Abstract
Objective:
To evaluate the morphologic features and the relative position of the incisive canal with regard to the maxillary incisor roots using computed tomography (CT).
Materials and Methods:
Morphologic evaluation of the incisive canal and its proximity to the maxillary central incisors were measured using CT images of 38 adults with skeletal and dental class I normal occlusion. Linear measurements were performed on the axial cross-sectional images corresponding to three vertical levels, the palatal opening of the incisive canal (L1), midlevel between the opening level and the root apex of the maxillary central incisors (L2), and the root apex of the maxillary central incisors (L3).
Results:
The percentage of subjects with an incisive canal width greater than the interroot distance of the central incisors was 86.8% and 63.2% at levels L1 and L2, respectively. The anteroposterior distance between the maxillary incisor roots and the boarder of the incisive canal was approximately 5–6 mm at levels L1 and L2.
Conclusion:
The anteroposterior distance between the maxillary central incisor roots and the incisive canal was approximately 5–6 mm. More than 60% of the subjects had an incisive canal width greater than the interroot distance. Evaluation of the proximity of the incisive canal to the maxillary incisors, along with its dimensional characteristics, may be helpful when a considerable amount of maxillary retraction is planned.
Keywords: Incisive canal, Tooth movement, Envelope of discrepancy, Maximum retraction, Complication
INTRODUCTION
The maxillary anterior teeth are important not only in achieving pleasing dental and facial esthetics but also in physiological functions including pronunciation and mastication.1–5 Therefore, determination of the three-dimensional (3D) position of the maxillary incisors is an integral part of orthodontic diagnosis and treatment planning, and various biomechanical treatment modalities are employed to achieve the ideal incisor position.
The extent of orthodontic tooth movement is constrained by the periodontal attachment apparatus; adjacent anatomical structures, such as the alveolar bone, tongue, and lips; and the biomechanical limits of anchorage during orthodontic mechanotherapy.6–10 Ackerman and Proffit introduced the concept of the “envelope of discrepancy,” which graphically shows the extent of changes possible with orthodontic tooth movement alone, with orthopedic or functional appliance therapy for growth modification, and with orthognathic surgery in combination with orthodontic treatment.7,11 Accordingly, it is traditionally thought that the amount of changes possible for the maxillary incisors with orthodontic treatment alone are approximately 7, 2, 4, and 2 mm for retraction, protraction, extrusion, and intrusion, respectively. Interestingly, the range of tooth movement during retraction of the maxillary incisors far exceeds the range of movement possible in other directions and/or for other teeth.
The anatomical limit of maxillary incisor retraction is reportedly the palatal cortical plate.12–16 However, another anatomical structure, the incisive canal, runs more closely to the maxillary incisor roots between the central incisor roots in the median plane than does the palatal cortical plate. The incisive canal connects the floor of the nasal cavity with the palate and opens into the oral cavity as the incisive foramen posterior to the maxillary central incisors. It runs parallel to the maxillary central incisors and transmits the nasopalatine vessels and nerves, branches of the maxillary artery, and the trigeminal nerve and is surrounded by a thick layer of cortical bone.17–22 Because of its proximity to the maxillary incisors, the possibility of surgical invasion of the incisive canal during dental procedures has been reported, and this can result in nonosseointegration of dental implants or sensory dysfunction.23,24
Although the overall anatomy of the incisive canal is well defined, its precise location in relation to the maxillary incisors is not well documented in the orthodontic literature. This may be because of the difficulties in detecting incisive canal morphology using conventional orthodontic radiographs. However, with recent advancements in 3D imaging, the approximation of the maxillary incisor roots to the incisive canal can be frequently detected after anterior retraction following orthodontic treatment (Figure 1). Interestingly, the contact of maxillary central incisor root with the incisive canal after maximum retraction was associated with apparent root resorption raising potent complications.25
Figure 1.
