Abstract
Purpose
Telehealth may remain an integral part of cancer survivorship care after the SARS-CoV-2 pandemic. While telehealth may reduce travel/waiting times and costs for many patients, it may also create new barriers that could exacerbate care disparities in historically underserved populations, manifesting as differences in overall care participation, and in differential video versus phone use for telehealth.
Methods
We reviewed visits by cancer survivors between January and December 2020 at a designated cancer center in Minnesota. We used descriptive statistics, data visualization, and generalized estimating equation logistic regression models to compare visit modalities and trends over time by age, urban/rural status, and race/ethnicity.
Results
Among 159,301 visits, including 33,242 telehealth visits, older and rural-dwelling individuals were underrepresented in telehealth compared with in-person care. Non-Hispanic White individuals, those aged 18–69 years, and urban residents used video for > 50% of their telehealth visits. In contrast, those aged ≥ 70 years, rural residents, and most patient groups of color used video for only 33–43% of their telehealth visits. Video use increased with time for everyone, but relative differences in telehealth modalities persisted. Visits of Black/African American patients temporarily fell in spring/summer 2020.
Conclusions
Our findings underscore reduced uptake of telehealth, especially video, among potentially vulnerable patient populations. Future research should evaluate reasons for differential telehealth utilization and whether visit modality (in-person versus video versus phone) affects cancer outcomes.
Implications for Cancer Survivors
A long-term cancer care model with integrated telehealth elements needs to account for specific barriers for vulnerable populations.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11764-021-01133-4.
Keywords: Telehealth, Telemedicine, Cancer care disparities, Cancer care during COVID-19, Phone and video use for telehealth
Introduction
During the SARS-CoV-2 pandemic, cancer healthcare rapidly transitioned towards reliance on telehealth as the default so as to minimize risk of SARS-CoV-2 infection for patients and providers. This rapid shift may have simplified care logistics and improved care convenience for many patients — for example by reducing travel and waiting times, and costs for gas and lodging for those who previously had to travel long distances to receive care [1]. At the same time, it is also possible that telehealth inadvertently exacerbated existing disparities in healthcare for some vulnerable populations — for example, because of technological barriers, insufficient internet connectivity, privacy concerns about the technology and in home settings, or because some patients may be uncomfortable using video in a telehealth appointment for other reasons [2, 3].
Telehealth has been promoted as promising tool in cancer survivorship since before the SARS-CoV-2 pandemic [4], but only during the pandemic was telehealth widely and rapidly implemented [5]. The budding literature on early experiences with telehealth during the pandemic emphasized that patients had an overall positive view of and were satisfied with telehealth [6–8]. Nevertheless, it is possible that early positive perceptions of telehealth were in part attributable to patients’ greater flexibility and tolerance to change in the early pandemic. Since then, patients may have grown weary of the multiple and long-term burdens the pandemic may have created in their everyday lives. For example, social isolation, potential losses of jobs and income, and complicated situations at home while in lockdown may have increased frustration and lowered patients’ acceptance of telehealth which was widely implemented because of the SARS-CoV-2 pandemic [9]. Additionally, acceptance of telehealth does not necessarily equate preference. For example, one study in otolaryngology found that while nearly 90% of patients had favorable views of telehealth during the pandemic, less than 50% reported they would continue telehealth post-pandemic [10].
In addition to attitudes towards telehealth, social determinants may play a role in the general uptake of telehealth, and in the use of different telehealth modalities (video versus phone). Recent studies on general medical encounters during the SARS-CoV-2 pandemic have suggested differences in use of telehealth by sex, age, income, type of insurance, and race/ethnicity [11–17]. These studies underscore the possibility that telehealth may increase health care disparities among historically marginalized population groups. Differences in uptake of telehealth could express in several forms — as non-participation in telehealth, and as differential use of video versus phone among those who participate in telehealth.
Understanding differences in the uptake of telehealth is crucial as we move towards a care model in which telehealth will likely continue in some format even after the pandemic. We examined utilization of telehealth and other visits in cancer survivors at a designated comprehensive cancer center in Minnesota between January and December 2020 among various subgroups of patients. Our objective was to describe mode of healthcare visits among cancer survivors seeking care and to identify possible differences in the uptake of telehealth. We hypothesized that vulnerable and historically marginalized patient populations (rural, older, and Black, indigenous, or persons of color [BIPOC]) less often participated in telehealth visits, and in video compared with phone telehealth visits specifically.
