Abstract
Background
Infertility is a global public health issue. Therapies such as intrauterine insemination (IUI) are effective but may be associated with considerable anxiety. Preliminary data suggest that decreasing this anxiety might lead to improved outcomes.
Objective
To determine whether lavender aromatherapy (LA) reduces anxiety during an IUI procedure.
Methods
A randomized controlled trial of women undergoing IUI at a hospital-based fertility clinic. The intervention and comparison were the use of LA vs water. Measurements were the change in anxiety level during an IUI procedure, with secondary assessment of pain scores, patient satisfaction, and pregnancy rates.
Results
In total, 67 women were screened, and 62 women randomly assigned to either placebo (n = 31) or LA (n = 31). No differences were observed in baseline demographic characteristics or visual analog scores for anxiety before IUI (mean [95% CI], 33.9 [25.2 to 45.6] mm vs 41.0 [33.0 to 49.0] mm) in the LA and placebo groups. However, a statistically significant change in anxiety was observed after LA inhalation during the procedure (mean [95% CI], −11.2 [−19.1 to −3.2]) compared with placebo (mean [95% CI], 1.3 [−5.6 to 8.2]; P = .02). No significant difference was observed in pain during IUI in the LA group vs placebo group. Patient satisfaction was high, with 93% of respondents in the LA group satisfied with the aromatherapy during their procedure. Additionally, 76% of participants who received placebo reported that they would prefer to use LA during their IUI. No statistically significant difference was detected in pregnancy rates between the 2 groups: 19.4% with LA vs 9.7% with placebo (P = .47).
Conclusion
LA reduced anxiety and was preferred by women during IUI fertility treatments.
Keywords: anxiety, infertility, intrauterine insemination, lavender aromatherapy
Background
Infertility is a global public health issue and has been acknowledged as a disease state by the World Health Organization.1-4 Noted to affect 12% of couples in the US, infertility contributes to more than one-half of all cases of global childlessness. Additionally, infertility rates have increased with the increasing age at first birth and with increased rates of diagnosis that accompany improved access to care.5-7 The challenges faced by persons with infertility are immense, and negative effects have been documented in psychosocial and relationship domains, with a statistically significant impact on quality of life.8-10
Infertility treatments range from lifestyle changes to operations and the use of oral or injectable medications with or without intrauterine insemination (IUI) to in vitro fertilization.11,12 Intrauterine insemination is considered first-line therapy for couples with unexplained infertility or mild male factor infertility or for women pursuing pregnancy with donor sperm.4,13-15
Procedurally, IUI is similar to placement of an intrauterine device (IUD). A speculum is placed in the vagina to visualize the cervix. Next, a thin flexible catheter is passed through the cervical canal while attached to a syringe prefilled with sperm washed for removal of other semen components and concentrated. The sperm are injected directly into the uterine cavity. Comparatively, IUD placement requires a slightly larger diameter catheter with farther entry into the uterine cavity.
Clinically important baseline anxiety has been reported in women undergoing IUD placement. This baseline anxiety regarding the procedure has been shown to affect patient decision-making and, ultimately, avoidance of IUD placement. 16 Similarly, women have different levels of anxiety, stress, and pain during infertility treatment procedures, including IUI. Patients with infertility specifically report anxiety and pain due to physical discomfort and the eagerness and anticipation of a long-awaited pregnancy. 17
Complementary and integrative medicine has been suggested as a supportive adjunct to address physical and psychologic distress during infertility treatments.18-22 Patients prefer integrative approaches for a low adverse effect profile and for proven efficacy as adjunct nonpharmacotherapy options for anxiety, stress, pain, and other psychological symptoms.23-25 Aromatherapy is an integrative therapy modality that has been widely trialed in various patient populations and practice settings.26,27
Previous studies have shown the benefit of aromatherapy in reduction of anxiety, pain, and other symptoms in the perioperative setting. Lavender aromatherapy (LA) has been specifically noted in prior studies to reduce stress and anxiety through its actions on the limbic system (LA). 28 For example, one prior study investigated the use of aromatherapy during IUD insertion and found a statistically significant decrease in anxiety measured before IUD insertion with use of LA compared with baseline anxiety levels. 16 No study, to our knowledge, has assessed use of aromatherapy during IUI procedures. In the present randomized controlled trial, we aimed to evaluate the use of LA for patients undergoing IUI, with assessment for patient anxiety, pain, and satisfaction before, during, and after IUI. Because of the nature of the intervention, the intervention was not masked to study participants or providers.
Methods
Study Design
This prospective randomized trial studied 62 patients undergoing IUI in an academic fertility center. The Mayo Clinic Institutional Review Board approved the trial. We aimed to enroll 62 women between ages 18 and 45 years who underwent IUI from May 1, 2017 to March 31, 2018. Women older than 45 are not eligible to receive fertility treatments with IUI in our practice, given the limited likelihood of success of treatment at this reproductive age. We excluded from participation women with a known allergy to LA or its components and women who reported current use of aromatherapy, since prior experience might increase the risk of negative perception of being enrolled in the placebo arm and skew the outcome in favor of active therapy. Demographic data were abstracted with manual chart review and included age, height, weight and ethnicity. Body mass index was calculated from height and weight. Infertility data included type of fertility treatment, semen parameters and the ease of the IUI procedure.
