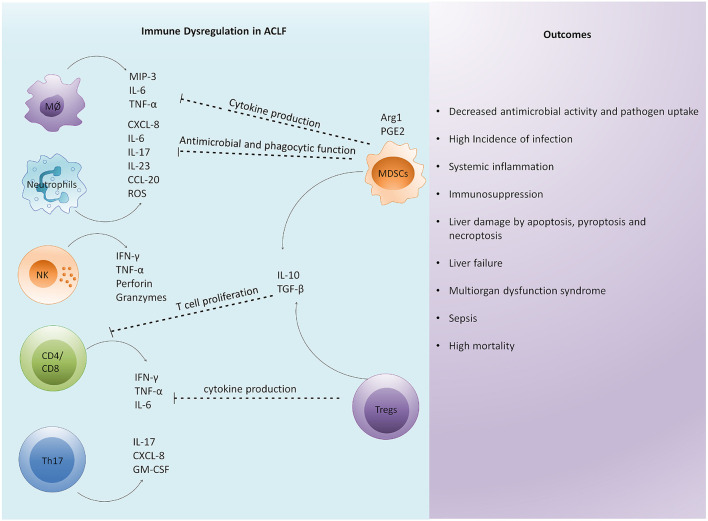
Figure 2.
Immune dysregulation is a critical factor in the pathophysiology of ACLF. Excessive immune activation drives systemic and intrahepatic cytokine storms in patients with ACLF leading to inflammation. Enormous cytokine secretion in the liver results in the infiltration of circulating immune cells that further induce hepatic damage. Subsequently, an antiinflammatory response is generated to control excessive inflammation. However, excessive antiinflammatory response by regulatory cells impairs the function of other immune cells by inhibiting their antimicrobial and phagocytic activities, cytokine secretion, and T cell proliferation. The overall immune dysregulation increases the risk of infection and sepsis development. In addition, it induces distinct cell death related pathways in the liver, causing multiorgan dysfunction leading to high mortality. MØ, macrophage; NK cells, natural killer cells; MIP-3, macrophage inflammatory protein; TNF-α, tumor necrosis factor- α; IFN-γ, interferon-γ; ROS, reactive oxygen species; GM-CSF, granulocyte macrophage colony stimulating factor; Arg1, arginase-1; PGE2, prostaglandin E2; MDSC, myeloid derived suppressor cells; Tregs, regulatory T cells; TGF-β, transforming growth factor-β.