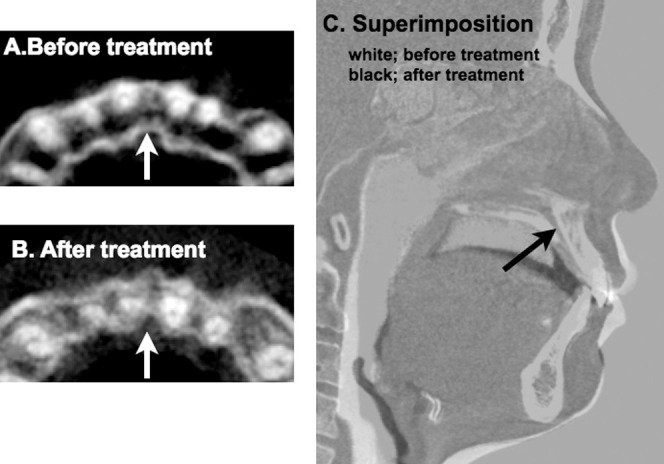
Cone beam computed tomography (CBCT) images of the incisive canal and superimposition before and after anterior retraction. Axial sections of the maxillary anterior region representing the apical one third of the maxillary incisors before (A) and after (B) anterior retraction. Notice the contact of the maxillary right central incisor and the approximation of the maxillary left central incisor roots to the incisive canal (arrow) after treatment. (C) CBCT superimposition on the cranial base before (in white) and after treatment (in black). Notice the changes in tooth position and the lateral profile following orthodontic treatment. No distinct changes were noted in the position of the incisive canal (arrow).
Therefore, the objective of this study was to evaluate the morphologic features and the relative position of the incisive canal with regard to the maxillary incisor roots using computed tomography (CT).
MATERIALS AND METHODS
Materials
The materials used for the study were retrieved from a preexisting archive of cross-sectional evaluations of adults (aged > 18) with skeletal and dental class I normal occlusion from the Institute of Craniofacial Deformity, Yonsei University (Seoul, Republic of Korea)26,27 with the approval of the institutional review board. The retrospectively retrieved materials were selected based on the following inclusion criteria: (1) the presence of clinical, lateral cephalogram, and CT images; (2) normal anteroposterior skeletal relationship (ANB of 0° to 4° and Wits appraisal of –4.0 mm to 0 mm); (3) normal overjet and overbite with class I molar and canine relationship; (4) no history of orthodontic or prosthetic treatment; and (5) no missing teeth except the third molars. Of 38 sets of materials (mean age, 21.2 ± 3.17 years), 21 were from men and 17 were from women. The average upper incisal angle to the SN plane (U1 to SN) of the subjects was 104.7° ± 5.62, indicating that the upper incisor inclination was within the normal range.
Morphologic Evaluation of the Incisive Canal and Its Proximity to the Maxillary Central Incisors
The CT images were obtained using HiSpeed Advantage (GE Medical Systems, Milwaukee, Wis) with the high-resolution bone algorithm (200 mA, 120 kV, a scanning time of 1 second) using a slice thickness of 1 mm. The CT images saved in Digital Imaging and Communication in Medicine format were analyzed using InVivoDental imaging software (version 5.2, Anatomage, San Jose, Calif). The axial plane was oriented with the Frankfort-horizontal (FH) plane as a horizontal reference plane. It was determined that the sagittal plane was perpendicular to the axial plane and parallel to the plane passing through anterior nasal spine and posterior nasal spine. Linear measurements were performed on the axial cross-sectional images corresponding to three vertical levels that were determined to exist in the sagittal plane: (1) the palatal opening of the incisive canal (opening level, L1), (2) midlevel between the opening level and the root apex of the maxillary central incisors (midlevel, L2), and (3) the root apex of the maxillary central incisors (root apex level, L3) (Figure 2A). Landmarks and measurements are defined as follows: Rm, the most medial point of the maxillary central incisor roots; Rp, the most posterior point of the maxillary central incisor roots; Cl, the most lateral point of the incisive canal; Rm-Rm, interroot distance; Rp-Rp, posterior interroot distance; Cl-Cl, canal width (Figure 2B); Ca, the most anterior point of the incisive canal; Cat, the tangent line through Ca; Rm-Cat, the distance from Rm to Cat; Rm-Canal, the distance from Rm to the anterior border of the incisive canal; Cl-Root, the distance from Cl to the posterior border of the maxillary central incisor root (Figure 2C). With regard to anteroposterior distances, the smaller value from the bilateral measurements was adopted as a representative value.
Figure 2.