All patients enrolled and consented the day they presented for an IUI procedure by the same study coordinator (S.M.). Randomization was achieved a priori with a 1-to-1 variable block approach in blocks of 4 patients. Group assignments were placed in opaque numbered envelopes. The group was revealed to the study coordinator after the patient agreed to participate in the trial. The primary end point was change in anxiety level throughout the IUI procedure. Secondary end points were change in pain score, patient satisfaction, and pregnancy rate. Pregnancy rates were included because they are a meaningful outcome in studies focused on fertility treatments or adjuncts. Inclusion of this secondary end point was exploratory because no existing literature suggests that LA improves pregnancy rates in attempts at spontaneous conception or during fertility treatment cycles.
Procedure
After agreeing to study participation, each patient was asked to complete a hospital anxiety and depression scale (HADS). 29 The HADS was completed independently and before undressing for the IUI procedure. Following HADS completion, the nurse or physician performing the IUI and the study coordinator reentered the procedure room. As per standard IUI procedure at our institution, the patient was asked to review and confirm correct data identifying the inseminate.
The study coordinator assessed anxiety and pain before, during, and after the IUI procedure. Intrauterine insemination procedures are brief, with procedural length ranging from 1 to 2 minutes. Anxiety was assessed with a 100 mm visual analog scale (VAS).30-32 Patients were asked to mark along this scale at the point that best correlated with their anxiety level. A standard 10-point Wong-Baker pain rating scale (0, no pain; 10, worst possible pain) 33 was used to measure pain preprocedure, during IUI, and postprocedure. Before the patient left the procedure room, a postprocedure assessment of anxiety, pain, and satisfaction was placed in the room for the participant to fill out in private. The satisfaction survey consisted of 4 questions about whether the patient was satisfied with LA, preferred LA, would recommend LA, and would use LA again. A 5-point Likert scale was used, with the responses strongly disagree, disagree, neutral, agree, and strongly agree.
Trial participants were given a purple porous drawstring pouch after their baseline anxiety and pain scores were obtained. For patients who were randomly assigned to the LA arm, the pouch contained a cotton ball with 1 drop of lavender essential oil (Lavandula angustifolia; Wyndmere Naturals). Those patients randomly assigned to the control arm were given a pouch with 1 drop of water on a cotton ball, as used in prior studies. 34 Participants were asked to smell the pouch during the procedure. The duration and frequency of LA use were not recorded or measured.
Statistical Analysis
On the basis of previous work by Shahnazi et al, 16 we assumed a mean (SD) change in anxiety in the experimental group of −4.19 (6.39) and in the placebo group of −.74 (4.18). Using a two-sided twosample t test and assuming unequal variance, we learned that 62 patients (31 per trial arm) were needed to obtain a power of 80% at alpha .05. Continuous variables were summarized and analyzed with 2-sample t test or Wilcoxon rank sum test as appropriate. Categorical variables were summarized as number (percent) and analyzed with χ2 test or Fisher exact test as appropriate. End points of anxiety and pain preprocedure and postprocedure were analyzed with paired 2-sample t test for change from baseline. Cohen’s d was calculated to estimate the effect size for the end points of anxiety and pain. P < .05 was considered statistically significant. SAS software (version 9; SAS Institute Inc) was used for data analysis. Research was performed in accordance with CONSORT (Consolidated Standards of Reporting Trials).
Results
Sample Population
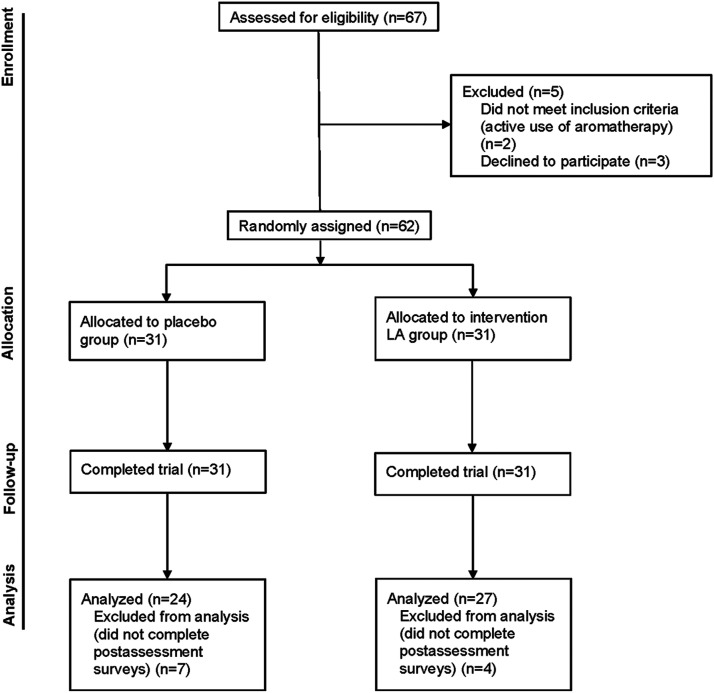
Sixty-seven patients (enrollment rate, 93%) were assessed from May 1, 2017 through March 31, 2018 (Figure 1). Five patients were excluded; three declined participation and two were excluded because they reported use of aromatherapy at enrollment. The other 62 patients completed the study intervention. However, seven participants in the placebo arm and 4 in the LA arm did not complete their postprocedure assessment or their satisfaction survey. Participants reported no adverse effects of LA use. Patient characteristics were assessed between the respondents and the nonrespondents of the survey, and no statistical difference was found (P > .05). The demographic and treatment cycle characteristics of all patients are outlined in Table 1. No differences were observed in baseline patient characteristics. The mean age in the placebo and LA arms was 33.4 (4.6) vs 31.5 (3.2) years (P = .06). Most participants self-identified as White (placebo arm, 87.1%; LA arm, 98.8%; P = .42), consistent with overall practice demographic characteristics. The mean (SD) duration of infertility for the placebo arm was 1.4 (1.1) years compared with 1.2 (1.2) years in the LA arm (P = .83).
