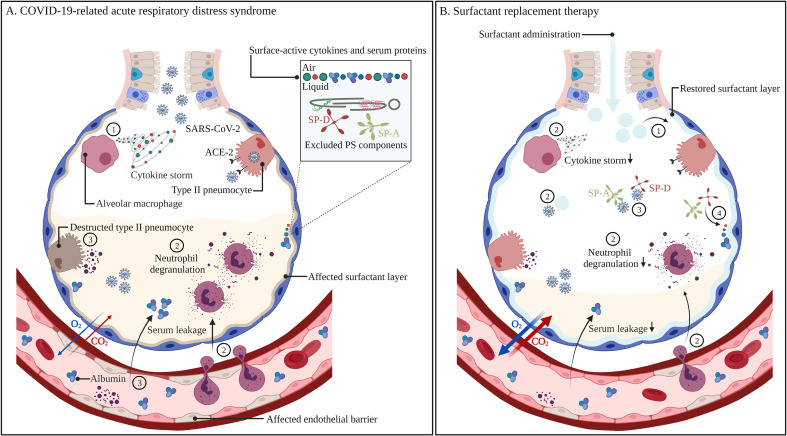
Fig. 4.
Non-treated (A)versus pulmonary surfactant-treated COVID-19-related acute respiratory distress syndrome (B). Infection with SARS-CoV-2 results in the recruitment of alveolar macrophages, which produce high levels of cytokines, also referred to as a cytokine storm (1). Subsequent neutrophil recruitment and degranulation (2) leads to the destruction of type II pneumocytes and endothelial cells, resulting in reduced surfactant production and secretion, serum leakage in the alveolar spaces and surfactant inactivation by surface-active cytokines and serum proteins that adsorb to the air-liquid interface, thereby excluding endogenous PS components (3). Improper surfactant function leads to collapsed alveoli, aberrant gas exchange and respiratory failure. The administration of exogenous surfactant can supplement the affected endogenous PS pool (1), as well as dampen the inflammatory response via interactions with immune cells, cytokines and SARS-CoV-2 (2). Exogenous SP-A and SP-D can prevent viral infection via binding and neutralization of the spike protein, thereby preventing its interaction with the ACE-2 receptor on type II pneumocytes (3). Exogenous SP-A and SP-D grants more resistance towards surfactant inactivation (4). Recovery of the surfactant layer as well as reduced inflammation leads to less cellular damage, reduced serum leakage in the alveolar spaces, enhanced gas exchange and thus the prevention of respiratory failure. Abbreviations: COVID-19; coronavirus disease-19, SARS-CoV-2; severe acute respiratory syndrome coronavirus-2, ACE-2; angiotensin-converting enzyme-2, SP-A; surfactant protein-A, SP-D; surfactant protein-D. Created with BioRender.com