (i) assessment of depression and/ or general anxiety symptoms using a standardised and validated measure; (ii) conducted during the COVID-19 pandemic; (iii) practicing medical doctors working in any speciality, across the world. Studies were excluded studies based on the following criteria: (i) studies conducted outside of the pandemic timeframe; (ii) studies using non-standardised or unvalidated measures; (iii) studies that do not report prevalence for the target population or do not provide sufficient information to calculate prevalence; (iv) studies that have not separated professions in the data; (v) studies relating exclusively to medical students, non-practicing doctors, or non-medical doctors; (vi) pre-prints, or studies not published in a peer reviewed journal; (vii) studies with a sample size <139 (calculated according to minimum expected prevalence from previous literature (Vaughan and Morrow, 1989)).; (viii) qualitative studies; (ix) articles inaccessible for full review or not published in English; (x) studies not reporting original research (e.g., literature review, article, commentary); (xi) studies focussing on mental health outcomes other than depression and/ or general anxiety (e.g., stress, burnout, specific anxiety disorders).
2.2. Search strategy
A search strategy was developed following consultation with an expert librarian. Search terms were selected to identify records reporting on prevalence data for depression and anxiety in doctors during the COVID-19 pandemic. Full text searches were conducted using the following key search terms: (covid OR covid-19 OR “sars cov 2″ OR “sarscov2" OR “corona virus") AND (doctor* OR physician* OR medic OR medics) AND (anxiety OR “anxiety symptoms” OR “anxiety disorder” OR anxious OR “generali?ed anxiety” OR panic OR worry OR depress* OR “mental health” OR “mental illness” OR “mental disorder*”). Four electronic databases (PubMed, CINAHL, Embase, PsychInfo) and one preprint database (MedRxiv) were searched. Final searches were conducted on 3rd March 2021. Search strategies were adapted for each database, where necessary. No restrictions were applied. An example of the search terms used is included in Supplementary Information 1 (SI1). Identified records were extracted to Zotero and then uploaded to (Covidence systematic review software 2021).
2.3. Selection process
Two independent reviewers (G.J. and L.F.) screened titles and abstracts, followed by all eligible full text papers, based on the pre-agreed inclusion criteria. Inter-rater reliability was substantial (K = 0.66/ 0.68). Two research supervisors (L.W. and V.S.) were available to resolve any disagreements.
2.4. Data extraction
Data extraction was conducted independently by G.J. and a third reviewer (J.L.), and cross-checked for reliability. Where essential data was missing, the corresponding authors were contacted to request information. The following data items were extracted: author, publication year, study design, recruitment method, data collection timeframe, geographical location, measures used, cut-off and severity thresholds. The following data were extracted for the target population only (i.e., doctors): sample size, sex, age, number of positive cases of depression and anxiety, response rate. In cases where prevalence information was missing, relevant calculations were made, where possible.
The primary outcome was the total number of positive cases of depression and/ or anxiety among doctors during the pandemic, determined by the number of participants scoring above a pre-defined threshold on a validated depression or anxiety measure. Frequency data were collected for total sample (N), anxiety and/or depression cases (n), and resulting proportions with 95% confidence intervals (CI).
2.5. Study risk of bias assessment
Risk of bias was independently assessed by G.J. and J.L. for all included studies using the Joanna Briggs Inventory (JBI) Checklist for Prevalence Studies tool (Munn et al., 2015). The tool was developed for the purpose of increasing consistency in systematic reviews of prevalence data and has been recommended as the most appropriate tool for studies of this kind (Migliavaca et al., 2020). Study risk of bias was evaluated based on the following nine criteria: 1) Was the sample frame appropriate to address the target population? 2) Were study participants recruited in an appropriate way? 3) Was the sample size adequate? 4) Were the study subjects and setting described in detail? 5) Was data analysis conducted with sufficient coverage of the identified sample? 6) Were valid methods used for the identification of the condition? 7) Was the condition measured in a standard, reliable way for all participants? 8) Was there appropriate statistical analysis? 9) Was the response rate adequate, and if not, was the low response rate managed appropriately? Within the existing literature (Islam et al., 2020; Sarria-Santamera et al., 2021), level of bias is assessed by calculating the total number of criteria with a yes response and converting this score into a percentage (n/9). Studies scoring <50% are considered high risk of bias, 50–69% medium risk of bias, and ≥70% low risk of bias. The quality assessment tool was first piloted on a small number of studies. L.W. and V.S. were available for consultation and to resolve any disagreements.
2.6. Data analysis
Studies assessed as high risk of bias were excluded from the primary analysis. Following consultation with expert statisticians, a meta-analysis for proportional data was conducted using the Metaprop (Nyaga et al., 2014) command of the software package STATA version 16.1 (StataCorp, 2019). To address potential weighting issues that can occur when including studies with proportions close to one or zero, which can disproportionately skew the outcome of meta-analysis, proportions were transformed using the Freeman-Tukey double arcsine method (Freeman & Tukey, 1950), and back-transformed for ease of interpretation (Barendregt et al., 2013). A DerSimonian & Laird (1986) random effects model was used to extract pooled prevalence, given the assumed differences in regional demographics and study design. The I2 statistic was used to assess the statistical heterogeneity (Higgins et al., 2003). I2 values < 50% are considered low, 50–75% moderate, and >75% high. Subgroup analyses were conducted to explore sources of heterogeneity, as expected in meta-analyses of cross-sectional studies.
2.7. Sensitivity and subgroup analysis
Sensitivity analysis was conducted to explore the impact of individual studies (leave one out and cumulative analyses), and the impact of study quality and design (risk of bias, measure, severity threshold, and survey timeframe). Survey timeframe was split into first three months of the pandemic (January to March 2020), and April 2020 onwards. In line with the JD-R model, subgroup analysis was conducted to explore the potential for variability in job demands and resources to explain heterogeneity of outcomes during the pandemic. gross domestic product (GDP) per capita and doctors per 10,000 population were used as potential indicators of job demands and resources for each study. GDP per capita was split into three groups <$10,000 per capita, $10–15,000 per capita, and >$25,000 per capita. Doctors per 10,000 population was split into four groups <15.5, 15.5–19, 20–29, and >30. Geographical region was also explored as a potential source of heterogeneity, with studies grouped by continent; two studies were omitted from this sub-group analysis due to their global coverage. Sub-group analysis was only conducted for categories with a minimum of four studies. Reported outcomes are proportion (p), confidence interval (CI) and percentage prevalence (p × 100%). All statistical analyses were two-tailed and p=<0.05 was considered statistically significant.
2.8. Publication bias
Publication bias was assessed via visual inspection of funnel plots (SI3 and SI4) and Egger's test (Egger et al., 1997), with p = <0.05 indicating publication bias.
2.9. Certainty assessment
The grading of recommendations assessment, development, and evaluation (GRADE) system was used to assess the quality of the overall body of evidence and the level of confidence in the conclusions drawn (Guyatt et al., 2008). GRADE assessment considers factors over and above individual study risk of bias, such as imprecision, inconsistency, indirectness, study limitations and publication bias. Overall quality of evidence may be rated as high, moderate, low, or very low. All observational research begins as low quality and can be (less commonly) upgraded or (more commonly) downgraded, based on the five criteria outlined above (Balshem et al., 2011).