Figure 1.
Consolidated standards of reporting trials flow diagram. LA indicates lavender aromatherapy.
Table 1.
Patient and cycle characteristics.
| Group a | |||
|---|---|---|---|
| Characteristic | Placebo (n=31) | LA (n=31) | P Value |
| Patient | |||
| Age, y | 33.4 (4.6) | 31.5 (3.2) | .06 b |
| BMI | 27.3 (5.9) | 27.6 (6.8) | .83 b |
| White race | 27 (87.1) | 30 (96.8) | .35 c |
| Infertility period, y | 1.4 (1.1) | 1.2 (1.2) | .45 |
| Previous IUI | 16 (51.6) | 15 (48.4) | .79 d |
| FSH, IU/L | 6.9 (2.1) | 7.1 (1.7) | .76 b |
| Missing, No. | 9 | 7 | |
| Estradiol, pg/mL | 44.6 (30.7) | 45.6 (37.1) | .81 b |
| Missing, No. | 9 | 9 | |
| AMH, ng/mL | 4.2 (5.2) | 3.7 (2.2) | .67 b |
| Missing, No | 4 | 0 | |
| Antral follicle count | 21.4 (13.9) | 25.9 (13.9) | .25 b |
| Missing, No. | 4 | 5 | |
| HADS score | |||
| Anxiety | 5.5 (3.1) | 6.5 (3.2) | .22 b |
| Depression | 1.9 (3.1) | 1.8 (2.3) | .89 b |
| Cycle | |||
| Protocols | >.99 c | ||
| Clomiphene citrate | 20 (64.5) | 19 (61.3) | |
| Letrozole | 7 (22.6) | 7 (22.6) | |
| Gonadotropin | 2 (6.5) | 3 (9.7) | |
| Natural cycle | 2 (6.5) | 2 (6.5) | |
| hCG trigger | 22 (71.0) | 20 (64.5) | .59 d |
| Partner present | 15 (48.4) | 16 (51.6) | .80 d |
| Follicular recruitment | 2.7 (1.5) | 3.0 (1.9) | .46 b |
| Missing, No. | 7 | 10 | |
| Endometrial echo complex, mm | 7.1 (2.9) | 6.8 (2.9) | .82 b |
| Missing, No. | 7 | 10 | |
| IUI procedure | .68 c | ||
| Easy | 25 (80.7) | 22 (71.0) | |
| Moderately easy | 2 (6.5) | 3 (9.7) | |
| Difficult | 4 (12.9) | 6 (19.3) | |
| Total motile sperm count, ×106 | 64.2 (58.5) | 34.5 (30.1) | .02 b |
| Sperm motility, % | 79.0 (15.5) | 74.5 (15.9) | .26 b |
| Progesterone supplementation | 5 (16.1) | 4 (12.9) | >.99 c |
Abbreviations: AMH, anti-Müllerian hormone; BMI, body mass index; FSH, follicle-stimulation hormone; HADS, hospital anxiety and depression scale; hCG, human chorionic gonadotropin; IUI, intrauterine insemination; LA, lavender aromatherapy.
aData represent mean (SD) or number (percentage) unless otherwise specified.
bt test used for continuous variables.
cFisher exact test used for categorical variables as appropriate.
dχ2 used for categorical variables as appropriate.
Anxiety and Pain Score
HADS scores less than 7 are considered normal for anxiety and depression. 29 HADS scores for baseline anxiety and depression were not different between the two groups: placebo group, mean (SD) HADS anxiety score, 5.5 (3.1); LA group, mean (SD) score, 6.5 (3.2) (Table 1). Cycle characteristics were similar between the two arms with the exception of lower total motile sperm count in the LA group (P = .02).