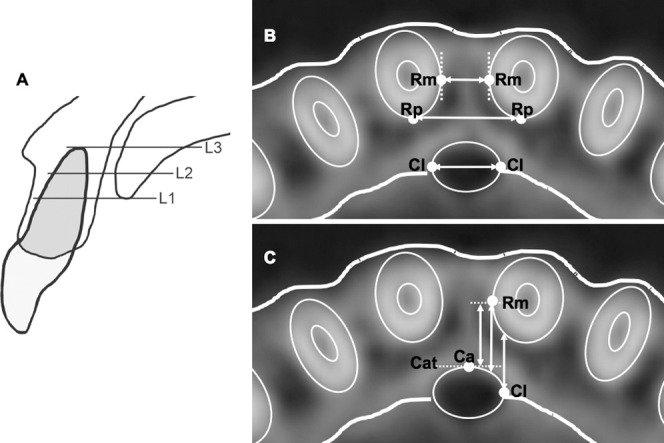
Landmarks and linear measurements. (A) Three vertical levels of the incisive canal: palatal opening level (L1), midlevel (L2), and root apex level (L3). (B) Landmarks for transverse measurements: Rm indicates the most medial point of the maxillary central incisor roots; Rp, the most posterior point of the maxillary central incisor roots; Cl, the most lateral point of the incisive canal; Rm-Rm, interroot distance; Rp-Rp, posterior interroot distance; Cl-Cl, canal width. (C) Landmarks for anteroposterior measurements: Ca indicates the most anterior point of the incisive canal; Cat, the tangent line through Ca; Rm-Cat, the distance from Rm to Cat; Rm-Canal, the distance from Rm to the anterior border of the incisive canal; Cl-Root, the distance from Cl to the posterior border of the maxillary central incisor root.
Statistical Evaluation
All measurements were made by a single examiner, who repeated them after a 2-week interval. The Dahlberg formula was used to calculate method errors:  , where d = the difference between two measurements and n = the number of measurement pairs.28 The method errors obtained ranged from 0.28 to 0.64 mm. Because the two-sample t-test showed no significant differences between men and women for any of the measurements, measurements were not divided according to gender. One-way analysis of variance followed by a Tukey test was used to investigate the influence of the differences in vertical levels. The statistical analyses were performed using SPSS 18.0 (IBM, Armonk, N.Y.), with a significance level of P < .05.
, where d = the difference between two measurements and n = the number of measurement pairs.28 The method errors obtained ranged from 0.28 to 0.64 mm. Because the two-sample t-test showed no significant differences between men and women for any of the measurements, measurements were not divided according to gender. One-way analysis of variance followed by a Tukey test was used to investigate the influence of the differences in vertical levels. The statistical analyses were performed using SPSS 18.0 (IBM, Armonk, N.Y.), with a significance level of P < .05.
RESULTS
Incisive Canal Width and Interroot Distance of the Maxillary Central Incisors
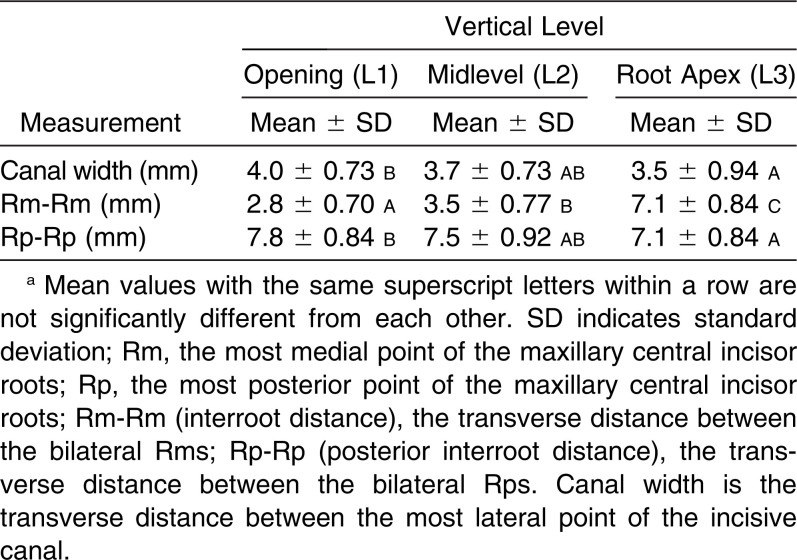
The incisive canal width (Cl-Cl) was 4.0 ± 0.73, 3.7 ± 0.73, and 3.5 ± 0.94 mm at levels L1, L2, and L3, respectively. The incisive canal width at L1 was significantly smaller than that at L3 (P < .05). Interroot distance (Rm-Rm) was 2.8 ± 0.70, 3.5 ± 0.77, and 7.1 ± 0.84 mm at levels L1, L2, and L3, respectively. Interroot distance was significantly increased from L1 to L3 (P < .05). Posterior interroot distance (Rp-Rp) was 7.8 ± 0.84, 7.5 ± 0.92, and 7.1 ± 0.84 mm at levels L1, L2, and L3, respectively. At L3, Rm and Rp represented the same point, and Rm-Rm was consequently equivalent to Rp-Rp. In contrast to Rm-Rm, Rp-Rp at L3 was significantly smaller than at L1 (P < .05) (Table 1).