3. Results
3.1. Study selection
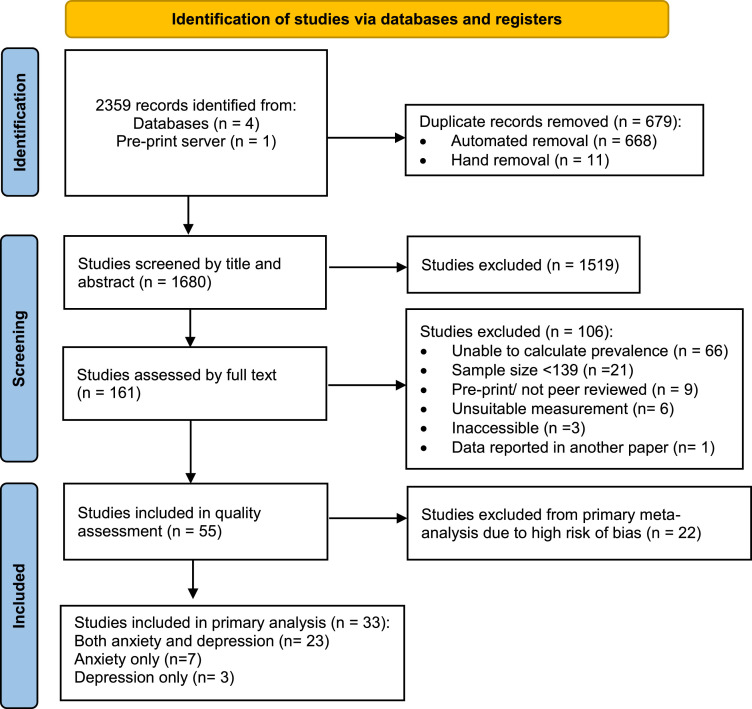
A total of 2359 records were identified following systematic review of four databases and one pre-print server. After removal of duplicates, 1680 records were screened by title and abstract. Full text review was conducted on 161 papers, of which a further 106 studies were excluded. Fifty-five studies (see SI2 for references) were included in the quality assessment process. A further 22 studies were excluded from the primary analysis due to high risk of bias, leaving 33 studies assessed as medium or low risk of bias. Twenty-three studies reported data for depression and anxiety, seven reported data exclusively for anxiety, and three reported data exclusively for depression. Study characteristics and prevalence data for high risk of bias studies are presented in Supplementary Tables 1 and 2 (ST1 and ST2). A PRISMA diagram detailing the flow of information is presented in Fig. 1
Fig. 1.
Prisma diagram presenting flow of information.
3.2. Risk of bias in studies
Risk of bias ratings for all 55 studies, assessed using the JBI Checklist for Prevalence Studies tool, are presented in ST3. Five studies were assessed as low, 28 as medium, and 22 as high risk of bias. Most studies used appropriate methods to identify and measure the condition(s) and reported appropriate statistical analysis. Setting and characteristics were also largely well described, although a small number of studies reporting on a wide range of health care workers were downgraded on this item, due to the lack of sufficient detail pertaining specifically to the target population of interest for this review (i.e., doctors). The predominant use of non-probability sampling methods reduced scores for many studies. This methodology typically indicates the absence of a sampling frame and random sampling approach, an inability to calculate a response rate, and introduces coverage bias. Some studies lost additional points due to inadequate reporting of data (e.g., absence of numerator and/or denominator), and some did not report sample size calculation, or provide sufficient information to calculate retrospectively.
3.3. Study characteristics
The sample size of the studies ranged from 149 to 10,178. All studies employed a cross-sectional design. Full study characteristics are summarised in ST4.
3.3.1. Characteristics of studies assessing depression
A total of 31,447 participants from 26 studies were included; ten studies were based in Asia, seven in Europe, four in North America, two in South America, two in Africa, and one multi-national. Participants’ mean (SD) age ranged from 28.0 (3) to 45.2 (13.3). The proportion of female participants ranged from 3.4% to 80.1%. The median number of participants per study was 467.5. Male vs female split was 45.9% vs 54.0% respectively (NB. sex data not reported for some studies).
3.3.2. Characteristics of studies assessing anxiety
A total of 33,281 participants from 30 studies were included. Ten studies were based in Asia, nine in Europe, five in North America, three in South America, two in Africa, and two were multi-national. The mean (SD) age of sample size ranged 28.0 (3) to 52.0 (11). The proportion of female participants ranged from 8.3% to 80.1%. The median number of participants per study was 502.5. Male vs female split was 46.6% vs 53.8%.
3.4. Measures
Seventeen studies used the Generalised Anxiety Disorder Scale-7 Item (GAD-7; Spitzer et al., 2006), thirteen used the Patient Health Questionnaire- 9 Item (PHQ-9; Kroenke et al., 2001), seven used the Hospital Anxiety and Depression Scale (HADS; Zigmond and Snaith, 1983), three used the Depression Anxiety Stress Scale-21 item (DASS-21, short version of the DASS; Lovibond and Lovibond, 1995), three used the Patient Health Questionnaire- 2 Item (PHQ-2; Löwe et al., 2005), one used the Generalised Anxiety Disorder Scale-2 Item (GAD-2; Kroenke et al., 2007) one used the Beck Anxiety Inventory (BAI; Beck et al., 1988), and one used the Patient-Reported Outcomes Measurement Information System– Anxiety (PROMIS; Cella et al., 2010).
3.5. Results of individual studies
Point prevalence of depression ranged from 6.1% (95% CI 5.5–6.8%) (Li et al., 2020)to 73.4% (95% CI 65.9–79.7%) (Elhadi et al., 2020). Point prevalence of anxiety ranged from 5.9% (95% CI 4.1–8.3%) (Skoda et al., 2020)to 74.2% (95% CI 70.3–77.8%) (Jain et al., 2020), although only two out of the 26 depression studies and two out of the 30 anxiety studies reported prevalence of <10%. Point prevalence and confidence intervals for all individual studies are presented in ST5.
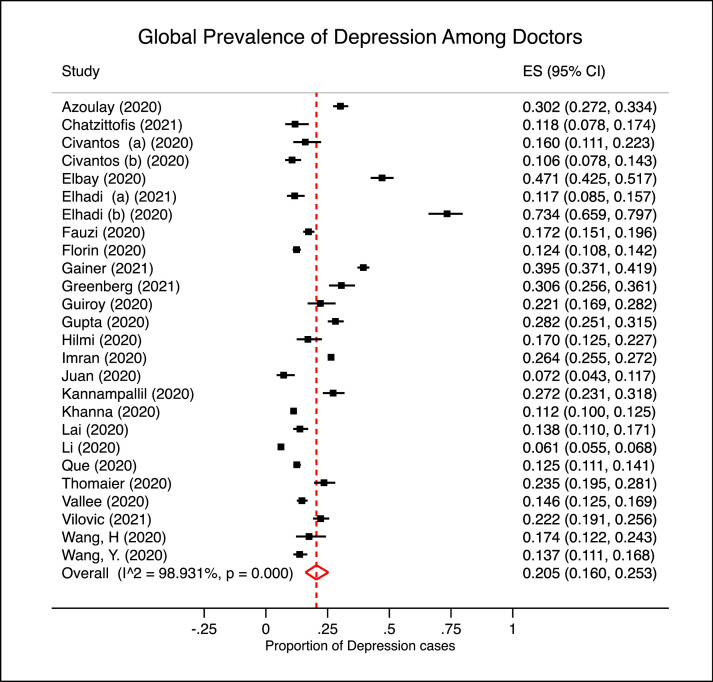
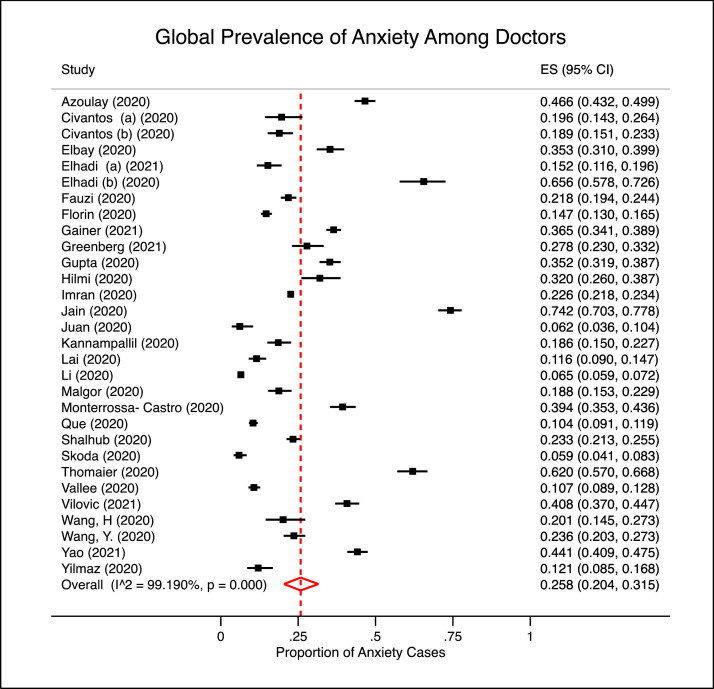
3.6. Results of synthesis
The pooled prevalence of depression for the 26 included studies was 20.5% (95% CI 16.0–25.3%), with a high degree of heterogeneity (I2 = 98.931%), as presented in Fig 2 . The pooled prevalence of anxiety for the 30 included studies was 25.8% (95% CI 20.4–31.5%), with a similarly high degree of heterogeneity (I2 = 99.190%), presented in Fig. 3
Fig. 2.
