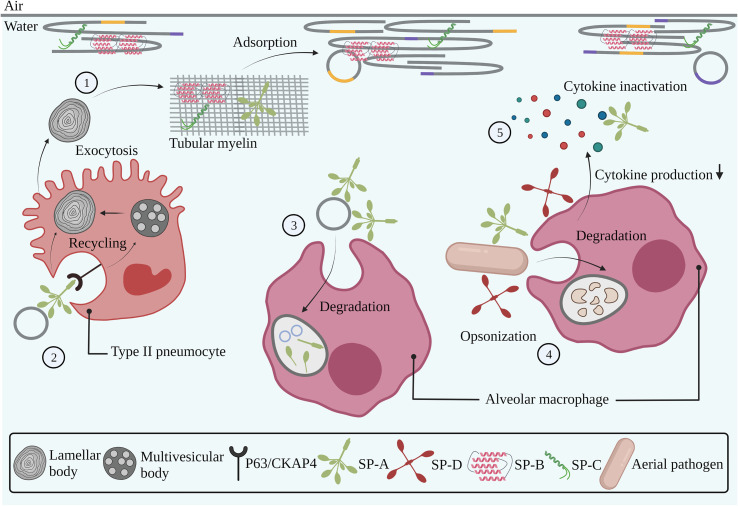
Fig. 3.
Interaction of endogenous pulmonary surfactant with pulmonary cells, cellular membranes and the immune system. Pulmonary surfactant is produced by type II pneumocytes in concentrically organized lamellar bodies, which are partly converted into tubular myelin upon secretion into the alveolar lumen. The presence of SP-B and SP-C in tubular myelin drives the adsorption of surfactant membranes towards the air-liquid interface (1). Binding of SP-A to the P63/CKAP4 receptor expressed by type II pneumocytes induces the uptake and recycling of used surfactant components (2). Degradation of used surfactant components occurs via uptake and phagocytosis by alveolar macrophages (3). SP-A and SP-D are involved in the pulmonary innate immune system via opsonization of aerial pathogens, followed by phagocytosis by alveolar macrophages (4). SP-A and SP-D modulate inflammatory responses via interactions with immune cells, thereby reducing cytokine production, as well as via direct binding and inactivation of soluble cytokines (5). Grey, orange and purple lines represent saturated, unsaturated and cholesterol-rich domains, respectively. Abbreviations: SP-A; surfactant protein-A, SP-B; surfactant protein-B, SP-C; surfactant protein-C, SP-D; surfactant protein-D. Created with BioRender.com (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)