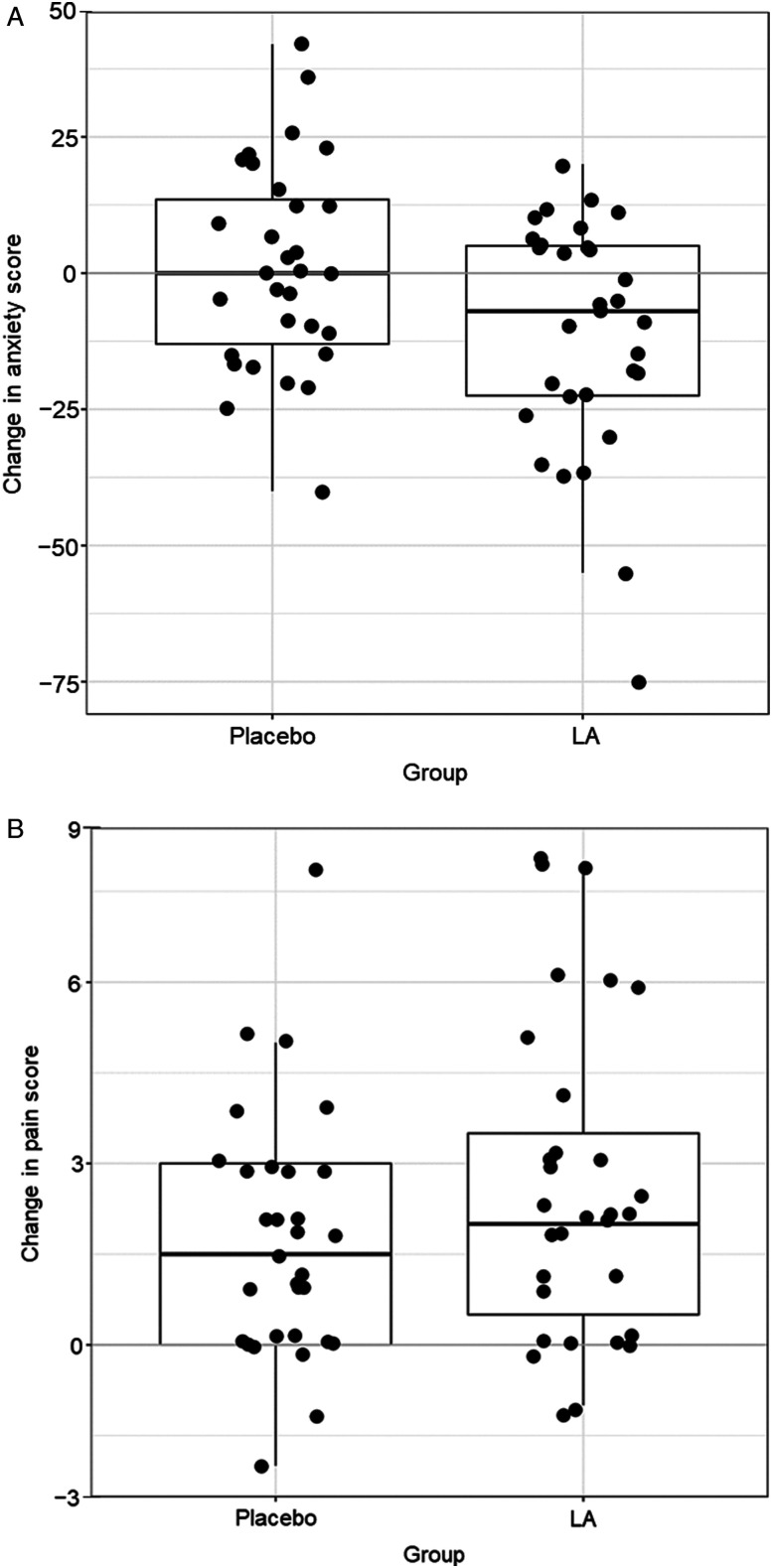
The mean (95% CI) preprocedure VAS anxiety level was 33.9 (25.2 to 45.6) in the placebo arm compared with 41.0 (33.0 to 49.0) in the LA arm (P = .22) (Table 2). No differences in VAS anxiety levels were discerned during IUI or after it. However, the change from baseline anxiety to the anxiety during the IUI procedure showed that participants in the LA arm had a decrease in VAS anxiety (mean [95% CI ], −11.6 [−19.1 to −3.2]) compared with participants in the placebo arm, who had nearly no change in anxiety (mean [95% CI], 1.3 [5.6 to 8.2]; P = .02) (Figure 2).
Table 2.
Analysis of change in pain score and anxiety level throughout the IUI procedure.
| Groupa,b | ||||
|---|---|---|---|---|
| Outcome | Placebo (n=31) | LA (n=31) | Cohen’s da | P Value |
| Anxiety level | ||||
| Pre-IUI | 33.9 (25.2 to 45.6) | 41.0 (33.0 to 49.0) | .31 (−.19 to .81) | .22 |
| During c | 1.3 (−5.6 to 8.2) | −11.2 (−19.1 to −3.2) | −.61 (−1.12 to −.10) | .02 |
| Post-IUIc,d | −24.4 (−33.0 to −15.9) | −25.0 (−34.6 to −15.4) | .02 (−.55 to .50) | .93 |
| Pain score | ||||
| Pre-IUI | .4 (.0 to .8) | .2 (.0 to .4) | .20 (−.69 to .31) | .45 |
| During c | 1.8 (1.0 to 2.5) | 2.6 (1.6 to 3.6) | .36 (−.15 to .86) | .16 |
| Post-IUIc,d | .0 (−.2 to .2) | 1.0 (.2 to 1.7) | .65 (.10 to 1.19) | .02 |
| Clinical pregnancy, e No. (%) | 3 (9.7) | 6 (19.4) | .47 | |
Abbreviations: IUI, intrauterine insemination; LA, lavender aromatherapy.
aValues are presented as mean (95% CI) unless specified otherwise.
bTwo-sample t test was used for analysis of continuous variables; Fisher exact test for analysis of categorical variables.
cChange in score from baseline.
dIn placebo group, n = 27; in LA group, n = 28.
eClinical pregnancy was analyzed with Fisher exact test.
Figure 2.
Scatter and box plot showing mean change during intrauterine insemination (IUI) from pre-IUI. A, Anxiety level. B, Pain level. Median (interquartile range) of the differences is shown. LA indicates lavender aromatherapy.