Table 1.
The Incisive Canal Width and Interroot Distance of the Maxillary Central Incisors at Three Vertical Levelsa
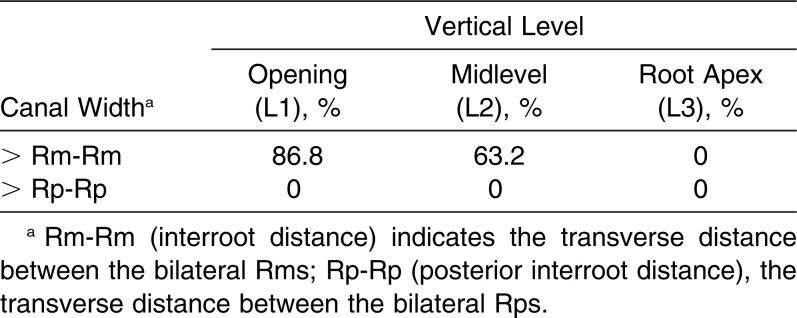
The percentage of subjects with an incisive canal width greater than the interroot distance (Rm-Rm) was 86.8% (33/38), 63.2% (24/38), and 0% (0/38) at levels L1, L2, and L3, respectively. On the other hand, the incisive canal width was smaller than Rp-Rp in all of the subjects at each vertical level (Table 2).
Table 2.
The Percentage of Patients With an Incisive Canal Width Greater Than the Interroot Distances
Proximity of the Anterior Border of the Incisive Canal to the Maxillary Central Incisor Root
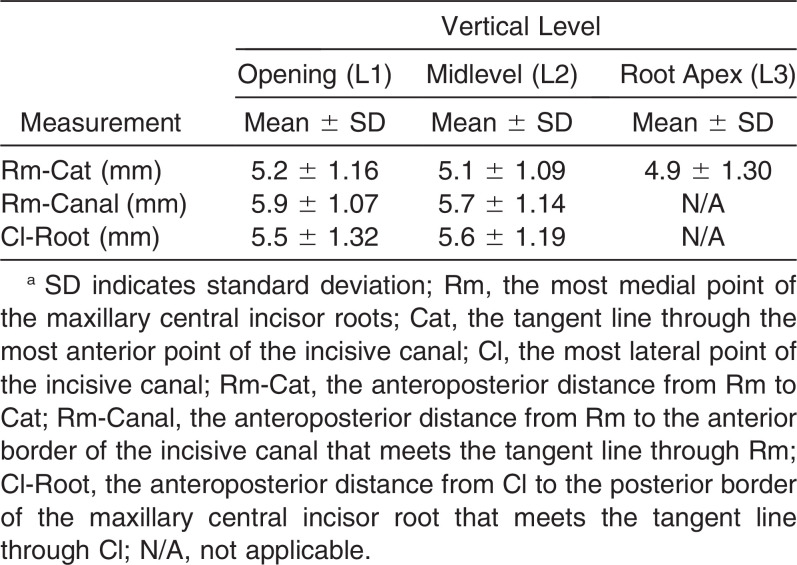
Rm-Cat was 5.2 ± 1.16, 5.1 ± 1.09, and 4.9 ± 1.30 mm at L1, L2, and L3, respectively. The measurements of Rm-Canal and Cl-Root were 5.9 ± 1.07 and 5.5 ± 1.32 mm at L1 and 5.7 ± 1.14 and 5.6 ± 1.19 mm at L2. Rm-Canal and Cl-Root were not measurable at L3 because the root apex was farther away from the median plane than was the most lateral border of the incisive canal in all subjects. Rm-Cat, Rm-Canal, and Cl-Root measurements did not show significant differences according to the vertical levels (Table 3).
Table 3.