Methods
Data source and identification of cancer survivors
The University of Minnesota Institutional Review Board approved this retrospective study. We reviewed electronic medical records (EMR) of visits that occurred among the cancer clinics of the University of Minnesota Masonic Cancer Center (MCC) between January and December 2020. Study participants were identified as individuals aged 18 or older with a primary cancer diagnosis who received care at the MCC and had consented to have their medical records reviewed for research purposes (~ 95% of patients). Cancer survivors were defined from the time of diagnosis. We excluded individuals with in situ diagnoses, except for in situ breast cancer, and we restricted our analyses to visits with a “completed” appointment status. Cancer treatment visits for chemotherapy, radiation, surgery, etc. were carried out in person, and not via telehealth, even during the SARS-CoV-2 pandemic. Therefore, in the comparison of telehealth utilization modes (video vs. phone), such cancer treatment visits were automatically excluded, resulting in an implicit focus on follow-up care.
Measures
Our primary outcome of interest was visit type (in-person, telehealth) and mode of telehealth visit (video, phone). We identified telehealth visits by the visit type field in the EMR: if the visit type mentioned “video” or “telephone”, the visit was classified accordingly; otherwise, the visit was evaluated as in-person visit. Our primary exposures of interest were age at time of visit (years, included as cubic age splines in the adjusted regression model), urban versus rural residence defined by residential ZIP code–based rural/urban commuting area (RUCA) codes (RUCA categorization C) [18], patients’ race and/or ethnicity (American Indian/American Native [AIAN], Asian, Non-Hispanic Black/African American [NH Black/AA], Hispanic, Multiple, Native Hawaiian/Pacific Islander [NHPI], NH White), and biological sex (female, male; self-identified gender was unavailable). We additionally adjusted for cancer diagnosis (breast, lung, gastrointestinal, gynecologic, other solid tumor, hematologic, multiple cancers). We classified cancer diagnoses based on ICD-10 codes abstracted from the EMR and based on SEER ICD-10 code categories [19].
Statistical analysis
Descriptive statistics and data visualization were used to describe visit mode and trends in visits over time. Visits from January to December 2020 were used for cross-sectional descriptive analysis and adjusted regression, but we visualized the monthly data to detect potential trends between March and December 2020. We used generalized estimating equation (GEE) logistic regression models to compare video versus phone visits by age, urban/rural status, and race/ethnicity, additionally adjusting for sex and cancer diagnosis. We clustered 2020 visits by patient in the GEE regression assuming an exchangeable correlation structure (compound symmetry) in the variance in order to account for dependence because some patients had multiple visits in 2020. We did not run a regression model to estimate in-person care versus overall telehealth participation for the following reasons: first, during this time period, video visits were the default unless requested for a particular necessitating reason. However, we were not able to discern specific reasons for the visit type chosen. For example, we were unable to determine if any visits that could theoretically have been done using telehealth were scheduled as in-person visits because a patient specifically requested in-person over telehealth care. Second, visits that were not scheduled because patients were unable to participate in any kind of telehealth at that time for any reason were not captured. We report odds ratios (OR) of video compared with phone use for a telehealth visit, and corresponding 95% confidence intervals (CI). P values < 0.05 were considered statistically significant. Analyses were conducted in SAS 9.4 and R using the splines, geepack, ggplot2, and egg packages.
Results
Over the study period, 159,301 visits were completed by 14,396 cancer survivors at the MCC between January and December 2020, including 33,242 telehealth visits by 10,620 cancer survivors between March and December 2020. Mean patient age at visit was 63.2 ± 13.8 years (62.6 ± 13.7 years in those with at least one telehealth visit; Table 1); 59% were female; 85% lived in urban areas; 91% of patients were NH White, 4% NH Black/AA, 3% Asian, 1.4% Hispanic, 0.7% AIAN, 0.3% of multiple races, and 0.1% NHPI. The most frequent aggregated cancer categories were hematologic (24%) and breast (23%). A small number of patients (10%) had more than one cancer diagnosis documented. Differences between the telehealth cohort versus all patients were small except for the proportion of rural residents (11% in those with at least one telehealth visit versus 15% in the overall patient population).
Table 1.