Forest plot showing the global prevalence of depression symptoms among doctors.
Fig. 3.
Forest plot showing the global prevalence of anxiety symptoms among doctors.
3.7. Sensitivity analysis
3.7.1. Sensitivity analysis for studies of depression
One study affected the pooled prevalence of depression by ≥1%. The study in question (Elhadi et al., 2020) changed pooled prevalence by 1.7%. After running the analysis without this study, pooled prevalence was 18.8% (95% CI 14.6–23.3%). Cumulative analysis revealed heterogeneity only reached acceptability for a subset of thirteen studies (Chatzittofis et al., 2021, Civantos et al., 2020a, Civantos et al., 2020b, Fauzi et al., 2020, Florin et al., 2020, Hilmi et al., 2020, Khanna et al., 2020, Lai et al., 2020, Que et al., 2020, Vallée et al., 2020, Wang et al., 2020, Wang et al., 2020, Elhadi and Msherghi, 2021) all with proportions falling within a 7% range (95% CI 10.6–17.4%). For these studies, heterogeneity was reduced to moderate (I2=65.063) and pooled prevalence was 13.5% (95% CI 12.2–14.8%).
As presented in Table 1 , between-group heterogeneity was not significant when analysed by measure (p = 0.062), severity threshold (p = 0.330), survey timeframe (p = 0.681), or risk of bias (p = 0.600).
Table 1.
Sensitivity analysis for depression studies.
| Depression | Studies, N | Pooled,% | 95% CI | I2 | p |
|---|---|---|---|---|---|
| Measure†: | |||||
| PHQ9 | 13 | 16.1 | 10.4–22.8 | 99.316 | 0.062 |
| HADS-D | 7 | 27.5 | 17.6–38.6 | 98.174 | |
| Severity: | 0.330 | ||||
| Mild | 10 | 23.5 | 15.0–33.2 | 99.487 | |
| Moderate | 16 | 18.5 | 14.6–22.9 | 96.395 | |
| Timeframe: | |||||
| First 3 months | 7 | 18.9 | 10.9–28.3 | 97.994 | 0.681 |
| April onwards | 19 | 21.1 | 15.7–27.0 | 99.117 | |
| Risk of bias: | |||||
| Low | 4 | 18.5 | 12.3–25.7 | 96.856 | 0.600 |
| Medium | 22 | 20.9 | 15.6–26.7 | 98.849 |
† Measures with fewer than four studies omitted *p = < 0.05.
3.7.2. Sensitivity analysis for studies of anxiety
Three studies affected the pooled prevalence of anxiety by ≥1% (Jain et al., 2020, Elhadi et al., 2020, Thomaier et al., 2020), the largest impact was a 1.5% change (Jain et al., 2020). After removing the three largest influencing studies, pooled prevalence was 21.8% (95% CI 17.3–26.7%). Cumulative analysis revealed that heterogeneity only reached acceptability for a subset of ten studies (Civantos et al., 2020a, Civantos et al., 2020b, Fauzi et al., 2020, Imran et al., 2020, Malgor et al., 2021, Shalhub et al., 2021, Wang et al., 2020, Wang et al., 2020, Elhadi and Msherghi, 2021, Kannampallil et al., 2020), all with proportions falling within an 8.5% range (95% CI 15.2–23.6%). For these studies, heterogeneity was reduced to moderate (I2=58.054) and pooled prevalence was 20.9% (95% CI 19.5–22.4%).
As presented in Table 2 , between-group heterogeneity was statistically significant when analysed by measure (p = 0.034), severity threshold (p = 0.013), and survey timeframe (p = 0.038), but not by risk of bias (p = 0.089).
Table 2.
Sensitivity analysis for anxiety studies.
| Anxiety | Studies, N | Pooled,% | 95% CI | I2 | p |
|---|---|---|---|---|---|
| Measure†: | |||||
| GAD7 | 17 | 20.3 | 14.3–27.2 | 99.293 |
0.034* |
| HADS-A | 7 | 35.5 | 23.2–49 | 98.639 | |
| Severity: | |||||
| Mild | 10 | 37.2 | 25.0–50.4 | 99.665 |
0.013* |
| Moderate | 20 | 20.5 | 15.9–25.6 | 97.690 | |
| Timeframe: | |||||
| First 3 months | 8 | 17.2 | 9.7–26.3 | 98.206 |
0.038* |
| April onwards | 22 | 29.2 | 22.5–36.4 | 99.327 | |
| Risk of bias: | |||||
| Low | 5 | 19.4 | 14.7–24.6 | 94.133 | 0.089 |
| Medium | 25 | 27.1 | 20.0–35.0 | 98.314 |
† Measures with fewer than four studies omitted * p = < 0.05.
3.8. Secondary analysis
Secondary analysis was performed with all studies (i.e., including those assessed as high risk of bias). The prevalence of depression symptoms for the 16 studies assessed as high risk of bias was 34.6% (95% CI 23.8–46.1%, I2=98.467). When compared with the 26 primary studies assessed as medium or low risk of bias, between-group heterogeneity was statistically significant (p = 0.018) (see SI5). By contrast, the prevalence of anxiety symptoms for the twenty-two studies assessed as high risk of bias (27.0%, 95% CI 20.5–34.0%, I2=98.918) was not significantly different from the 30 studies assessed as medium or low risk of bias (p = 0.787) (see SI6).
3.9. Subgroup analysis
Subgroup categorical information for each study is provided in ST6.
3.9.1. Subgroup analysis for studies of depression
As presented in Table 3 , between-group heterogeneity was statistically significant for studies of depression when analysed by GDP per capita (p = 0.014). Further analysis revealed significant heterogeneity between the <$10,000 and $10–15,000 groups (p = 0.005) but differences were not significant between other groups. Differences were not explained by geographical region (p = 0.282), or by doctors per 10,000 population (p = 0.198).
Table 3.
Subgroup analysis for studies of depression symptoms.
| Depression | Studies, N | Pooled,% | 95% CI | I2 | p |
|---|---|---|---|---|---|
| Region†: | 0.282 | ||||
| Asia | 10 | 14.8 | 9.0–21.7 | 99.339 | |
| Europe | 7 | 21.3 | 13.4–30.5 | 97.697 | |
| North America | 4 | 24.5 | 12.8–38.6 | 98.064 | |
| GDP per capita: | |||||
| >$25,000 | 9 | 20.1 | 12.8–28.6 | 98.150 | 0.014* |
| $10–15,000 | 8 | 13.3 | 9.0–18.4 | 97.349 | |
| <$10,000 | 7 | 28.8 | 19.1–39.6 | 99.030 | |
| Doctors per 100K: | 0.198 | ||||
| >30 | 4 | 16.3 | 12.2–20.8 | 90.204 | |
| 20–29 | 8 | 27.7 | 17.2–39.7 | 98.073 | |
| 15.5–19 | 8 | 15.0 | 8.4–23.0 | 98.541 | |
| <15.5 | 4 | 20.3 | 12.2–29.8 | 99.095 |
† Regions with fewer than four studies omitted * p = < 0.05 ** p = <0.01.