Pain scores stayed relatively low throughout the IUI procedure. No statistically significant difference was shown between baseline pain scores among placebo and LA groups (P = .45) (Table 2). Differences in pain scores during IUI were statistically significant but not clinically important (mean [95% CI], 1.8 [1.0 to 2.5] for placebo group vs 2.6 [1.6 to 3.6] for LA group; P = .02). Of note, 23 patients (95.8%) in the placebo arm reported no change in pain compared with 14 patients (51.9%) in the LA group. In contrast, only two patients (7%) in the placebo arm reported decreased pain compared with 12 patients (43%) in the LA group. One LA participant had an 8/10 pain score postprocedure. She did not require any intervention.
Patient Satisfaction
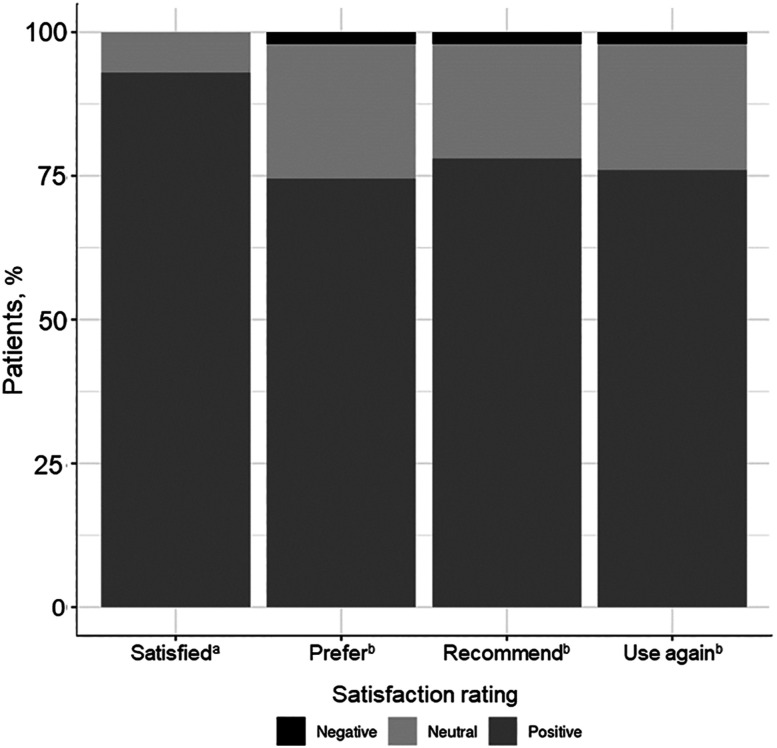
In the LA group, 27 patients completed their LA satisfaction survey. Of these, 25 (92.6%) responded positively, 2 (6.5%) were neutral, and no patient responded negatively to the satisfaction question (Figure 3). Of the placebo group, 24 patients completed the LA satisfaction survey; 7 (29.2%) gave a positive response, 14 (58.3%) gave a neutral response, and 3 (12.5%) gave a negative response. Of all participants who completed the survey, 74.5% responded positively when asked whether they preferred LA during an IUI procedure (placebo group, 16 [66.7%]; LA group, 22 [81.5%]). The majority of participants (78.4%, n=40) responded that they would recommend LA to other patients and would prefer LA (76.5%, n = 39) at their next IUI.
Figure 3.
Lavender aromatherapy (LA) results proposed for LA satisfaction survey. Among participants who received LA, 92.6% (n = 25) were satisfied with its effect and 6.5% (n = 2) had a neutral response. Of survey respondents, 74.5% (n = 38) preferred LA, 23.5% (n = 12) were neutral about LA, and 2.0% (n = 1) had a negative response. In addition, 78.4% (n = 40) would recommend LA to another patient, 19.6% (n = 10) were neutral, and 2.0% (n = 1) would not recommend its use. Among all survey participants, 76.5% (n = 39) responded that they would use LA again, 21.6% (n = 11) were neutral, and 2.0% (n = 1) would not use LA again. Footnote “a” indicates patients randomly assigned to LA (n = 27); footnote “b,” all participants who completed the survey (n = 51).
Discussion
The present randomized controlled trial highlights a novel use of LA for women undergoing IUI fertility procedures. LA was shown to decrease procedural anxiety and had a high rate of patient satisfaction and request for future use. Lavender aromatherapy had no statistically significant effect on pain scores during the procedure or on pregnancy rate.
Multiple studies of LA have shown that it has a positive effect on reducing anxiety in low acuity settings. The outcomes showed this result for patient-reported levels and for physiologic signs of stress, including systolic blood pressure, heart rate, and salivary cortisol concentration. 35 Comparatively, studies following major cardiac operation have showed mixed effects, with LA having either positive benefit or no effect on anxiety and pain.34,36-38 Our study found no effect of LA on pain scores during the procedure. Interestingly, however, patients who received LA in our study had a statistically significant increased pain score after the procedure (score, 1) compared with the placebo group (score, 0). The impact of LA on postprocedural pain scores has been mixed and not previously studied in this patient population.