Demographic and clinical characteristics of patients who used telehealth between March and December 2020, University of Minnesota Masonic Cancer Center
| Patient characteristic | Patients with at least one telehealth appointment, N = 10,620 | All patients, N = 14,396 | ||
|---|---|---|---|---|
| N | % | N | % | |
| Age group | ||||
| 18–49 years | 1707 | 16.1 | 34 | 15.5 |
| 50–69 years | 5363 | 50.5 | 7152 | 49.7 |
| ≥ 70 years | 3550 | 33.4 | 4010 | 34.8 |
| Sex | ||||
| Female | 6312 | 59.5 | 8473 | 58.9 |
| Male | 4308 | 40.5 | 5923 | 41.1 |
| Race/ethnicity | ||||
| American Indian/Alaska Native | 76 | 0.7 | 98 | 0.7 |
| Asian | 308 | 3.0 | 383 | 2.8 |
| Non-Hispanic Black/African American | 438 | 4.3 | 580 | 4.2 |
| Hispanic | 147 | 1.4 | 196 | 1.4 |
| Native Hawaiian/Pacific Islander | 12 | 0.1 | 16 | 0.1 |
| Non-Hispanic White | 9255 | 90.1 | 12,568 | 90.6 |
| Multiple | 30 | 0.3 | 36 | 0.3 |
| Residence | ||||
| Rural | 1201 | 11.4 | 2096 | 14.6 |
| Urban | 9379 | 88.7 | 12,223 | 85.4 |
| Primary cancer site | ||||
| Breast | 2417 | 22.8 | 3256 | 22.6 |
| Gastrointestinal | 941 | 8.9 | 1264 | 8.8 |
| Gynecologic | 900 | 8.5 | 1317 | 9.2 |
| Hematologic | 2528 | 23.8 | 3430 | 23.8 |
| Lung | 595 | 5.6 | 823 | 5.7 |
| Other solid | 2043 | 19.2 | 2934 | 20.4 |
| Multiple | 1196 | 11.3 | 1372 | 9.5 |
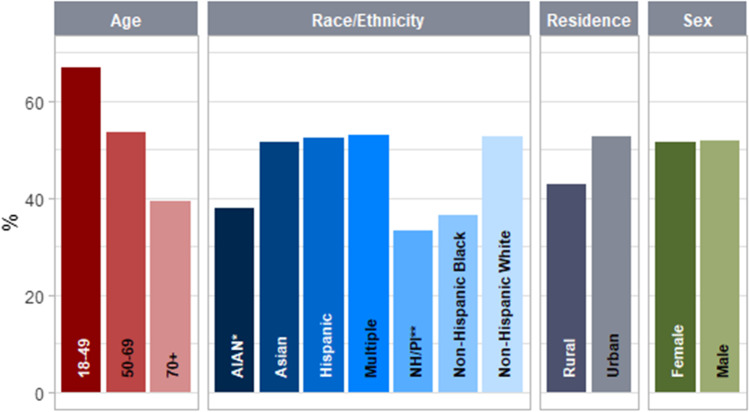
In our assessment of video versus phone use for telehealth, the proportion of video use among telehealth visits varied (Fig. 1 and Table 2): video visits accounted for more than 50% of all telehealth visits among Asian, Hispanic, NH White individuals, and among those with multiple ancestral backgrounds, but only for about one-third of all telehealth visits among AIAN (versus NH White, adjusted OR 0.55, 95% CI 0.35–0.85), Black/AA (versus NH White, OR 0.43, 95% CI 0.36–0.51), and NH/PI individuals (versus NH White, adjusted OR 0.55, 95% CI range 0.30–1.03). Video use was furthermore less common among older individuals, with approximately two thirds of all telehealth visits on video among those aged 18–49, but less often among those aged 50 or older, and rarest among those aged 70 or older (39%). We found no evidence for differences in video use by sex. In the adjusted logistic regression, increasing age, modeled as cubic splines, was non-linearly associated with less frequent video use (P < 0.0001): the decline in video use grew steeper as age increased (Supplemental Fig. 1). Video use was less common among rural (43%) than urban (53%) residents. We tested for interaction between residential status and sex (P = 0.29), and between residential status and age (P = 0.0009): the association between rural residency and less video use was stronger among those who were younger; and the association between being older and less video use was stronger among those living in urban than in rural areas (Table 2 and Supplemental Fig. 6). The adjusted analysis also revealed variation in video use by cancer categories: visits by patients with gynecologic, hematologic, lung, or multiple cancers were less likely to be on video than visits by patients with breast cancer (OR range 0.41–0.79, 95% CI range 0.36–0.89). Across all groups, the share of video versus phone use for telehealth continued to increase through December, but the observed relative differences by age, rurality, and race/ethnicity remained consistent despite overall increasing video use (Supplemental Fig. 3).
Fig. 1.
Share (%) of video among all telehealth visits March–December 2020 for different population groups, University of Minnesota Masonic Cancer Center. *American Indian/Alaska Native, **Native Hawaiian/Pacific Islander
Table 2.
