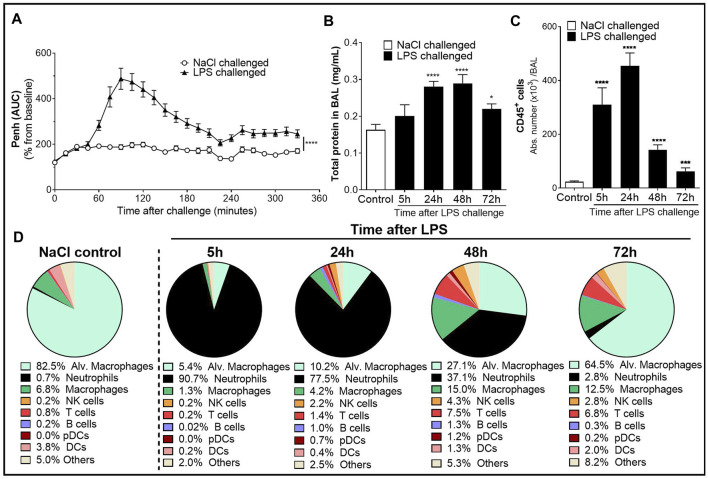
FIGURE 1.
Characterization of the lipopolysaccharide (LPS)-induced acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) model in male DBA/1 mice. LPS inhalation was associated with a significant breathing pattern alteration (A), an increase in alveolar–capillary barrier permeability (B), and increased immune cell infiltrates in the bronchoalveolar space (C, D) compared with NaCl-exposed mice (control mice). (A) Breathing pattern alteration was measured by the change in the calculated enhanced pause (Penh) using whole-body plethysmography in conscious unrestrained mice over a period of 6 h following LPS (black triangles) or NaCl inhalation (white circles). Results are expressed as the mean percentage Penh area under the curve (AUC) normalized to the baseline ± SEM (n = 16 mice per group). ****p < 0.0001 paired Student t-test. (B) Alveolar–capillary barrier permeability was assessed by measuring the total protein concentration in the bronchoalveolar lavage (BAL) supernatant at 5, 24, 48, and 72 h after LPS challenge (black bars, n = 7–16 mice per time point) or NaCl challenge (control mice, white bar, n = 20; all time points were pooled). Results are expressed as mean ± SEM. *p < 0.05, ****p < 0.0001 paired Student t-test. (C) Time course of CD45+ immune cells in the BAL measured by flow cytometry in samples collected at 5, 24, 48, and 72 h after LPS challenge (black bars, n = 7–16 mice per time point) or NaCl challenge (control mice, white bar, n = 20; all time points were pooled). Results are expressed as mean ± SEM. ***p < 0.001, ****p < 0.0001 paired Student t-test. (D) Frequencies of BAL immune cell populations over time. Results are expressed as proportions among total CD45+ cells for each time point.