Aromatherapy, and specifically LA, has been applied to multiple facets of women’s health. For women with premenstrual syndrome and primary dysmenorrhea (pain with periods), LA has been shown to minimize the symptoms of pain, anxiety, and depression.39-41 Additionally, LA has been shown to decrease anxiety in early labor and to improve postpartum symptoms of stress, anxiety, and depression.42,43 Among women with menopausal symptoms, such as hot flashes, sexual dysfunction, and sleep disturbances, LA has had positive effects.44,45
When used as aromatherapy, lavender oil has few adverse effects. Although multiple accounts of contact dermatitis or other allergic reactions have been reported with topical use, 46 our protocol avoided direct contact with skin. Interestingly, two large cohort studies found that the prevalence of lavender allergy, through a retrospective review of patch testing, ranged from 2.2% to 3.7% in patients referred for the testing, and 1 group had a history of cosmetic dermatitis.47,48 Care providers should take precautions for potential contact reactions but can feel confident in offering lavender oil for use as aromatherapy. 49
Compared with the general population, women with infertility have a high degree of anxiety and depression. 50 Procedural aspects of fertility care present scenarios of heightened anxiety; the interventional and sensitive nature of the procedures adds to the high emotional and financial tolls of treatment. Studies on use of alternative and complementary medicine by fertility patients have shown high degrees of use—nearly 75.5% in one study—primarily for such treatments as acupuncture and reflexology. 51 The rates of anxiety and depression of patients with infertility, coupled with their willingness to pursue alternative therapies, make this an ideal patient population for LA.
Our study identified LA as a meaningful treatment adjunct for women pursuing IUI for fertility treatment. The strengths of our study include its randomized design and standardized assessment of patient response. However, the findings of our study are limited by its small sample size and lack of patient diversity. Baseline anxiety was not considered for inclusion or exclusion criteria and would be important to consider for future trials. Additionally, we did not assess whether patient preference for LA during IUI would impact decision-making about pursuit of additional or more aggressive fertility treatment options, or both, another limitation of our study. Future research with a larger sample size, with inclusion of more diverse patients, is needed to confirm our results. In summary, the present study suggests that LA is a simple, cost-effective adjunct therapy for women undergoing IUI fertility procedures.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author’s Note: Reprints: Brent A. Bauer, MD, Division of General Internal Medicine, Mayo Clinic, 200 First St SW, Rochester, MN 55905 (bauer.brent@mayo.edu). Presented at Gynecological Endocrinology: the 18th World Congress, International Society of Gynecological Endocrinology, Firenze, Italy, March 7-10, 2018.
Trial Registration: Clinical Trial Registration No. NCT03461055
ORCID iDs
Saswati Mahapatra https://orcid.org/0000-0002-6929-1382
Brent A. Bauer https://orcid.org/0000-0003-3453-6906
References
- 1.Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22(6):1506-1512. doi: 10.1093/humrep/dem046 [DOI] [PubMed] [Google Scholar]
- 2.Gurunath S, Pandian Z, Anderson RA, Bhattacharya S. Defining infertility--a systematic review of prevalence studies. Hum Reprod Update. 2011;17(5):575-588. doi: 10.1093/humupd/dmr015 [DOI] [PubMed] [Google Scholar]
- 3.Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12):e1001356. doi: 10.1371/journal.pmed.1001356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ombelet W, Campo R, Bosmans E, Nijs M. Intrauterine insemination (IUI) as a first-line treatment in developing countries and methodological aspects that might influence IUI success. ESHRE Monogr. 2008;2008(1):64-72. doi: 10.1093/humrep/den165 [DOI] [Google Scholar]
- 5.Moreau C, Bouyer J, Ducot B, Spira A, Slama R. When do involuntarily infertile couples choose to seek medical help? Fertil Steril. 2010;93(3):737-744. doi: 10.1016/j.fertnstert.2008.10.011 [DOI] [PubMed] [Google Scholar]
- 6.Swift BE, Liu KE. The effect of age, ethnicity, and level of education on fertility awareness and duration of infertility. J Obstet Gynaecol Can. 2014;36(11):990-996. doi: 10.1016/S1701-2163(15)30412-6 [DOI] [PubMed] [Google Scholar]
- 7.Greil AL, McQuillan J. Help‐seeking patterns among subfecund women. J Reprod Infant Psychol. 2004;22(4):305-319. doi: 10.1080/02646830412331298332 [DOI] [Google Scholar]
- 8.Benyamini Y, Gozlan M, Kokia E. Women’s and men’s perceptions of infertility and their associations with psychological adjustment: a dyadic approach. Br J Health Psychol. 2009;14(Pt 1):1-16. doi: 10.1348/135910708X279288 [DOI] [PubMed] [Google Scholar]
- 9.Kim JH, Shin HS, Yun EK. A dyadic approach to infertility stress, marital adjustment, and depression on quality of life in infertile couples. J Holist Nurs. 2018;36(1):6-14. doi: 10.1177/0898010116675987 [DOI] [PubMed] [Google Scholar]