Multivariate GEE logistic regression: adjusted odds ratios of video (versus phone) use for telehealth between March and December 2020, N = 33,242 visits, University of Minnesota Masonic Cancer Center
| Parameter | Odds ratio | 95% confidence interval | P | |
|---|---|---|---|---|
| Age (modeled as cubic splines; by residential status) | < 0.0001 | |||
| Urban: Age 63 versus 54 (median versus 25th percentile) | 0.73 | 0.67 | 0.79 | < .0001 |
| Rural: Age 63 versus 54 | 1.07 | 0.85 | 1.35 | 0.57 |
| Urban: Age 71 versus 63 (75th percentile versus median) | 0.73 | 0.67 | 0.80 | < .0001 |
| Rural: Age 71 versus 63 | 0.77 | 0.59 | 1.00 | 0.05 |
| Race/ethnicity | ||||
| American Indian/Alaska Native | 0.54 | 0.35 | 0.83 | 0.005 |
| Asian | 0.69 | 0.56 | 0.84 | 0.0003 |
| Non-Hispanic Black/African American | 0.42 | 0.36 | 0.51 | < .0001 |
| Hispanic | 0.71 | 0.54 | 0.94 | 0.02 |
| Native Hawaiian/Other Pacific Islander | 0.55 | 0.29 | 1.03 | 0.06 |
| Multiple | 0.60 | 0.35 | 1.03 | 0.09 |
| Non-Hispanic White | 1 (Ref.) | |||
| Residence (at different ages) | ||||
| Rural versus urban, at age 54 | 0.43 | 0.35 | 0.53 | < .0001 |
| Rural versus urban, at age 63 | 0.64 | 0.52 | 0.78 | < .0001 |
| Rural versus urban, at age 71 | 0.67 | 0.54 | 0.82 | 0.0001 |
| Sex | ||||
| Male | 1.04 | 0.95 | 1.13 | 0.43 |
| Female | 1 (Ref.) | |||
| Cancer type | ||||
| Gastrointestinal | 0.97 | 0.84 | 1.11 | 0.64 |
| Gynecologic | 0.41 | 0.36 | 0.48 | < .0001 |
| Hematologic | 0.76 | 0.68 | 0.85 | < .0001 |
| Lung | 0.66 | 0.56 | 0.78 | < .0001 |
| Multiple cancer diagnoses | 0.79 | 0.70 | 0.90 | 0.0003 |
| Other solid tumor | 0.90 | 0.80 | 1.03 | 0.12 |
| Breast | 1 (Ref.) | |||
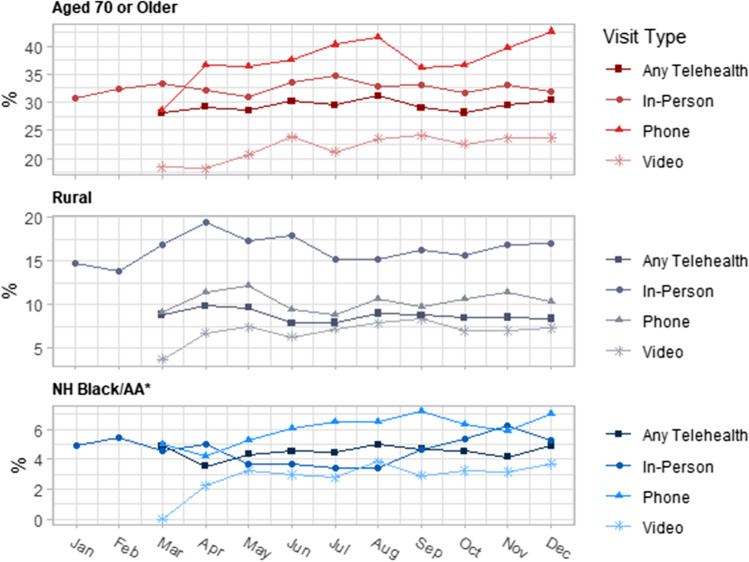
We visualized the total number of completed visits and of cancellations over time (Supplemental Figs. 4 and 5), and the relative share of different population groups in any kind of telehealth versus in-person visits versus video versus phone visits over time (Fig. 2 and Supplemental Fig. 2). This analysis (Fig. 2) was restricted to those we hypothesized to be most vulnerable to potential disparities (those aged ≥ 70, rural, or Black/AA; a meaningful depiction of other BIPOC groups was not possible due to small monthly sample sizes). We did not observe a time trend in the number of completed visits or cancellations over time except for a temporary uptick in cancellations in March 2020 when the pandemic took hold in the USA. We found that the relative proportion of those aged ≥ 70 was smaller among video visits than this group’s relative proportion among in-person visits; however, this group’s relative proportion among phone visits was higher (Fig. 2). In contrast, among rural residents, relative proportions in phone and video visits were similar, but both substantially lower than this group’s relative participation among in-person visits. The highest relative proportion of NH Black/AA patients was among phone visits; additionally, NH Black/AA patients’ relative proportion among in-person visits, and to a lesser degree among video visits, as well as the total number of completed visits by NH Black/AA patients temporarily fell in spring/summer 2020.
