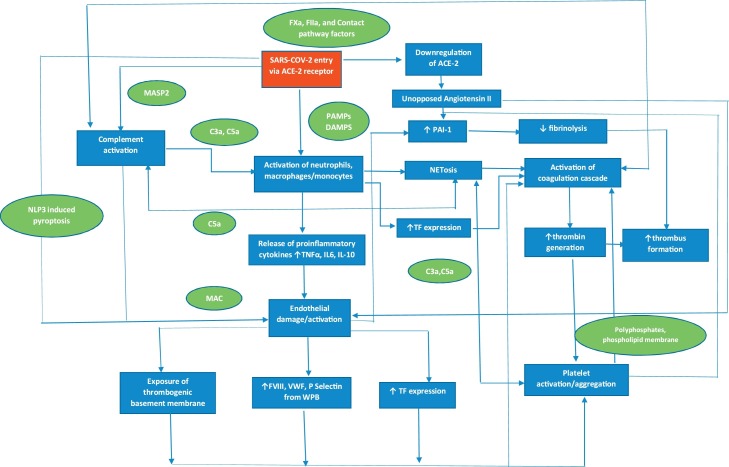
Fig. 1.
Pathophysiology of COVID-19 associated coagulopathy. SARS-CoV2 triggers the release of cytokines from monocytes, macrophages and neutrophils leading to a cytokine storm. This results in activation of monocytes, macrophages and neutrophils with upregulation of tissue factor and release of NETs. The endothelium is damaged/activated due to pyroptosis induced by direct viral invasion, release of cytokines, complement activation and downregulation of ACE2. This leads to exposure of the thrombogenic basement membrane, upregulation of tissue factor and release of factor VIII, VWF and P-Selectin from WPB resulting in activation of platelets and coagulation factors. Fibrinolysis is also suppressed due to inhibition of PAI-I further contributing to the procoagulant state. In addition, there is significant cross talk between the immune, complement, and coagulation systems leading to a positive feedback loop, thus amplifying this response. ACE-2, angiotensin converting enzyme 2; C, complement; COVID-19, coronavirus disease 2019; IL, interleukin; NET, neutrophil extracellular trap; MASP2, Mannan-binding lectin serine protease 2; MAC; membrane attack complex; NLP3, NLR pyrin domain containing 3; PAI-1, plasminogen activator inhibitor 1; SARS-CoV2, severe acute respiratory syndrome coronavirus 2; TF, tissue factor; TNF, tumour necrosis factor; WPB, Weibel Palade body.