- 10.Pasch LA, Sullivan KT. Stress and coping in couples facing infertility. Curr Opin Psychol. 2017;13:131-135. doi: 10.1016/j.copsyc.2016.07.004 [DOI] [PubMed] [Google Scholar]
- 11.Jin J. JAMA patient page. Treatments for infertility. J Am Med Assoc. 2015;313(3):320. doi: 10.1001/jama.2014.7051 [DOI] [PubMed] [Google Scholar]
- 12.Zhong X, Liu J, Cui Q, et al. Effect of parental physiological conditions and assisted reproductive technologies on the pregnancy and birth outcomes in infertile patients. Oncotarget. 2017;8(11):18409-18416. doi: 10.18632/oncotarget.12553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duran HE, Morshedi M, Kruger T, Oehninger S. Intrauterine insemination: a systematic review on determinants of success. Hum Reprod Update. 2002;8(4):373-384. doi: 10.1093/humupd/8.4.373 [DOI] [PubMed] [Google Scholar]
- 14.Cantineau AE, Cohlen BJ, Heineman MJ, Marjoribanks J, Farquhar C. Intrauterine insemination versus fallopian tube sperm perfusion for non-tubal infertility. Cochrane Database Syst Rev. 2013;10(2):CD001502. doi: 10.1002/14651858.CD001502.pub4 [DOI] [PubMed] [Google Scholar]
- 15.Sinha P, Pandey K, Srivastava A. Factors determining successful intrauterine insemination. Int J Reprod Contracept Obstet Gynecol. 2017;6(9):3887-3891. doi: 10.18203/2320-1770.ijrcog20174028 [DOI] [Google Scholar]
- 16.Shahnazi M, Nikjoo R, Yavarikia P, Mohammad-Alizadeh-Charandabi S. Inhaled lavender effect on anxiety and pain caused from intrauterine device insertion. J Caring Sci. 2012;1(4):255-261. doi: 10.5681/jcs.2012.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benyamini Y, Gozlan M, Kokia E. Variability in the difficulties experienced by women undergoing infertility treatments. Fertil Steril. 2005;83(2):275-283. doi: 10.1016/j.fertnstert.2004.10.014 [DOI] [PubMed] [Google Scholar]
- 18.Agarwal A, Ranjan R, Dhiraaj S, Lakra A, Kumar M, Singh U. Acupressure for prevention of pre-operative anxiety: a prospective, randomised, placebo controlled study. Anaesthesia. 2005;60(10):978-981. doi: 10.1111/j.1365-2044.2005.04332.x [DOI] [PubMed] [Google Scholar]
- 19.Marc I, Toureche N, Ernst E, et al. Mind-body interventions during pregnancy for preventing or treating women’s anxiety. Cochrane Database Syst Rev. 2011;2011(7):CD007559. doi: 10.1002/14651858.CD007559.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sniezek DP, Siddiqui IJ. Acupuncture for treating anxiety and depression in women: a clinical systematic review. Med Acupunct. 2013;25(3):164-172. doi: 10.1089/acu.2012.0900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson KA. An integrative approach to diagnosing and treating unexplained infertility. J Chin Med 2018;118:49-57. [Google Scholar]
- 22.Zafman KB, Sabo M, Thake E, Lee J, Copperman A, Mukherjee T. Patients undergoing assisted reproductive technology (ART) treatments seek integrative approach to infertility [27F]. Obstet Gynecol. 2016;127:58S. doi: 10.1097/01.Aog.0000483882.51977.58 [DOI] [Google Scholar]
- 23.Johnson JR, Crespin DJ, Griffin KH, et al. The effectiveness of integrative medicine interventions on pain and anxiety in cardiovascular inpatients: a practice-based research evaluation. BMC Complement Altern Med. 2014;14:486. doi: 10.1186/1472-6882-14-486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schlegel ML, Whalen JL, Williamsen PM. Integrative therapies for women with a high risk pregnancy during antepartum hospitalization. MCN Am J Matern Child Nurs. 2016;41(6):356-362. doi: 10.1097/NMC.0000000000000279 [DOI] [PubMed] [Google Scholar]
- 25.Smith CA, Ussher JM, Perz J, Carmady B, de Lacey S. The effect of acupuncture on psychosocial outcomes for women experiencing infertility: a pilot randomized controlled trial. J Altern Complement Med. 2011;17(10):923-930. doi: 10.1089/acm.2010.0380 [DOI] [PubMed] [Google Scholar]
- 26.Tsai SS, Wang HH, Chou FH. The effects of aromatherapy on postpartum women: a systematic review. J Nurs Res. 2020;28(3):e96. doi: 10.1097/jnr.0000000000000331 [DOI] [PubMed] [Google Scholar]
- 27.Xiao Y, Li L, Xie Y, Xu J, Liu Y. Effects of aroma therapy and music intervention on pain and anxious for breast cancer patients in the perioperative period. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2018;43(6):656-661. doi: 10.11817/j.issn.1672-7347.2018.06.013 [DOI] [PubMed] [Google Scholar]
- 28.Koulivand PH, Khaleghi Ghadiri M, Gorji A. Lavender and the nervous system. Evid Based Complement Alternat Med. 2013;2013:681304. doi: 10.1155/2013/681304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1:29. doi: 10.1186/1477-7525-1-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luyk NH, Beck FM, Weaver JM. A visual analogue scale in the assessment of dental anxiety. Anesth Prog. 1988;35(3):121-123. [PMC free article] [PubMed] [Google Scholar]
- 31.Harada T, Kurai R, Ito S, et al. Effect of joyful and anxiety-provoking music on autonomic nervous system function. Int Med J. 2017;24:211-213. [Google Scholar]