Fig. 2.
Shares (%) in visits by selected vulnerable population groups over time in 2020, by type of visit, University of Minnesota Masonic Cancer Center. *Non-Hispanic Black/African American
Discussion
Our findings underscore differences in the uptake of video compared to phone use among cancer survivors seeking cancer care and who utilized telehealth, as well as in the uptake of any kind of telehealth compared with in-person care. Older (compared with younger) and rural (versus urban) individuals used telehealth less often than in-person care. Older, rural, and BIPOC patient populations used phone (versus video) for telehealth more often than younger, urban, and White patients. Video use for telehealth increased with time in all patient groups, but relative differences in video versus phone use persisted.
Our study confirms previous studies that reported sociodemographic disparities in the uptake of telehealth early during the pandemic [11–13, 20] and emphasizes that these disparities may have persisted even as telehealth was no longer a novelty in cancer care. Telehealth facilitated the continuity of care while minimizing risk of SARS-CoV-2 infection [21, 22], and perhaps made healthcare more convenient for many by reducing costs and care logistics [7]. However, potential barriers to telehealth need to be addressed as telehealth is integrated into a long-term cancer care model. These barriers are likely not equally distributed in the population and may differ by telehealth modality, due to factors such as appropriate internet access, the digital divide, differing comfort levels with technology, and other unique patient situations.
One compelling finding of this study is that the relative participation of rural (compared with urban) patients in any kind of telehealth was lower than their relative participation among in-person care. This finding is relevant since telehealth has been previously described as one potential approach to mitigate rural healthcare shortages that exist independently of the SARS-CoV-2 pandemic, and to improve care logistics, for example travel times [23, 24]. Our findings suggest telehealth barriers disproportionally affect rural patients. We do not know if these barriers exist at the patient and/or provider level. While internet access may play a role for this discrepancy, broadband access in rural Minnesota tends to be better than in many other states [25, 26]. Hence, a rural healthcare model which incorporates elements of telehealth may improve access to care for some but not all rural patient populations, and future research should assess barriers to telehealth among individuals living in rural areas.
Similarly, we saw some disparities in participation in any kind of telehealth compared with in-person care in those aged ≥ 70. But unlike for rural patients where participation differences were largest between in-person and any kind of telehealth, for the oldest patient group, the largest participation differences were between video and phone use for telehealth. This finding suggests that video technology or appropriate internet access to enable video visits, or general comfort with video visits, may be a concern in those aged ≥ 70.
We found that the number of NH Black/AA patient visits, especially in-person and video visits fell in spring/summer 2020 but rose again in fall/winter. Based on data from only 1 year, we cannot determine whether this is a recurring pattern, or unique to 2020, with both the SARS-CoV-2 pandemic and the nationwide protests following the murder of George Floyd in Minneapolis where this study was based. Possible explanations include increased care disruptions from one or both events, and fear of discrimination backlash among Black/AA patients during the human and civil rights protests. Historically, media coverage of human right protests of persons of color has often been racist, biasing public opinion against persons of color [27, 28]. We cannot confirm that Black/AA had increased fear of discrimination in spring/summer 2020, but this explanation would be consistent with the fact that we saw a spring/summer dip in Black/AA in-person and video visits, while phone visits — where skin color is not readily discernible — went up; as well as consistent with a general rise in hate crimes over the past years, and acts of racism in summer 2020 specifically [29, 30].
There may be ways to mitigate the disparities we observed. Studies before and during the pandemic, including some of our own work, found that telehealth has been acceptable to many patients [31–33]; for example, through improved care logistics (travel time to visits, time off of work, costs/logistics associated with childcare for time during appointments) and access to specialists that may not be available in some communities (i.e., genetic counselors in rural areas). Our data, however, suggest telehealth is less utilized in some populations. Further work needs to be done to understand ways to mitigate barriers to telehealth, for example through individualized care models depending on patients’ ability and willingness to participate in telehealth, and accounting for individuals’ health literacy, technology literacy, the quality of telehealth visits and connectivity, which were not available from the EMR data for this study. We also only had information on education for few participants, but education levels may influence the uptake of telehealth. The role of broadband infrastructure needs to be understood; for example, would offering freely available internet options in large cities improve access to high-quality telehealth for those who would like to use it but whose internet access is limited. Lastly, little if any research has been conducted on whether video visits may have better long-term outcomes compared with phone visits, especially in cancer specifically [34].