3.9.2. Subgroup analysis for studies of anxiety
As presented in Table 4 , between-group heterogeneity was statistically significant among anxiety studies when analysed by doctors per 10,000 population (p = 0.003). As expected, the highest pooled prevalence of anxiety was calculated for the group of studies with the lowest number of doctors per 10,000 population (<15.5) at 37.9% (95% CI 20.6–56.9%). However, the lowest rates of anxiety were not observed in either of the categories with the highest numbers of doctors per 10,000 population (20–29, >30) but rather for the group of studies within the 15.5–19 doctors per 10,000 population range, with a prevalence of 14.7% (95% CI 9.0–21.5%). Further analysis revealed significant heterogeneity between the 15.5–19 group, when compared with the <15.5 group (p = 0.013), and when compared with the 20–29 group (p = 0.001). GDP per capita was on the threshold of significance (p = 0.054). Differences were not explained by geographical region (p = 0.145).
Table 4.
Subgroup analysis.
| Anxiety | Studies, N | Pooled,% | 95% CI | I2 | p |
|---|---|---|---|---|---|
| Region†: | |||||
| Asia | 10 | 21.5 | 13.1–21.3 | 99.508 |
0.145 |
| Europe | 8 | 21.0 | 12.7–30.8 | 98.255 | |
| North America | 5 | 35.3 | 23.0–48.6 | 98.330 | |
| GDP per capita: | 0.054 | ||||
| >$25,000 | 10 | 25.6 | 16.0–36.6 | 98.980 | |
| $10–15,000 | 10 | 16.4 | 9.4–24.9 | 98.870 | |
| >$10,000 | 8 | 32.7 | 22.3–44.1 | 98.934 | |
| Doctors per 100K: | 0.003** | ||||
| >30 | 5 | 19.1 | 9.1–31.6 | 98.681 | |
| 20–29 | 11 | 32.4 | 24.0–41.4 | 97.796 | |
| 15.5–19 | 8 | 14.7 | 9.0–21.5 | 98.050 | |
| <15.5 | 4 | 37.9 | 20.6–56.9 | 99.51 |
† Regions with fewer than four studies omitted * p = < 0.05 ** p = <0.01.
3.10. Publication bias
Egger's test revealed that publication bias was not statistically significant for studies reporting prevalence of depression symptoms (p = 0.6765), nor for studies reporting anxiety symptoms (p = 0.8973) (see SI3 and SI4 for visual funnel plots).
4. Discussion
4.1. Summary of evidence
The objective of this systematic review and meta-analysis was to provide an estimate of the global prevalence of depression and anxiety symptoms among doctors during the COVID-19 pandemic. The overall pooled prevalence of depression, calculated from 26 studies and 31,447 participants, was 20.5% (95% CI 16.0–25.3%). The overall pooled prevalence of anxiety, calculated from 30 studies and 33,281 participants, was 25.8% (95% CI 20.4–31.5%).
4.2. Comparison with existing evidence
Findings are broadly comparable to earlier estimates for doctors, conducted within the first three to six months of the pandemic. Pappa et al. (2020) conducted a meta-analysis of health care workers up until mid-April 2020. Their subgroup analysis of six studies reporting anxiety data specifically for doctors revealed a pooled prevalence of 21.7% (95% CI 15.3–29.0%); while five studies reported depression data with a pooled prevalence of 25.4% (95% CI 16•6–35.2%). In Santabárbara et al. (2021) meta-analysis of anxiety in health care workers, conducted up until mid-September 2020, a sub-group analysis of 13 studies of doctors reported a more modest pooled prevalence of 17% (95% CI 12.0–22.0%) for anxiety. This figure is comparable to the proportion calculated from the eight studies conducted in the first three months in the current study, but somewhat lower than the overall pooled estimate. However, direct comparisons are difficult due to the wide and overlapping confidence intervals and significant heterogeneity found across reviews.
The prevalence of depression and anxiety symptoms among doctors also falls within the range reported in research conducted during the SARS epidemic ranging from 18% to 57% (Tam et al., 2004; Chan and Huak, 2004; Phua et al., 2005; Nickell et al., 2004; Maunder et al., 2004; Koh et al., 2005). However, these studies reported data on the prevalence of psychological distress rather than symptoms of depression and anxiety. Furthermore, many of these studies focussed on the broader population of healthcare workers, rather than doctors, so a direct comparison is not possible
The results of the current study are also broadly consistent with previous studies conducted prior to the pandemic, indicating very high prevalence of depression and anxiety among doctors. However, evidence of a clear increase compared with pre-pandemic estimates is lacking. As above, direct comparisons are difficult to make as much of the pre-pandemic literature reports the prevalence of psychological distress and/ or burnout, rather than depression and anxiety, for this population. To the author's knowledge, there has only been one systematic review of depression and anxiety in qualified doctors prior to the pandemic (Beyond Blue, 2010); however, pooled prevalence was not calculated due to the wide variation in point prevalence. The narrative summary reported depression as ranging from 14% to 60%, and anxiety ranging from 18% to 55%. Subsequently, a cross-sectional study based in the Netherlands reported prevalence of depression and anxiety among doctors to be 29% and 24% respectively (Ruitenburg et al., 2012). In 2017, a study conducted in Ireland reported 16.6% and 14.4% of doctors with symptoms of depression and anxiety of moderate severity or above (Hayes et al., 2017); although these figures are more modest (particularly in relation to anxiety symptoms) than those reported in the current study, they remain considerably higher than rates in the general population. Previous research has also found higher levels of job demands are associated with reduced wellbeing in doctors (Khan et al., 2018, Lee et al., 2013, Teoh et al., 2021). A tentative hypothesis is that the absence of a clear increase in prevalence of depression and anxiety among doctors during the COVID-19 pandemic, compared with previous estimates, might suggest either a ceiling effect of job demands has been reached, or that greater job resources have been made available during the pandemic to offset the increased demands.
Interestingly, a meta-analysis conducted for the general population, up to June 2020, estimated the global prevalence as 28.0% (95% CI 25.0–31.2%) for depression and 26.9% (95% CI 24.0–30.0%) for anxiety (Nochaiwong et al., 2021). These rates are significantly higher than pre-pandemic global estimates for the general population of 4.7% (4.4–5.0%) for depression (Ferrari et al., 2013) and 7.3% (4.8–10.9%) for anxiety (Baxter et al., 2013). This suggests there may have been a large increase in depression and anxiety symptoms among the general population within the first few months of the pandemic, reaching the consistently high levels reported among doctors. Furthermore, while levels of anxiety in the Nochaiwong study appear similar to those reported for doctors in the current study (26.9% vs 25.8%), levels of depression appear significantly higher in the global general population compared to those observed in doctors in the current study (28.0% vs 20.5%). Given that reduced activity is associated with depression, this finding might be explained by the presumed greater levels of inactivity within the general population, due to lockdown restrictions. Whereas doctors, as essential workers, may have experienced a less severe loss of routine. It is also of note that the pre-pandemic Ferrari and Baxter meta-analyses used studies that estimated prevalence based on ‘gold standard’ diagnostic interview procedures rather than self-report, which may account for some of the difference in outcomes.
The data from this study suggests that doctors continue to be a population at high risk of depression and anxiety, but the evidence does not support a clear increase in symptoms, compared with pre-pandemic data.
