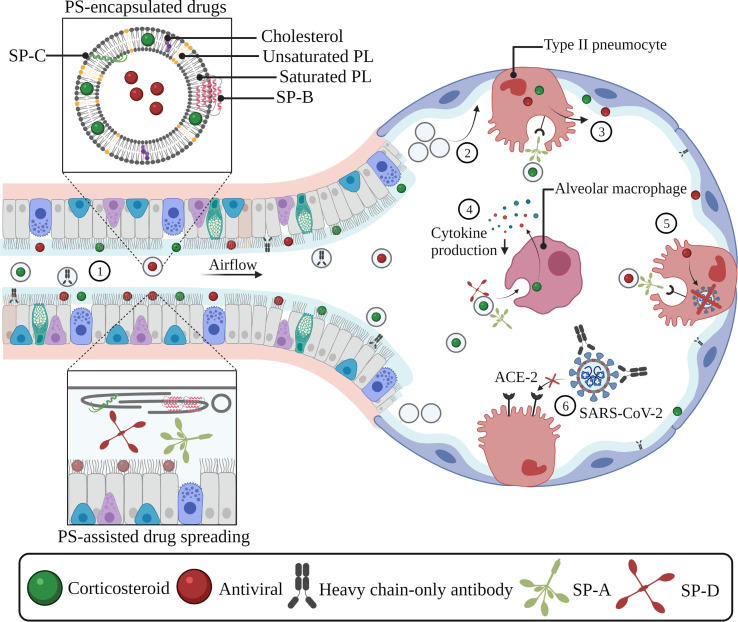
Fig. 5.
Exogenous pulmonary surfactant as a vehicle or liposomal carrier for COVID-19-targeting drugs. Encapsulation of drugs inside exogenous PS can improve drug spreading and adsorption along the entire pulmonary epithelium (1). The administration of exogenous surfactant can supplement the reduced or inactivated endogenous surfactant pool, which prevents alveolar collapse and facilitates the delivery and deposition of inhaled drugs in deeper lung regions (2). SP-A-mediated uptake in type II pneumocytes induces drug- and surfactant recycling, which allows further drug spreading along the alveolar interface (3). SP-A- and SP-D-mediated drug internalization by alveolar macrophages allows anti-inflammatory drugs (e.g. corticosteroids) to interfere with the production of pro-inflammatory cytokines (4). SP-A-mediated uptake of antivirals in type II pneumocytes results in the reduction of viral replication processes and/or viral infectivity via various mechanisms of action (5). PS-assisted delivery of monoclonal-antibody based products (e.g. heavy chain-only antibodies) allows them to bind to viral components (e.g. the spike protein), thereby preventing interactions with the ACE-2 receptor thus reducing their infectivity (6). Abbreviations: SP-A; surfactant protein-A, SP-B; surfactant protein-B, SP-C; surfactant protein-C, SP-D; surfactant protein-D, ACE-2; angiotensin-converting enzyme-2, SARS-CoV-2. severe acute respiratory syndrome coronavirus-2, PL; phospholipid, PS; pulmonary surfactant. Created with BioRender.com