Strengths of this study included a large sample size, the inclusion of all cancer types without any restrictions, and the detailed comprehensive visualization and analysis of visit data over time in 2020, and by potentially vulnerable patient groups. Limitations included the use of data from only one academic institution in the Midwest, with a heavily non-Hispanic White patient population which does not automatically allow for generalizability to states with different population compositions. Because of small sample sizes, we could not meaningfully evaluate month-to-month participation of BIPOC patient groups other than non-Hispanic Black/AA patients in different types of visits. We also could not conduct multivariate analysis for participation in any type of telehealth versus in-person care as outcome because we had no information on visits that were never scheduled or on the potential eligibility of some in-person visits for telehealth. Some telehealth visits, especially at the beginning of the pandemic, may have been listed as video visits, but due to technical difficulties, may have ended up as phone visits. In that case, it is probable that vulnerable populations (those aged ≥ 70, rural, persons of color) would have been similarly or more, but not less, likely to encounter such technical difficulties. If this resulted in bias, it would have rendered our estimates conservative since we found less frequent video compared with phone use among these vulnerable populations.
Conclusion
Telehealth is here to stay in the care of cancer survivors, and thus understanding and addressing its opportunities and barriers is critical. Some of these opportunities and barriers may be unique to specific population groups such that a “one size fits all” telehealth approach may not be feasible going forward. We found differences in the use of video for telehealth by age, race/ethnicity, and rural versus urban residence in cancer survivors; as well as tentative evidence that rural patients, and to some degree older patients are less likely to participate in telehealth than in in-person care. Future research should evaluate potential underlying contributors to the observed disparities such as technology and internet access, fear of discrimination, and barriers that exist at the provider versus patient level. Additional research is also needed to determine whether telehealth versus in-person visits, and video versus phone visits affect cancer outcomes, therefore indicating whether these differences represent true disparity.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PNG 3 KB) Modeled non-linear relationship (cubic splines) between age and probability of using video (versus phone) for telehealth visits (cubic spline model, in this example with fixed covariates: a Non-Hispanic White female patient with breast cancer living in an urban area).
Supplementary file2 (PNG 13 KB) Shares (%) in visits by selected population groups (aged 18-49, aged 50-69, urban, Non-Hispanic [NH] White) over time in 2020, by type of visit, University of Minnesota Masonic Cancer Center.
Supplementary file3 (PNG 12 KB) Share of video visits (%) among all telehealth visits in March-December 2020 for different population groups over time, N=33,242 visits, University of Minnesota Masonic Cancer Center. * American Indian / Alaska Native. ** Non-Hispanic Black/African American.
Supplementary file4 (PNG 10 KB) Number of completed visits and cancellations by selected vulnerable patient populations over time in 2020, University of Minnesota Masonic Cancer Center. * Non-Hispanic Black/African American.
Supplementary file5 (PNG 8 KB) Number of completed visits and cancellations by selected patient populations (aged 18-49, aged 50-69, urban, Non-Hispanic [NH] White) over time in 2020, University of Minnesota Masonic Cancer Center.
Supplementary file6 (PNG 5 KB) Interaction between age and residential status with regard to video use for telehealth, University of Minnesota Masonic Cancer Center.
Acknowledgements
We would like to thank Vidhyalakshmi Ramesh, Tatiana Ditta, Suzanne Yerg, and Kaia Verich for collecting and helping us understand the electronic medical records data used in this study.
Author contribution
All authors contributed to the study conception and design. Material preparation and data analysis were performed by Patricia Jewett, Anne Blaes, and Rachel Vogel. Interpretation and critical revision for intellectual content were performed by all authors. The first draft of the manuscript was written by Patricia Jewett, and all authors reviewed, revised, and added to previous versions of the manuscript. All authors read and approved the final manuscript version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data availability
The datasets generated and/or analyzed for the current study are protected since they contain sensitive identifiable (medical records numbers, ZIP codes, cancer diagnoses, etc.). Deidentified aggregated versions of the data can be made available upon reasonable request from the corresponding author.
Code availability
We used SAS 9.4 for our analyses. We can provide the code upon request.
Declarations
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board of the University of Minnesota reviewed and approved this study.
Consent to participate
Data for this retrospective review study came from medical records of individuals who had previously provided written consent to have their medical records reviewed for research purposes.