4.3. Sub-group heterogeneity
The subgroup analyses conducted in this review (geographical region, doctors per 10,000 population, GDP per capita) were able to explain some of the heterogeneity in depression and anxiety studies, but not consistently. When comparing prevalence based on GDP per capita, there was significant between-group heterogeneity for depression (p = 0.014), and threshold significance for anxiety (p = 0.054). As expected, the highest prevalence rates were recorded for the lowest GDP per capita (<$10,000 studies), with pooled prevalence of 28.8% (95% CI 19.1–39.6%) for depression and 32.7% (95% CI 22.3–44.1%) for anxiety. However, notably, for both sub-group analyses, the lowest levels of depression and anxiety were not reported for countries with the highest GDP per capita (>$25,000), but for studies in the $10–15,000 level, with prevalence of depression at 13.3% (95% CI 9.0–18.4%) and of anxiety at 16.4% (95% CI 9.4–24.9%). These findings are consistent with previous research that suggests that beyond a certain level of wealth and resource, additional benefit to emotional wellbeing is minimal (Kahneman and Deaton, 2010).
Findings are somewhat consistent with the JD-R model, which was used to select the subgroup comparisons of GDP per capita and doctors per 10,000 population as factors that may be expected to increase job demands and reduce job resources for doctors during the pandemic. Lowest GDP corresponded with highest rates of depression symptoms, and lowest numbers of doctors per 10,000 corresponded with highest rates of anxiety.
4.4. Methodological heterogeneity
The methodological differences explored via sensitivity analyses (risk of bias, measure, severity threshold, survey timeframe) did not explain the heterogeneity for depression studies, apart from when comparing high risk of bias with low/ medium risk of bias studies (p = 0.018). High risk of bias studies produced a prevalence of 34.6% (23.8–46.1%) whereas low/medium risk of bias studies produced a prevalence of 20.5% (16.0–25.3%). Conversely, all of the methodological differences were relevant in explaining the heterogeneity in anxiety studies, apart from risk of bias (high vs low/medium p = 0.787).
The type of measure used in depression studies did not produce statistically significant differences in estimates (p = 0.062). Pooled prevalence was 16.1% (95% CI 10.4–22.8%) for the PHQ9 and 27.5% (95% CI 17.6–38.6%) for the HADS-D. However, for anxiety, there was a significant difference between studies using the GAD7 vs those using the HADS-A (p = 0.034). Pooled prevalence was 20.3% (95% CI 14.3–27.2%) for the GAD7 and 35.5% (95% CI 23.2–49.1%) for the HADS-A. This may be explained by potential differences in the underlying factor being measured. For example, a meta confirmatory factor analysis of the HADS identified a strong general factor. The authors suggested that it does not provide good separation between symptoms of anxiety and depression and recommended it may be best used as a measure of general distress (Norton et al., 2013).
Reporting of mild vs moderate and above symptoms did not produce statistically different prevalence estimates for depression (p = 0.330) but did for anxiety (p = 0.013). Studies reporting mild and above symptoms of anxiety produced a pooled prevalence of 37.2% (95% CI 25.0–50.4%) whereas studies reporting moderate and above symptoms produced a more modest estimate of 20.5% (95% CI 15.9–25.6%). The lack of consensus and consistency across studies regarding what constitutes clinically significant levels of anxiety symptoms, and the poor equivalence when comparing severity levels across different measures, presents a challenge when attempting to estimate an overall prevalence (Clover et al., 2020).
The timeframe of data collection was not significant for depression studies (p = 0.681) but was for anxiety studies (p = 0.038). Interestingly, the pooled prevalence of anxiety symptoms was significantly lower in studies conducted within the first three months of the pandemic (17.2%, 95% CI 9.7–26.3%) compared with studies reporting data from April onwards (29.2%, 95% CI 22.5–36.4%). Although this was based on a small subgroup of eight studies. This finding is in contrast to research in the UK general population between 23rd March and 9th August 2020 that suggest symptoms of anxiety were higher in the first few months before gradually declining (Fancourt et al., 2021). This finding might be understood as the consequence of chronic stress on the medical workforce as the pandemic progressed. However, it is also of note that findings from the UK-based study (Fancourt et al., 2021) are not consistent with the pooled prevalence reported in a similar timeframe from the global meta-analysis (Nochaiwong et al., 2021). This inconsistency is reflective of the overall high variability in the evidence.
4.5. Limitations
This review has several limitations. Firstly, there are a number of limitations associated with the methodology of the studies of interest. As with all observational research, causation cannot be inferred. The predominant use of non-probability sampling methods introduced the highest levels of bias. This methodology means that a sampling frame and stratified random sampling approach is typically absent, which has implications for coverage bias and the ability to calculate a response rate. In addition, the widespread use of online-only survey, although appropriate given the global context, may have introduced further coverage bias by excluding people who were too busy or overwhelmed to access their emails or social media. Other potential sources of bias include self-selection bias, which may be introduced by disproportionately attracting doctors with a past history or particular interest in mental health. Conversely, social desirability bias can also be introduced by the use of self-report measures. All of which can influence study results. Another significant limitation is the high heterogeneity observed across studies. Heterogeneity is inherent in meta-analyses of this type of data, but limits confidence in the conclusions drawn. Given the between-study variability in geographical location, settings, and specialities, generalisability may be limited. Lack of consistency in methodological approaches also limits confidence in conclusions, including the use of a wide variety of questionnaires, differences in cut-offs and severity thresholds, and absence of ‘gold standard’ diagnostic interviews.
There are also several limitations associated with the methodology of the overall review. High risk of bias studies were excluded, with the aim of reducing overall bias and increasing homogeneity (Higgins et al., 2011; Detweiler et al., 2016). However, a drawback of analysis with a reduced sample is a reduction in overall precision. Sensitivity analysis incorporating high risk studies indicated that omitting these studies from the primary analyses of anxiety was not sufficient to explain heterogeneity. However, the significant difference in pooled prevalence in depression studies highlights the potential utility of this approach in avoiding overestimation of distress. Inter-rater reliability for risk of bias ratings was not an available as a function within the software used. Reporting bias may have been introduced by the exclusion of gray literature, non-English language papers, and inaccessible papers. While this study covered symptoms of depression and anxiety, specific anxiety disorders and other mental health conditions were excluded. It may also have been useful to consider the influence of additional variables, including indicators of more localised job demands, such as local infection rates during the timeframe for each study, and indicators of resources, such as organisational, social and psychological factors. Finally, although this review covers more than twelve months of research conducted during the pandemic, any studies published after the 3rd March 2021 will be absent from analyses. Given the rate at which new studies are being published, a more updated meta-analysis may soon be required.
4.6. Quality of evidence
The overall quality of evidence likely falls within the low to very low range, as per GRADE assessment guidelines. All observational research begins as low quality. Given the wide-ranging point prevalence observed across studies, the broad confidence intervals around pooled prevalence estimates, and the high level of heterogeneity observed, this assessment appears to be a fair reflection. This means that the estimate of effect is uncertain and future research may change this estimate. Recommendations for improving the quality of future research are outlined below.
4.7. Strengths
Despite these limitations, this review has a number of strengths. Firstly, risk of bias assessment highlighted a number of strengths in the individual studies. The vast majority of studies used appropriate and valid methods to identify depression and/or anxiety and measured the condition(s) in a standard and reliable way for all participants. Most studies appropriately described and reported the statistical analyses conducted. Setting and characteristics were also largely well described.
