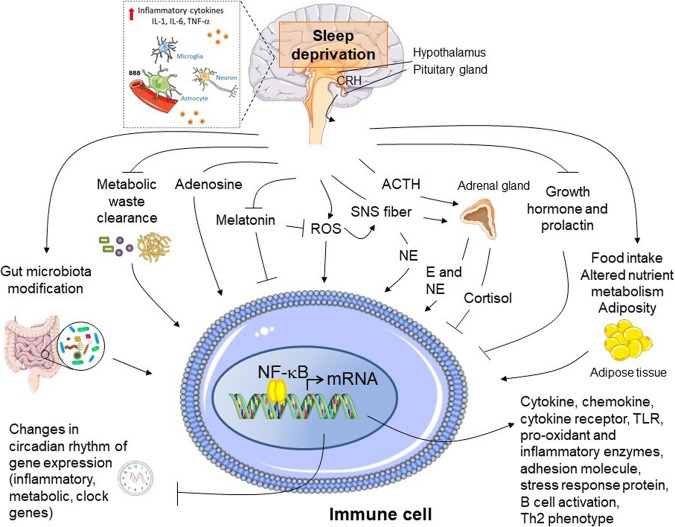
Fig. 3. Pro-inflammatory molecular pathways induced by sleep deprivation.
A schematic model of potential mechanistic pathways linking sleep deprivation and inflammatory immune activation is depicted. Sleep deprivation is associated with activation of the sympathetic nervous system and release of norepinephrine and epinephrine into the systemic circulation, as well as to some extent with impaired hypothalamus-pituitary axis stimulation. These neuromediators may act along with other potential stimuli accumulated following sleep deprivation including reactive oxygen species (ROS), adenosine, metabolic waste products (e.g., β-amyloid) not cleared during normal sleep, gut microbiota dysbiosis leading to altered local and systemic pattern of metabolic products, as well as with changes in the profile of neuro-endocrine hormones, such as prolactin, growth hormone, and altered circadian rhythm of melatonin secretion. In immune cells located in the brain and the peripheral tissues, these stimuli may in concert trigger inflammatory activation, with release of cytokines, chemokines, acute phase protein, etc. via the recruitment of transcriptional regulators of pro-inflammatory gene expression, mainly nuclear factor (NF)-κB, and disturbing the circadian rhythmicity of gene expression of both clock genes and metabolic, immune and stress response genes (see text for further detail). E: epinephrine; NE: norepinephrine; TLR: Toll-like receptor. Arrows indicate stimulation; lines indicate inhibition. The illustrations were modified from Servier Medical Art (http://smart.servier.com/), licensed under a Creative Common Attribution 3.0 Generic License.