Fig. 2.
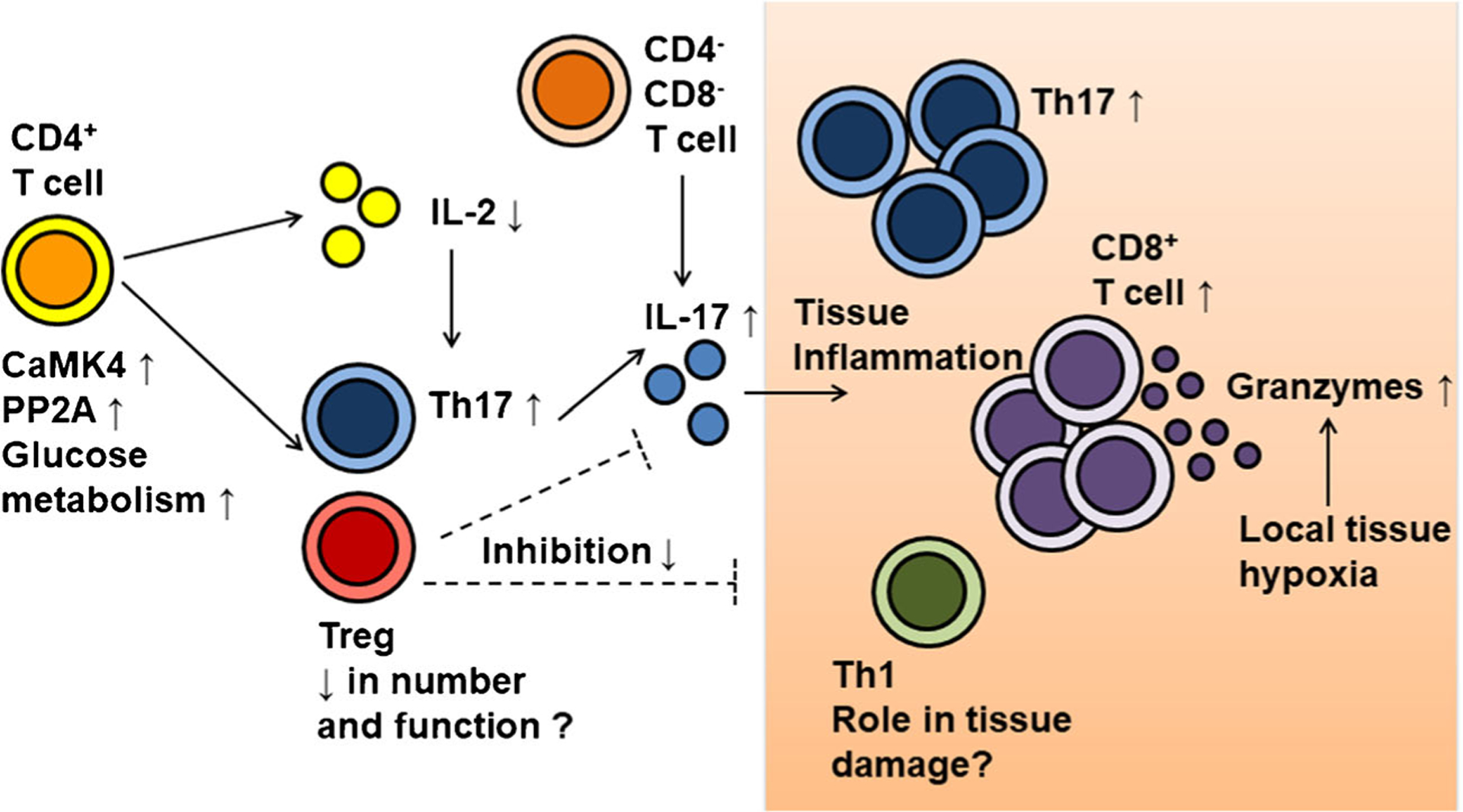
Dysregulated T cell subset distribution and function involved in driving lupus pathogenesis. Abnormality of CD4+ function and signaling, including increased calcium/calmodulin-dependent protein kinase IV (CaMK4), serine/threonine protein phosphatase 2A (PP2A), and glucose metabolism, cause reduction in IL-2 production and the imbalance of Th17/ regulatory T cells (Treg). Reduction of Treg numbers and function may partly play a role in lupus pathogenesis through inadequate suppression of systemic and tissue inflammation. Meanwhile, increased IL-17 production by Th17 and CD4− CD8− double-negative T cells contributes to tissue inflammation. Increased numbers of Th17 and CD8+ T cells indicate their pathogenic roles, and increased effector function of tissue-infiltrating T cells may be caused of local factors, such as hypoxia