In consideration of the overall review, to our knowledge, this is the first systematic review and meta-analysis of the global prevalence of symptoms of depression and anxiety among doctors during the pandemic. The number of studies returned in our searches was unexpectedly high; enabling us to be more selective in the quality of the studies included for full analysis. Although high risk of bias studies were excluded from the primary analyses, secondary analysis was also conducted to compare high vs medium/ low risk of bias studies. While between-group heterogeneity was not significant when comparing the risk of bias for anxiety studies, heterogeneity was significant for depression studies. The more modest pooled prevalence for depression, using just the lower risk studies, may therefore be considered a more accurate estimate. Data were extracted for cases above clinical cut-off thresholds; for the majority of studies, reported cut-offs were within the moderate severity range. In the few studies where a specific cut-off score was not reported, data were extracted for cases in the moderate and above categories. Studies reporting prevalence estimates based on predominantly mild symptoms are likely to provide an overinflated estimation of mental health conditions in this population; therefore, the pooling of predominantly moderate and above estimates may offer a more accurate reflection of the prevalence of clinically relevant symptoms in doctors than studies including data for all levels of symptom severity. Further strengths include the large number of overall participants from across the globe, spanning a wide range of clinical specialities and settings. Subgroup analyses, exploring the potential impact of job demands, provides some additional insight into factors that may be influencing prevalence.
4.8. Recommendations
Given the evidence for high levels of depression and anxiety symptoms among doctors across the world, health care services should consider multi-level approaches to support (Bakker and Demerouti, 2018). Firstly, organisational and structural changes are needed to ensure doctors have access to the most fundamental resources, such as time to sleep, eat, exercise, and spend time with others (Unadkat and Farquhar, 2020). Ongoing efforts should be made to destigmatise discussions around mental health (Galbraith et al., 2020). Formal and informal peer support systems may help to facilitate these conversations and should be encouraged (Behrman et al., 2020). Schwartz rounds are increasing in popularity, are well received by staff (Flanagan et al., 2020), and can normalize conversations around the emotional impact of work and reduce stigma. Similarly, formal and informal psychology input should be embedded within health services. Services should consider incorporating evidence based and high-quality interventions, such as those based on mindfulness and cognitive-behavioural therapy, which have been found to be effective in reducing stress, anxiety, and depression for doctors and nurses (Melnyk et al., 2020; Murray et al., 2016). Systems to monitor the wellbeing of doctors should be in place, and in cases where one-to-one psychological support is required there should be clear and discreet pathways to referral.
Further longitudinal research is needed to monitor long-term outcomes and to explore potential differences in trajectory of mental health outcomes for doctors compared with other populations. Future research may benefit from greater consideration of individual, social and organisational demands and resources. Improvements to research methodology would also increase the overall quality of the evidence base and enable greater confidence in conclusions. Specifically, the adoption of random probability sampling methods is needed. There also needs to be more consistency in measurement. Future studies would benefit from adopting ‘gold standard’ diagnostic interview methods, using only measures with the strongest psychometric properties, utilizing cut-offs that optimize sensitivity and specificity in identifying clinically relevant symptoms, and reporting on a broader range of cut-offs in order to facilitate better comparisons with studies using alternative measures (Clover et al., 2020; Cameron et al., 2008).
4.9. Conclusion
This systematic review and meta-analysis provides a comprehensive analysis of the global prevalence of depression and anxiety symptoms among doctors during the first twelve months of the COVID-19 pandemic. Symptoms of depression and anxiety are elevated among doctors, compared with earlier research from the general population, but not conclusively more so than pre-pandemic levels among doctors. Differences in study design and variation in job demands may account for some of the observed heterogeneity. Findings may help to quantify the needs of this population and guide health care systems to plan support as we recover from the pandemic, and prepare for other times of national or global crisis.
Role of funding sources
This review was conducted as part of doctoral training and is funded by NHS Wales.
CRediT authorship contribution statement
GJ designed the study and protocol, conducted literature searches, screening, data extraction, quality assessment, statistical analysis, and wrote the manuscript. VS contributed to the design and coordination of the study and provided input into the final drafts. LF conducted independent screening and full text review. JS conducted independent data extraction and quality assessment. LW contributed to the design and coordination of the study, provided input into the final drafts and was the primary supervisor. All authors have approved the final manuscript.
Registration and protocol
The protocol was registered on PROSPERO and can be accessed online (CRD42021228667).
Conflict of Interest
The authors declare no conflicts of interest.
Acknowledgements
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.11.026.
Appendix. Supplementary materials
References
- American Psychiatric Association . American Psychiatric Pub; 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) [Google Scholar]
- Bakker A.B., Demerouti E. Job demands–resources theory: taking stock and looking forward. J. Occup. Health Psychol. 2017;22(3):273. doi: 10.1037/ocp0000056. [DOI] [PubMed] [Google Scholar]
- Bakker, A.B., & Demerouti, E. (2018). Multiple levels in job demands-resources theory: implications for employee well-being and performance.
- Balshem H., Helfand M., Schünemann H.J., Oxman A.D., Kunz R., Brozek J.…Guyatt G.H. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011;64(4):401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- Barendregt J.J., Doi S.A., Lee Y.Y., Norman R.E., Vos T. Meta-analysis of prevalence. J. Epidemiol. Community Health. 2013;67(11):974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- Baxter A.J., Scott K.M., Vos T., Whiteford H.A. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol. Med. 2013;43(5):897. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 1988;56(6):893. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Behrman S., Baruch N., Stegen G. Peer support for junior doctors: a positive outcome of the COVID-19 pandemic? Future healthcare journal. 2020;7(3):e64. doi: 10.7861/fhj.2020-0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyond Blue. National Mental Health Survey of Doctors and Medical Students (2010). https://www.beyondblue.org.au/docs/default-source/research-project-files/bl1132-report-nmhdmss-full-report_web.
- Brady K.J., Trockel M.T., Khan C.T., Raj K.S., Murphy M.L., Bohman B.…Roberts L.W. What do we mean by physician wellness? A systematic review of its definition and measurement. Academic Psychiatry. 2018;42(1):94–108. doi: 10.1007/s40596-017-0781-6. [DOI] [PubMed] [Google Scholar]
- Cameron I.M., Crawford J.R., Lawton K., Reid I.C. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. British Journal of General Practice. 2008;58(546):32–36. doi: 10.3399/bjgp08X263794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D., Riley W., Stone A., Rothrock N., Reeve B., Yount S.…Cooperative Group PROMIS. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J. Clin. Epidemiol. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A.O., Huak C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Chic Ill) 2004;54(3):190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatzittofis A., Karanikola M., Michailidou K., Constantinidou A. Impact of the COVID-19 pandemic on the mental health of healthcare workers. J. Environ. Res. 2021;18(4) doi: 10.3390/ijerph18041435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civantos A.M., Bertelli A., Goncalves A., Getzen E., Chang C., Long Q., Rajasekaran K. Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: A national study. Journal of Otolaryngology. 2020;41(6):102694. doi: 10.1016/j.amjoto.2020.102694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civantos A.M., Byrnes Y., Chang C., Prasad A., Chorath K., Poonia S.K., Jenks C.M., Bur A.M., Thakkar P., Graboyes E.M., Seth R., Trosman S., Wong A., Laitman B.M., Harris B.N., Shah J., Stubbs V., Choby G., Long Q., Rajasekaran K. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head & Neck. 2020;42(7):1597–1609. doi: 10.1002/hed.26292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clover K., Lambert S.D., Oldmeadow C., Britton B., King M.T., Mitchell A.J., Carter G.L. Apples to apples? Comparison of the measurement properties of hospital anxiety and depression-anxiety subscale (HADS-A), depression, anxiety and stress scale-anxiety subscale (DASS-A), and generalised anxiety disorder (GAD-7) scale in an oncology setting using Rasch analysis and diagnostic accuracy statistics. Current Psychology. 2020:1–10. [Google Scholar]
- Covidence systematic review software (2021). Veritas Health Innovation, Australia. Available at www.covidence.org.