Proximity of the Anterior Border of the Incisive Canal to the Maxillary Central Incisor Roots at Three Vertical Levelsa
DISCUSSION
Based on the “envelope of discrepancy,” the maximum amount of maxillary anterior retraction is 7 mm,11 and the recent development of skeletal anchorage has also broadened the limits of orthodontic tooth movement.29 Our results indicate that the biological anteroposterior distances between the maxillary central incisor roots and the incisive canal were approximately 5–6 mm, slightly less than our conventional guidelines. This 5- to 6-mm distance does not necessarily imply the “safety zone” for retraction because individuals with relatively large interroot distances are not at risk of canal invasion or contact even following maximum retraction. However, more than 60% of our subject pool had an incisive canal width larger than the interroot distance, and individual variations of canal dimension, especially enlargement and asymmetry of the canal morphology, are frequently reported with 3D evaluation.20,21,30,31
Anatomical features of the incisive canal have been studied in connection with rehabilitation of the maxillary anterior region18–24 and the placement of orthodontic mini-implants.30,32–34 However, the consequences or the possibilities of incisor roots being in contact with the incisive canal following tooth movement are poorly documented in the orthodontic literature. Similar to the example presented in Figure 1, it was recently noted through 3D evaluation that the maxillary central incisor root in direct contact with the incisive canal following anterior retraction was associated with severe root resorption, but without any neurologic symptoms.25 Given that the incisive canal is surrounded by thick cortical bone, similar reactions may be induced when the roots are in contact with the lingual cortical plate. Contact of tooth roots with the cortical plate has been addressed as a contributor to root resorption,12–14,16 result in delayed tooth movement,12 and may also cause perforation and dehiscence of the cortical plate.6,9,10,12,15 In this context, it is interesting to note that the incidence of orthodontic root resorption is by far more frequent in the maxillary central incisors, even with their larger tooth dimensions, than in the lateral incisors.14,35
Considering the morphologic dimensions of the central incisor roots and the incisive canal, the posterior-median aspect of the apical third (L1 or L2 levels) of the roots rather than the root apex per se is most likely to approximate with the canal following maxillary anterior retraction and root movement. However, in many clinical situations anterior intrusion also occurs during the retraction process, raising the possibility of approximation along the path of tooth movement. It is also noteworthy that in the mandibular canal, temporary paresthesia of the lower lip was reported in association with tooth root when in contact with the canal wall following orthodontic tooth movement.36,37 Thus, 3D images may be helpful in estimating the proximity of the incisive canal along with the dimensional characteristics when a considerable amount of maxillary incisor retraction with vertical control is planned.
Tooth movement induces remodeling of the surrounding bone. Although remodeling of the incisive canal following orthodontic tooth movement has not, to our knowledge, been reported,25 relative changes in the position of the incisive canal because of changes in the surrounding alveolar bone following tooth loss have been noted in the edentulous dentition.22,38 Therefore, to determine the remodeling potential of the incisive canal wall following orthodontic tooth movement, further evaluations using comparisons of pre- and posttreatment materials are necessary.
CONCLUSIONS
The anteroposterior distance between the maxillary central incisor roots and the incisive canal was approximately 5–6 mm.
More than 60% of subjects had an incisive canal width greater than the interroot distance.
Evaluation of the proximity of the incisive canal to the maxillary incisors, in addition to its dimensional characteristics, may be helpful when a considerable amount of maxillary retraction is planned.
ACKNOWLEDGMENT
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2013R1A1A3011648). The authors declare no conflicts of interest related to this study.