Consent for publication
Not applicable. No individual or identifiable data are included in this article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nanda AM, Sharma R. A review of patient satisfaction and experience with telemedicine: a virtual solution during and beyond COVID-19 pandemic. Telemedicine and e-Health. 2021. 10.1089/tmj.2020.0570 [DOI] [PubMed]
- 2.Kaplan B. Revisting health information technology ethical, legal, and social issues and evaluation: telehealth/telemedicine and COVID-19. Int J Med Inform. 2020;143:104239. 10.1016/j.ijmedinf.2020.104239 [DOI] [PMC free article] [PubMed]
- 3.Jalali MS, Landman A, Gordon WJ. Telemedicine, privacy, and information security in the age of COVID-19. J Am Med Inform Assoc. 2021;28(3):671–672. doi: 10.1093/jamia/ocaa310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sirintrapun SJ, Lopez AM. Telemedicine in cancer care. Am Soc Clin Oncol Educ Book. 2018;38:540–545. doi: 10.1200/EDBK_200141. [DOI] [PubMed] [Google Scholar]
- 5.Schrag D, Hershman DL, Basch E. Oncology practice during the COVID-19 pandemic. JAMA. 2020;323(20):2005–2006. doi: 10.1001/jama.2020.6236. [DOI] [PubMed] [Google Scholar]
- 6.Zimmerman BS, et al. Patient perception of telehealth services for breast and gynecologic oncology care during the COVID-19 pandemic: a single center survey-based study. J Breast Cancer. 2020;23(5):542–552. doi: 10.4048/jbc.2020.23.e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Triantafillou V, Layfield E, Prasad A, Deng J, Shanti RM, Newman JG, et al. Patient perceptions of head and neck ambulatory telemedicine visits: a qualitative study. Otolaryngol Head Neck Surg. 2021;164(5):923–31. [DOI] [PubMed]
- 8.Slightam C, et al. Patient perceptions of video visits using veterans affairs telehealth tablets: survey study. Journal of medical Internet research. 2020;22(4):e15682. doi: 10.2196/15682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lou E, et al. Perspectives of cancer patients and their health during the COVID-19 pandemic. PLoS One. 2020;15(10):e0241741. doi: 10.1371/journal.pone.0241741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lechien JR, Radulesco T, Distinguin L, Chekkoury-Idrissi Y, Circiu MP, Afia FE, et al. Patient and otolaryngologist perceptions of telemedicine during COVID-19 pandemic. European Archives of Oto-Rhino-Laryngology. 2021;1–5. [DOI] [PMC free article] [PubMed]
- 11.Wegermann K, Wilder JM, Parish A, Niedzwiecki D, Gellad ZF, Muir AJ, et al. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19. Dig Dis Sci. 2021;1–7. [DOI] [PMC free article] [PubMed]
- 12.Darrat I, et al. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngology-Head & Neck Surgery. 2021;147(3):287–295. doi: 10.1001/jamaoto.2020.5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lame M, Leyden D, Platt SL. Geocode maps spotlight disparities in telehealth utilization during the COVID-19 pandemic in New York City. Telemedicine and e-Health. 2021;27(3):251–253. doi: 10.1089/tmj.2020.0297. [DOI] [PubMed] [Google Scholar]
- 14.Aziz K, Moon JY, Parikh R, Lorch AC, Friedman DS, Miller JB, et al. Association of patient characteristics with delivery of ophthalmic telemedicine during the COVID-19 pandemic. JAMA Ophthalmology. 2021. [DOI] [PMC free article] [PubMed]
- 15.Rodriguez JA, et al. Disparities in telehealth use among California patients with limited English proficiency: study examines disparities in telehealth use among California patients with limited English proficiency. Health Aff. 2021;40(3):487–495. doi: 10.1377/hlthaff.2020.00823. [DOI] [PubMed] [Google Scholar]
- 16.Jain V, et al. Racial and geographic disparities in internet use in the US among patients with hypertension or diabetes: implications for telehealth in the era of COVID-19. Diabetes Care. 2021;44(1):e15–e17. doi: 10.2337/dc20-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clare CA. Telehealth and the digital divide as a social determinant of health during the COVID-19 pandemic. Network Modeling Analysis in Health Informatics and Bioinformatics. 2021;10(1):1–3. doi: 10.1007/s13721-021-00300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rural health research center. rural-urban commuting area codes (RUCA). Using RUCA data. June 25 2021]; Available from: https://depts.washington.edu/uwruca/ruca-uses.php.
- 19.Surveillance, epidemiology, and end results program (SEER). ICD-10 codes. 24 May 2021]; Available from: https://seer.cancer.gov/tools/conversion/2017/ICD10_to_ICD10CM_FY2017.pdf. Accessed 17 Nov 2021.