- Dai Y., Zhang B., Sun H., Li Z., Shen L., Liu Y. Prevalence and correlates of psychological symptoms in Chinese doctors as measured with the SCL-90-R: a meta-analysis. Res. Nurs. Health. 2015;38(5):369–383. doi: 10.1002/nur.21673. [DOI] [PubMed] [Google Scholar]
- De Sio S., Buomprisco G., Perri R., Bruno G., Mucci N., Nieto H.A.…Cedrone F. Work-related stress risk and preventive measures of mental disorders in the medical environment: an umbrella review. Eur. Rev. Med. Pharmacol. Sci. 2020;24(2):821–830. doi: 10.26355/eurrev_202001_20065. [DOI] [PubMed] [Google Scholar]
- Demerouti E., Bakker A.B., Nachreiner F., Schaufeli W.B. The job demands-resources model of burnout. Journal of Applied psychology. 2001;86(3):499. [PubMed] [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Detweiler B.N., Kollmorgen L.E., Umberham B.A., Hedin R.J., Vassar B.M. Risk of bias and methodological appraisal practices in systematic reviews published in anaesthetic journals: a meta-epidemiological study. Anaesthesia. 2016;71(8):955–968. doi: 10.1111/anae.13520. [DOI] [PubMed] [Google Scholar]
- Dong M., Zhou F.C., Xu S.W., Zhang Q., Ng C.H., Ungvari G.S., Xiang Y.T. Vol. 50. Suicide and Life-Threatening Behavior; 2020. pp. 1264–1275. (Prevalence of Suicide-Related Behaviors Among physicians: A systematic Review and Meta-Analysis). [DOI] [PubMed] [Google Scholar]
- Dyrbye L.N., Thomas M.R., Shanafelt T.D. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Academic medicine. 2006;81(4):354–373. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhadi, M., Msherghi, A., Elgzairi, M., Alhashimi, A., Bouhuwaish, A., Biala, M., Abuelmeda, S., Khel, S., Khaled, A., Alsoufi, A., Elhadi, A., & BenGhatnsh, A. (2020). The Mental Well-Being of Frontline Physicians Working in Civil Wars Under Coronavirus Disease 2019. [DOI] [PMC free article] [PubMed]
- Elhadi M., Msherghi A. Mental health of surgeons during the COVID-19 pandemic: An urgent need for intervention. Surgery. 2021;169(2):477–478. doi: 10.1016/j.surg.2020.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck M.W., Derakshan N., Santos R., Calvo M.G. Anxiety and cognitive performance: attentional control theory. Emotion. 2007;7(2):336. doi: 10.1037/1528-3542.7.2.336. [DOI] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. The Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauzi M.F.M., Yusoff H.M., Robat R.M., Saruan N.A.M., Ismail K.I., Haris A.F.M. Doctors’ mental health in the midst of COVID-19 pandemic: The roles of work demands and recovery experiences. Int. J. Environ. Res. Public Health. 2020;17(19) doi: 10.3390/ijerph17197340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari A.J., Somerville A.J., Baxter A.J., Norman R., Patten S.B., Vos T., Whiteford H.A. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol. Med. 2013;43(3):471. doi: 10.1017/S0033291712001511. [DOI] [PubMed] [Google Scholar]
- Flanagan E., Chadwick R., Goodrich J., Ford C., Wickens R. Reflection for all healthcare staff: a national evaluation of Schwartz rounds. J. Interprof. Care. 2020;34(1):140–142. doi: 10.1080/13561820.2019.1636008. [DOI] [PubMed] [Google Scholar]
- Florin M., Pinar U., Chavigny E., Bouaboula M., Jarboui L., Coulibaly A., Lemogne C., Fournier L. Socio-economic and psychological impact of the COVID-19 outbreak on private practice and public hospital radiologists. J. Radiology. 2020;1:109285. doi: 10.1016/j.ejrad.2020.109285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman M.F., Tukey J.W. Transformations related to the angular and the square root. Ann. Math. Stat. 1950:607–611. [Google Scholar]
- Galbraith N., Boyda D., McFeeters D., Hassan T. The mental health of doctors during the COVID-19 pandemic. BJPsych. Bull. 2020:1–4. doi: 10.1192/bjb.2020.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt G.H., Oxman A.D., Vist G.E., Kunz R., Falck-Ytter Y., Alonso-Coello P., Schünemann H.J. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallion L.S., Tolin D.F., Assaf M., Goethe J., Diefenbach G.J. Cognitive control in generalized anxiety disorder: relation of inhibition impairments to worry and anxiety severity. Cognit. Ther. Res. 2017;41(4):610–618. [Google Scholar]
- Hayes B., Prihodova L., Walsh G., Doyle F., Doherty S. What's up doc? A national cross-sectional study of psychological wellbeing of hospital doctors in Ireland. BMJ Open. 2017;7(10) doi: 10.1136/bmjopen-2017-018023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D.…Sterne J.A. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011:343. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilmi M., Boileve A., Ducousso A., Michalet M., Turpin A., Neuzillet C., Naoun N. Professional and Psychological Impacts of the COVID-19 Pandemic on Oncology Residents: A National Survey. JCO Global Oncology. 2020;1:1674–1683. doi: 10.1200/GO.20.00376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L.…Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imran N., Masood H.M.U., Ayub M., Gondal K.M. Psychological impact of COVID-19 pandemic on postgraduate trainees: A cross-sectional survey. Postgraduate Medical J. 2020;1 doi: 10.1136/postgradmedj-2020-138364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M.A., Alam S.S., Kundu S., Hossan T., Kamal M.A., Cavestro C. Prevalence of Headache in Patients with Coronavirus Disease 2019 (COVID-19): a Systematic Review and Meta-Analysis of 14,275 Patients. Front Neurol. 2020:11. doi: 10.3389/fneur.2020.562634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A., Teoh K.R., Islam S., Hassard J. Psychosocial work characteristics, burnout, psychological morbidity symptoms and early retirement intentions: a cross-sectional study of NHS consultants in the UK. BMJ Open. 2018;8(7) doi: 10.1136/bmjopen-2017-018720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain A., Singariya G., Kamal M., Kumar M., Jain A., Solanki R.K. COVID-19 pandemic: Psychological impact on anaesthesiologists. J. Anaesthesia. 2020;64(9):774–783. doi: 10.4103/ija.IJA_697_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahneman D., Deaton A. High income improves evaluation of life but not emotional well-being. Proc. Natl. Acad. Sci. 2010;107(38):16489–16493. doi: 10.1073/pnas.1011492107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannampallil, T. G., Goss, C. W., Evanoff, B. A., Strickland, J. R., McAlister, R. P., & Duncan, J. (2020). Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS ONE [Electronic Resource], 15(8), e0237301. [DOI] [PMC free article] [PubMed]
- Khanna R.C., Honavar S.G., Metla A.L., Bhattacharya A., Maulik P.K. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. J. Ophthalmology. 2020;68(6):994–998. doi: 10.4103/ijo.IJO_1458_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh D., Lim M.K., Chia S.E., Ko S.M., Qian F., Ng V.…Fones C. Med. Care. 2005. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare Workers in Singapore What can we Learn? pp. 676–682. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Monahan P.O., Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee W.J., Maunder R.G., Goldbloom D.S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric services. 2008;59(1):91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaire, J.B., & Wallace, J.E. (2017). Burnout among doctors. [DOI] [PubMed]