REFERENCES
- 1.Riedel RA. Esthetics and its relation to orthodontic therapy. Angle Orthod. 1950;20:168–178. doi: 10.1043/0003-3219(1950)020<0168:EAIRTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Rains MD, Nanda R. Soft-tissue changes associated with maxillary incisor retraction. Am J Orthod. 1982;81:481–488. doi: 10.1016/0002-9416(82)90427-4. [DOI] [PubMed] [Google Scholar]
- 3.Arnett GW, Bergman RT. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am J Orthod. 1993;103:299–312. doi: 10.1016/0889-5406(93)70010-L. [DOI] [PubMed] [Google Scholar]
- 4.Kokich V. Esthetics and anterior tooth position: an orthodontic perspective part III: mediolateral relationships. J Esthet Restor Dent. 1993;5:200–207. doi: 10.1111/j.1708-8240.1993.tb00781.x. [DOI] [PubMed] [Google Scholar]
- 5.Sarver DM. The importance of incisor positioning in the esthetic smile: the smile arc. Am J Orthod. 2001;120:98–111. doi: 10.1067/mod.2001.114301. [DOI] [PubMed] [Google Scholar]
- 6.Wennstrom JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol. 1987;14:121–129. doi: 10.1111/j.1600-051x.1987.tb00954.x. [DOI] [PubMed] [Google Scholar]
- 7.Proffit WR, White RP., Jr Who needs surgical-orthodontic treatment. Int J Adult Orthodon Orthognath Surg. 1990;5:81–89. [PubMed] [Google Scholar]
- 8.Ackerman JL, Proffit WR. Soft tissue limitations in orthodontics: treatment planning guidelines. Angle Orthod. 1997;67:327–336. doi: 10.1043/0003-3219(1997)067<0327:STLIOT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Vardimon AD, Oren E, Ben-Bassat Y. Cortical bone remodeling/tooth movement ratio during maxillary incisor retraction with tip versus torque movements. Am J Orthod Dentofacial Orthop. 1998;114:520–529. doi: 10.1016/s0889-5406(98)70172-6. [DOI] [PubMed] [Google Scholar]
- 10.Re S, Cardaropoli D, Corrente G, Abundo R. Bodily tooth movement through the maxillary sinus with implant anchorage for single tooth replacement. Clin Orthod Res. 2001;4:177–181. doi: 10.1034/j.1600-0544.2001.040308.x. [DOI] [PubMed] [Google Scholar]
- 11.Ackerman JL, Proffit WR. Diagnosis and treatment planning. In: Graber TM, Swain BF, editors. Current Orthodontic Concepts and Techniques. St. Louis, Mo: Mosby; 1982. pp. 3–100. [Google Scholar]
- 12.Wainwright WM. Faciolingual tooth movement: its influence on the root and cortical plate. Am J Orthod. 1973;64:278–302. doi: 10.1016/0002-9416(73)90021-3. [DOI] [PubMed] [Google Scholar]
- 13.Ten Hoeve A, Mulie RM. The effect of antero-postero incisor repositioning on the palatal cortex as studied with laminagraphy. J Clin Orthod. 1976;10:804–822. [PubMed] [Google Scholar]
- 14.Kaley J, Phillips C. Factors related to root resorption in edgewise practice. Angle Orthod. 1991;61:125–132. doi: 10.1043/0003-3219(1991)061<0125:FRTRRI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Handelman CS. The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996;66:95–110. doi: 10.1043/0003-3219(1996)066<0095:TAAIII>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Horiuchi A, Hotokezaka H, Kobayashi K. Correlation between cortical plate proximity and apical root resorption. Am J Orthod. 1998;114:311–318. doi: 10.1016/s0889-5406(98)70214-8. [DOI] [PubMed] [Google Scholar]
- 17.Jacob S, Zelano B, Gungor A, Abbott D, Naclerio R, McClintock MK. Location and gross morphology of the nasopalatine duct in human adults. Arch Otolaryngol Head Neck Surg. 2000;126:741–748. doi: 10.1001/archotol.126.6.741. [DOI] [PubMed] [Google Scholar]
- 18.Kim GT, Hwang EH, Lee SR. A study of incisive canal using a cone beam computed tomography. Korean J Oral Maxillofac Radiol. 2004;34:7–12. [Google Scholar]
- 19.Mraiwa N, Jacobs R, Van Cleynenbreugel J, Sanderink G, Schutyser F, Suetens P, van Steenberghe D, Quirynen M. The nasopalatine canal revisited using 2D and 3D CT imaging. Dentomaxillofac Radiol. 2004;33:396–402. doi: 10.1259/dmfr/53801969. [DOI] [PubMed] [Google Scholar]
- 20.Liang X, Jacobs R, Martens W, Hu Y, Adriaensens P, Quirynen M, Lambrichts I. Macro- and micro-anatomical, histological and computed tomography scan characterization of the nasopalatine canal. J Clin Periodontol. 2009;36:598–603. doi: 10.1111/j.1600-051X.2009.01429.x. [DOI] [PubMed] [Google Scholar]