- 32.Klausenitz C, Hacker H, Hesse T, et al. Auricular acupuncture for exam anxiety in medical students-a randomized crossover investigation. PLoS One. 2016;11(12):e0168338. doi: 10.1371/journal.pone.0168338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qazi Y, Hurwitz S, Khan S, Jurkunas UV, Dana R, Hamrah P. Validity and reliability of a novel ocular pain assessment survey (OPAS) in quantifying and monitoring corneal and ocular surface pain. Ophthalmology. 2016;123(7):1458-1468. doi: 10.1016/j.ophtha.2016.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bikmoradi A, Seifi Z, Poorolajal J, Araghchian M, Safiaryan R, Oshvandi K. Effect of inhalation aromatherapy with lavender essential oil on stress and vital signs in patients undergoing coronary artery bypass surgery: a single-blinded randomized clinical trial. Complement Ther Med. 2015;23(3):331-338. doi: 10.1016/j.ctim.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 35.Kang HJ, Nam ES, Lee Y, Kim M. How strong is the evidence for the anxiolytic efficacy of lavender?: systematic review and meta-analysis of randomized controlled trials. Asian Nurs Res. 2019;13(5):295-305. doi: 10.1016/j.anr.2019.11.003 [DOI] [PubMed] [Google Scholar]
- 36.Salamati A, Mashouf S, Mojab F. Effect of inhalation of lavender essential oil on vital signs in open heart surgery ICU. Iran J Pharm Res (IJPR). 2017;16(1):404-409. [PMC free article] [PubMed] [Google Scholar]
- 37.Najafi Z, Taghadosi M, Sharifi K, Farrokhian A, Tagharrobi Z. The effects of inhalation aromatherapy on anxiety in patients with myocardial infarction: a randomized clinical trial. Iran Red Crescent Med J. 2014;16(8):e15485. doi: 10.5812/ircmj.15485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salamati A, Mashouf S, Sahbaei F, Mojab F. Effects of inhalation of lavender essential oil on open-heart surgery pain. Iran J Pharm Res (IJPR). 2014;13(4):1257-1261. [PMC free article] [PubMed] [Google Scholar]
- 39.Uzunçakmak T, Ayaz Alkaya S. Effect of aromatherapy on coping with premenstrual syndrome: a randomized controlled trial. Complement Ther Med. 2018;36:63-67. doi: 10.1016/j.ctim.2017.11.022 [DOI] [PubMed] [Google Scholar]
- 40.Nikjou R, Kazemzadeh R, Rostamnegad M, Moshfegi S, Karimollahi M, Salehi H. The effect of lavender aromatherapy on the pain severity of primary dysmenorrhea: a triple-blind randomized clinical trial. Ann Med Health Sci Res. 2016;6(4):211-215. doi: 10.4103/amhsr.amhsr_527_14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matsumoto T, Asakura H, Hayashi T. Does lavender aromatherapy alleviate premenstrual emotional symptoms?: a randomized crossover trial. Biopsychosoc Med. 2013;7:12. doi: 10.1186/1751-0759-7-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kianpour M, Mansouri A, Mehrabi T, Asghari G. Effect of lavender scent inhalation on prevention of stress, anxiety and depression in the postpartum period. Iran J Nurs Midwifery Res. 2016;21(2):197-201. doi: 10.4103/1735-9066.178248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vaziri F, Shiravani M, Najib FS, Pourahmad S, Salehi A, Yazdanpanahi Z. Effect of lavender oil aroma in the early hours of postpartum period on maternal pains, fatigue, and mood: a randomized clinical trial. Int J Prev Med. 2017;8:29. doi: 10.4103/ijpvm.IJPVM_137_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salehi-Pourmehr H, Ostadrahimi A, Ebrahimpour-Mirzarezaei M, Farshbaf-Khalili A. Does aromatherapy with lavender affect physical and psychological symptoms of menopausal women? A systematic review and meta-analysis. Complement Ther Clin Pract. 2020;39:101150. doi: 10.1016/j.ctcp.2020.101150 [DOI] [PubMed] [Google Scholar]
- 45.Kazemzadeh R, Nikjou R, Rostamnegad M, Norouzi H. Effect of lavender aromatherapy on menopause hot flushing: a crossover randomized clinical trial. J Chin Med Assoc. 2016;79(9):489-492. doi: 10.1016/j.jcma.2016.01.020 [DOI] [PubMed] [Google Scholar]
- 46.Corazza M, Amendolagine G, Borghi A, Toni G, Lauriola MM. Aromatherapy and occupational allergic contact dermatitis: two further cases caused by lavender oil and other essential oils. Contact Dermatitis 2019;81(5):378-379. doi: 10.1111/cod.13328 [DOI] [PubMed] [Google Scholar]
- 47.Bingham LJ, Tam MM, Palmer AM, Cahill JL, Nixon RL. Contact allergy and allergic contact dermatitis caused by lavender: a retrospective study from an Australian clinic. Contact Dermatitis. 2019;81(1):37-42. doi: 10.1111/cod.13247 [DOI] [PubMed] [Google Scholar]
- 48.Sugiura M, Hayakawa R, Kato Y, Sugiura K, Hashimoto R. Results of patch testing with lavender oil in Japan. Contact Dermatitis. 2000;43(3):157-160. doi: 10.1034/j.1600-0536.2000.043003157.x [DOI] [PubMed] [Google Scholar]
- 49.Boonchai W, Iamtharachai P, Sunthonpalin P. Occupational allergic contact dermatitis from essential oils in aromatherapists. Contact Dermatitis. 2007;56(3):181-182. doi: 10.1111/j.1600-0536.2007.01024.x [DOI] [PubMed] [Google Scholar]
- 50.Cousineau TM, Domar AD. Psychological impact of infertility. Best Pract Res Clin Obstet Gynaecol. 2007;21(2):293-308. doi: 10.1016/j.bpobgyn.2006.12.003 [DOI] [PubMed] [Google Scholar]
- 51.Porat-Katz A, Paltiel O, Kahane A, Eldar-Geva T. The effect of using complementary medicine on the infertility-specific quality of life of women undergoing in vitro fertilization. Int J Gynaecol Obstet. 2016;135(2):163-167. doi: 10.1016/j.ijgo.2016.05.011 [DOI] [PubMed] [Google Scholar]