- Lee R.T., Seo B., Hladkyj S., Lovell B.L., Schwartzmann L. Correlates of physician burnout across regions and specialties: a meta-analysis. Human resources for health. 2013;11(1):1–16. doi: 10.1186/1478-4491-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Mao X., Li J., Fang L., Du G., Qiao J., Jia X. Anxiety and Depression Among Imaging Doctors in Post-COVID-19 Period. SN Comprehensive Clinical Medicine. 2020;1:1–5. doi: 10.1007/s42399-020-00654-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Löwe B., Kroenke K., Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) J. Psychosom. Res. 2005;58(2):163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Rourke S., Hunter J.J., Goldbloom D., Balderson K.…Fones C.S. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 2004;66(6):938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- Malgor R.D., Sobreira M.L., Mouawad N.J., Johnson A.P., Wohlauer M.V., Coogan S.M., Shalhub S. Brazilian vascular surgeons experience during the coronavirus (COVID-19) pandemic. Vascular. 2021;29(3):451–460. doi: 10.1177/1708538120954961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S.…Wasylenki D.A. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infect. Dis. 2006;12(12):1924. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk B.M., Kelly S.A., Stephens J., Dhakal K., McGovern C., Tucker S.…Bird S.B. Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: a systematic review. Am. J. Heal. Promo. 2020;34(8):929–941. doi: 10.1177/0890117120920451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migliavaca C.B., Stein C., Colpani V., Munn Z., Falavigna M. Quality assessment of prevalence studies: a systematic review. J. Clin. Epidemiol. 2020;127:59–68. doi: 10.1016/j.jclinepi.2020.06.039. [DOI] [PubMed] [Google Scholar]
- Moran T.P. Anxiety and working memory capacity: a meta-analysis and narrative review. Psychol. Bull. 2016;142(8):831. doi: 10.1037/bul0000051. [DOI] [PubMed] [Google Scholar]
- Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int. J. Evid. Based Healthcare. 2015;13(3):147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- Murray M., Murray L., Donnelly M. Systematic review of interventions to improve the psychological well-being of general practitioners. BMC Fam. Pract. 2016;17(1):1–14. doi: 10.1186/s12875-016-0431-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S.…Upshur R.E. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nochaiwong S., Ruengorn C., Thavorn K., Hutton B., Awiphan R., Phosuya C.…Wongpakaran T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci. Rep. 2021;11(1):1–18. doi: 10.1038/s41598-021-89700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton S., Cosco T., Doyle F., Done J., Sacker A. The Hospital Anxiety and Depression Scale: a meta confirmatory factor analysis. J. Psychosom. Res. 2013;74(1):74–81. doi: 10.1016/j.jpsychores.2012.10.010. [DOI] [PubMed] [Google Scholar]
- Nyaga V.N., Arbyn M., Aerts M. Vol. 72. Archives of Public Health; 2014. pp. 1–10. (Metaprop: a Stata command to Perform Meta-Analysis of Binomial Data). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phua D.H., Tang H.K., Tham K.Y. Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Academ. Emerg. Medic. 2005;12(4):322–328. doi: 10.1197/j.aem.2004.11.015. [DOI] [PubMed] [Google Scholar]
- Que J., Shi L., Deng J., Liu J., Zhang L., Wu S., Gong Y., Huang W., Yuan K., Yan W., Sun Y., Ran M., Bao Y., Lu L. Psychological impact of the COVID-19 pandemic on healthcare workers: A cross-sectional study in China. General Psychiatry. 2020;33(3) doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rock P.L., Roiser J.P., Riedel W.J., Blackwell A.D. Cognitive impairment in depression: a systematic review and meta-analysis. Psychol. Med. 2014;44(10):2029. doi: 10.1017/S0033291713002535. [DOI] [PubMed] [Google Scholar]
- Royal College of Physicians . Royal College of Physicians; London: 2015. Work and Wellbeing in the NHS: Why Staff Health Matters to Patient Care. [Google Scholar]
- Ruitenburg M.M., Frings-Dresen M.H., Sluiter J.K. The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: a cross-sectional study. BMC Health Serv. Res. 2012;12(1):1–7. doi: 10.1186/1472-6963-12-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runswick O.R., Roca A., Williams A.M., Bezodis N.E., North J.S. The effects of anxiety and situation-specific context on perceptual–motor skill: a multi-level investigation. Psychol. Res. 2018;82(4):708–719. doi: 10.1007/s00426-017-0856-8. [DOI] [PubMed] [Google Scholar]
- Salari N., Khazaie H., Hosseinian-Far A., Khaledi-Paveh B., Kazeminia M., Mohammadi M.…Eskandari S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum. Resour. Health. 2020;18(1):1–14. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Bueno-Notivol J., Lipnicki D.M., Olaya B., Pérez-Moreno M., Gracia-García P.…Ozamiz-Etxebarria N. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021 doi: 10.1016/j.pnpbp.2021.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarria-Santamera A., Orazumbekova B., Terzic M., Issanov A., Chaowen C., Asúnsolo-del-Barco A. Vol. 9. Multidisciplinary Digital Publishing Institute; 2021. Systematic Review and Meta-Analysis of Incidence and Prevalence of Endometriosis; p. 29. (In Healthcare). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shalhub S., Mouawad N.J., Malgor R.D., Johnson A.P., Wohlauer M.V., Coogan S.M., Woo K. Global vascular surgeons’ experience, stressors, and coping during the coronavirus disease 2019 pandemic. J. Vascular Surgery. 2021;73(3):762–771. doi: 10.1016/j.jvs.2020.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoda E.-M., Teufel M., Stang A., Jockel K.-H., Junne F., Weismuller B., Hetkamp M., Musche V., Kohler H., Dorrie N., Schweda A., Bauerle A. Psychological burden of healthcare professionals in Germany during the acute phase of the COVID-19 pandemic: Differences and similarities in the international context. J. Public Health. 2020;42(4):688–695. doi: 10.1093/pubmed/fdaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- StataCorp, 2019; Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC.
- Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D.…Thacker S.B. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Tam C.W., Pang E.P., Lam L.C., Chiu H.F. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004;34(7):1197. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- Teoh K.R.H., Hassard J., Cox T. Doctors’ working conditions, wellbeing and hospital quality of care: a multilevel analysis. Saf. Sci. 2021;135 [Google Scholar]
- Tian-Ci Quek T., Tam W.S., X Tran B., Zhang M., Zhang Z., Su-Hui Ho C., Chun-Man Ho R. The global prevalence of anxiety among medical students: a meta-analysis. Int. J. Environ. Res. Public Health. 2019;16(15):2735. doi: 10.3390/ijerph16152735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomaier, L., Teoh, D., Jewett, P., Beckwith, H., Parsons, H., Yuan, J., Blaes, A. H., Lou, E., Hui, J. Y. C., & Vogel, R. I. (2020). Emotional health concerns of oncology physicians in the United States: Fallout during the COVID-19 pandemic. [DOI] [PMC free article] [PubMed]
- Unadkat S., Farquhar M. Doctors’ wellbeing: self-care during the covid-19 pandemic. BMJ. 2020:368. doi: 10.1136/bmj.m1150. [DOI] [PubMed] [Google Scholar]
- Vallée M., Kutchukian S., Pradere B., Verdier E., Durbant È., Ramlugun D., Saiydoun G. Prospective and observational study of COVID-19’s impact on mental health and training of young surgeons in France. J. British Surgery. 2020;107(11):e486–e488. doi: 10.1002/bjs.11947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughan J.P., Morrow R.H., World Health Organization . World Health Organization; 1989. Manual of Epidemiology For District Health Management. [Google Scholar]
- Wallace J.E., Lemaire J.B., Ghali W.A. Physician wellness: a missing quality indicator. The Lancet. 2009;374(9702):1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- World Health Organisation. Coronavirus disease (COVID-19) pandemic. Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- Wang H., Huang D., Huang H., Zhang J., Guo L., Liu Y., Ma H., Geng Q. The psychological impact of covid-19 pandemic on medical staff in guangdong, china: A cross-sectional study. Psychological Medicine, No-Pagination Specified. 2020 doi: 10.1017/S0033291720002561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Ma S., Yang C., Cai Z., Hu S., Zhang B., Liu Z. Acute psychological effects of Coronavirus Disease 2019 outbreak among healthcare workers in China: a cross-sectional study. Translational psychiatry. 2020;10(1):1–10. doi: 10.1038/s41398-020-01031-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson E. UK NHS staff: stressed, exhausted, burnt out. The Lancet. 2015;385(9971):841–842. doi: 10.1016/S0140-6736(15)60470-6. [DOI] [PubMed] [Google Scholar]
- Wilson, M.R. (2012). Anxiety: attention, the brain, the body and performance. The Oxford handbook of sport and performance psychology, 173–190.
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.