- 21.Song WC, Jo DI, Lee JY, et al. Microanatomy of the incisive canal using three-dimensional reconstruction of microCT images: an ex vivo study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:583–590. doi: 10.1016/j.tripleo.2009.06.036. [DOI] [PubMed] [Google Scholar]
- 22.Thakur AR, Burde K, Guttal K, Naikmasur VG. Anatomy and morphology of the nasopalatine canal using cone-beam computed tomography. Imaging Sci Dent. 2013;43:273–281. doi: 10.5624/isd.2013.43.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Artzi Z, Nemcovsky CE, Bitlitum I, Segal P. Displacement of the incisive foramen in conjunction with implant placement in the anterior maxilla without jeopardizing vitality of nasopalatine nerve and vessels: a novel surgical approach. Clin Oral Implants Res. 2000;11:505–510. doi: 10.1034/j.1600-0501.2000.011005505.x. [DOI] [PubMed] [Google Scholar]
- 24.Kraut RA, Boyden DK. Location of incisive canal in relation to central incisor implants. Implant Dent. 1998;7:221–225. doi: 10.1097/00008505-199807030-00010. [DOI] [PubMed] [Google Scholar]
- 25.Chung CJ, Choi YJ, Kim KH. Approximation and contact of the maxillary central incisor roots with the incisive canal after maximum retraction with temporary anchorage devices: report of two cases. Am J Orthod Dentofacial Orthop. 2015;148:493–502. doi: 10.1016/j.ajodo.2015.04.033. [DOI] [PubMed] [Google Scholar]
- 26.Kim SJ, Choi TH, Baik HS, Park YC, Lee KJ. Mandibular posterior anatomic limit for molar distalization. Am J Orthod Dentofacial Orthop. 2014;146:190–197. doi: 10.1016/j.ajodo.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 27.Lee KJ, Joo E, Kim KD, Lee JS, Park YC, Yu HS. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am J Orthod Dentofacial Orthop. 2009;135:486–494. doi: 10.1016/j.ajodo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 28.Houston W. The analysis of errors in orthodontic measurements. Am J Orthod. 1983;83:382–390. doi: 10.1016/0002-9416(83)90322-6. [DOI] [PubMed] [Google Scholar]
- 29.Graber LW, Vanarsdall RL, Vig KW. Orthodontics Current Principles and Techniques. Philadelphia, Pa: Elsevier; 2011. pp. 46–54. 5th ed. [Google Scholar]
- 30.Kim SJ, Lim SH. Anatomic study of the incisive canal in relation to midpalatal placement of mini-implant. Korean J Orthod. 2009;39:146–158. [Google Scholar]
- 31.Asaumi R, Kawai T, Sato I, Yoshida S, Yosue T. Three-dimensional observations of the incisive canal and the surrounding bone using cone-beam computed tomography. Oral Radiol. 2010;26:20–28. [Google Scholar]
- 32.Bernhart T, Vollgruber A, Gahleitner A, Dortbudak O, Haas R. Alternative to the median region of the palate for placement of an orthodontic implant. Clin Oral Implants Res. 2000;11:595–601. doi: 10.1034/j.1600-0501.2000.011006595.x. [DOI] [PubMed] [Google Scholar]
- 33.Henriksen B, Bavitz B, Kelly B, Harn SD. Evaluation of bone thickness in the anterior hard palate relative to midsagittal orthodontic implants. Int J Oral Maxillofac Implants. 2003;18:578–581. [PubMed] [Google Scholar]
- 34.Schlegel KA, Kinner F, Schlegel KD. The anatomic basis for palatal implants in orthodontics. Int J Adult Orthodon Orthognath Surg. 2002;17:133–139. [PubMed] [Google Scholar]
- 35.Segal GR, Schiffman PH, Tuncay OC. Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofac Res. 2004;7:71–78. doi: 10.1111/j.1601-6343.2004.00286.x. [DOI] [PubMed] [Google Scholar]
- 36.Krogstad O, Omland G. Temporary paresthesia of the lower lip: a complication of orthodontic treatment. A case report. Br J Orthod. 1997;24:13–15. doi: 10.1093/ortho/24.1.13. [DOI] [PubMed] [Google Scholar]
- 37.Farronato G, Garagiola U, Farronato D, Bolzoni L, Parazzoli E. Temporary lip paresthesia during orthodontic molar distalization: report of a case. Am J Orthod Dentofacial Orthop. 2008;133:898–901. doi: 10.1016/j.ajodo.2006.09.051. [DOI] [PubMed] [Google Scholar]
- 38.Mardinger O, Namani-Sadan N, Chaushu G, Schwartz-Arad D. Morphologic changes of the nasopalatine canal related to dental implantation: a radiologic study in different degrees of absorbed maxillae. J Periodontol. 2008;79:1659–1662. doi: 10.1902/jop.2008.080043. [DOI] [PubMed] [Google Scholar]