- 20.Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2020;1357633X20963893. [DOI] [PMC free article] [PubMed]
- 21.Hoffman DA. Increasing access to care: telehealth during COVID-19. Journal of Law and the Biosciences. 2020;7(1):lsaa043. doi: 10.1093/jlb/lsaa043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lonergan PE, et al. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19: cross-sectional analysis. Journal of medical Internet research. 2020;22(7):e19322. doi: 10.2196/19322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehrotra A, et al. Utilization of telemedicine among rural Medicare beneficiaries. JAMA. 2016;315(18):2015–2016. doi: 10.1001/jama.2016.2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charlton M, et al. Challenges of rural cancer care in the United States. Oncology (Williston Park) 2015;29(9):633–640. [PubMed] [Google Scholar]
- 25.Drake C, et al. The limitations of poor broadband internet access for telemedicine use in rural America: an observational study. Ann Intern Med. 2019;171(5):382–384. doi: 10.7326/M19-0283. [DOI] [PubMed] [Google Scholar]
- 26.Pew Research Center, February 2020. How states are expanding broadband access. 24 May 2021]; Available from: https://www.pewtrusts.org/en/research-and-analysis/reports/2020/02/how-states-are-expanding-broadband-access. Accessed 17 Nov 2021.
- 27.Harlow S, et al. Is the whole world watching? Building a typology of protest coverage on social media from around the world. Journal Stud. 2020;21(11):1590–1608. [Google Scholar]
- 28.Kilgo DK, Harlow S. Protests, media coverage, and a hierarchy of social struggle. The International Journal of Press/Politics. 2019;24(4):508–530. doi: 10.1177/1940161219853517. [DOI] [Google Scholar]
- 29.Center for the study of hate and extremism. 2020 report to the nation: illustrated almanac. 24 May 2021]; Available from: https://www.csusb.edu/sites/default/files/Special%20Status%20Report%20Nov%202020%2011.22.20%20combined.pdf. Accessed 17 Nov 2021.
- 30.The Guardian, 29 July 2020. Hateful incidents against Americans of color surge amid pandemic. 24 May 2021]; Available from: https://www.theguardian.com/us-news/2020/jul/29/hate-crimes-americans-of-color-pandemic. Accessed 17 Nov 2021.
- 31.Isautier, J.M., et al., People’s experiences and satisfaction with telehealth during the COVID-19 pandemic in Australia: cross-sectional survey study. Journal of Medical Internet Research, 2020. 22(12): p. e24531. [DOI] [PMC free article] [PubMed]
- 32.Darcourt JG, et al. Analysis of the implementation of telehealth visits for care of patients with cancer in Houston during the COVID-19 pandemic. JCO oncology practice. 2021;17(1):e36–e43. doi: 10.1200/OP.20.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson BA, et al. The new normal? Patient satisfaction and usability of telemedicine in breast cancer care. Ann Surg Oncol. 2021;28(10):5668–5676. doi: 10.1245/s10434-021-10448-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rush KL, et al. Videoconference compared to telephone in healthcare delivery: a systematic review. Int J Med Informatics. 2018;118:44–53. doi: 10.1016/j.ijmedinf.2018.07.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file1 (PNG 3 KB) Modeled non-linear relationship (cubic splines) between age and probability of using video (versus phone) for telehealth visits (cubic spline model, in this example with fixed covariates: a Non-Hispanic White female patient with breast cancer living in an urban area).
Supplementary file2 (PNG 13 KB) Shares (%) in visits by selected population groups (aged 18-49, aged 50-69, urban, Non-Hispanic [NH] White) over time in 2020, by type of visit, University of Minnesota Masonic Cancer Center.
Supplementary file3 (PNG 12 KB) Share of video visits (%) among all telehealth visits in March-December 2020 for different population groups over time, N=33,242 visits, University of Minnesota Masonic Cancer Center. * American Indian / Alaska Native. ** Non-Hispanic Black/African American.
Supplementary file4 (PNG 10 KB) Number of completed visits and cancellations by selected vulnerable patient populations over time in 2020, University of Minnesota Masonic Cancer Center. * Non-Hispanic Black/African American.
Supplementary file5 (PNG 8 KB) Number of completed visits and cancellations by selected patient populations (aged 18-49, aged 50-69, urban, Non-Hispanic [NH] White) over time in 2020, University of Minnesota Masonic Cancer Center.
Supplementary file6 (PNG 5 KB) Interaction between age and residential status with regard to video use for telehealth, University of Minnesota Masonic Cancer Center.
Data Availability Statement
The datasets generated and/or analyzed for the current study are protected since they contain sensitive identifiable (medical records numbers, ZIP codes, cancer diagnoses, etc.). Deidentified aggregated versions of the data can be made available upon reasonable request from the corresponding author.
We used SAS 9.4 for our analyses. We can provide the code upon request.