Abstract
Background
Emergency appendectomy is often performed for de Garengeot hernia. However, in some cases, there may be a chance to perform an appendix-preserving elective surgery.
Case description
A 76-year-old woman presented to our hospital with complaints of a right inguinal swelling, which we diagnosed as a de Garengeot hernia using computed tomography (CT). B-mode ultrasonography (US) of the mass showed an appendix 4–6 mm in diameter with a clear wall structure; color Doppler US showed pulsatile blood flow signal in the appendiceal wall. Twenty-eight days later, herniorrhaphy with transabdominal preperitoneal repair (TAPP) was performed without appendectomy. Another 70-year-old woman presented to our hospital with complaints of a painful bulge in the right inguinal region. The diagnosis of de Garengeot hernia was made using CT. B-mode US showed an appendix 5 mm in diameter with a clear wall structure. Color Doppler US showed a pulsatile blood signal in the appendiceal wall. Seven days later, herniorrhaphy with TAPP was performed without appendectomy.
Conclusion
De Garengeot hernia is often associated with appendicitis; however, an appendix-preserving elective herniorrhaphy can be performed if US and intraoperative findings do not suggest appendicitis or circulatory compromise in the appendix.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40792-021-01329-x.
Keywords: De Garengeot hernia, Ultrasonography, Appendicitis, Elective surgery
Background
De Garengeot hernia is a femoral hernia that contains the appendix [1]; its incidence has been reported to be 0.15–5% of all femoral hernias [2–4]. Diagnosis is often difficult because of its rarity. Because de Garengeot hernia is often associated with appendicitis or circulatory compromise of the appendix, most surgeons perform emergent herniorrhaphy with appendectomy [5–7]; however, there may be a chance to perform an appendix-preserving elective surgery in certain situations. We report two cases of de Garengeot hernia that were preoperatively diagnosed and treated with elective herniorrhaphy without appendectomy. We have also highlighted the usefulness of ultrasonography (US) in the evaluation of inflammation and circulatory status of the appendix.
Case presentation
Case 1
A 76-year-old woman presented to our hospital with complaints of a right inguinal swelling. Her body temperature was 35.9 ℃, and the mass was not reducible. Blood tests showed a white blood cell (WBC) count of 3400/mm3, hemoglobin 11.9 g/dL, C-reactive protein (CRP) 0.02 mg/dL, albumin 3.7 g/dL, total bilirubin 0.7 mg/dL, blood urea nitrogen 16 mg/dL, and creatinine 0.76 mg/dL, which were not suggestive of an inflammatory reaction. Plain computed tomography (CT) (Fig. 1) revealed a well-defined, isodense, blind-ended tubular structure medial to the right femoral vein. B-mode ultrasonography (US) showed a blind-ended hyperechoic luminal structure protruding from the abdominal cavity (diameter: 4 mm at the body, 6 mm at the tip), a reticular hyperechoic area, and an anechoic area medial to the right femoral vein, which were determined to be the appendix, mesoappendix, and ascites, respectively (Fig. 2a). The appendiceal wall structure (five layers) was clearly visible. Color Doppler US showed pulsatile blood flow signals in the appendiceal wall (Fig. 2b, Additional file 1: video S1). CT and US indicated de Garengeot hernia; however, results of blood studies and US did not suggest appendicitis or appendiceal circulatory compromise. We planned an elective herniorrhaphy, which was performed using a transabdominal preperitoneal approach (TAPP), 28 days later.
Fig. 1.
Computed tomography (Case 1). a Axial image showing a well-defined isodense structure (Ap) on the medial side of the right femoral vein (FV). b Coronal image showing an isodense blind-ended tubular structure (Ap) on the medial side of the right FV protruding from the abdominal cavity. Ap appendix, FA femoral artery
Fig. 2.
Ultrasonography (US) (Case 1). a B-mode US showing a blind-ended hyperechoic luminal structure with five layers extending from the abdominal cavity (diameter: 4 mm at the body, 6 mm at the tip), a reticular hyperechoic area, and a hypoechoic area on the medial side of the right femoral vein. They were diagnosed as appendix (Ap), mesoappendix (M), and ascites (A), respectively. b Color doppler US showing pulsatile blood flow signals in the appendiceal wall
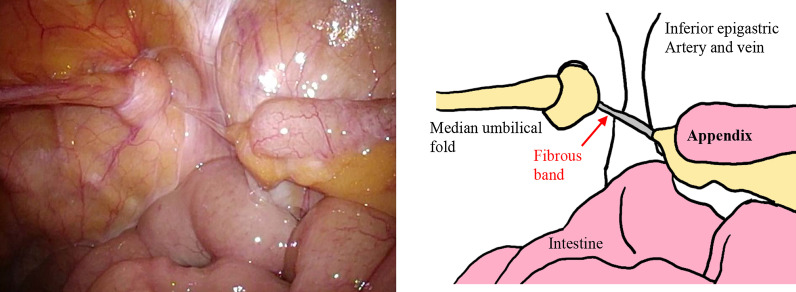
The patient was placed in the supine position under general anesthesia, and one 5-mm port each was placed on the umbilicus, umbilical level on the right side of the abdomen, and left lower abdomen. Laparoscopy showed incarceration of the median umbilical fold into the right femoral ring and the free appendix in the abdominal cavity (Fig. 3, Additional file 2: video S2). A fibrous band was also found between the right femoral ring and appendiceal tip, suggesting that the appendiceal tip had previously been in the femoral ring. There was no enlargement or color change in the appendix; therefore, appendectomy was not performed. The median umbilical fold was restored to the abdominal cavity, the peritoneum was incised, and parietalization was performed. Versatex mesh (Covidien) 14 cm × 9 cm was placed in the preperitoneal space and fixed with an Absorber Tack 5 mm (Covidien). The peritoneum was closed using continuous suturing with a 3–0 Polysorb (Covidien).
Fig. 3.
Laparoscopic image (Case 1). The median umbilical fold was incarcerated into the right femoral ring, and the appendix was present in the free abdominal cavity. There was no enlargement or color change in the appendix. A fibrous band was found between the right femoral ring and the appendiceal tip
She was discharged 2 days after the surgery and has shown no sign of hernia recurrence or appendicitis during the 6 months that have passed since the surgery.
Case 2
A 70-year-old woman presented to our hospital with complaints of right inguinal pain and swelling. A 3-cm inguinal mass was palpable; but not manually reducible. Blood test showed slightly elevated WBC count and CRP level (WBC 9500/mm3, CRP 2.23 mg/dL). Contrast-enhanced CT (Fig. 4) showed a blind-ended tubular structure, 6 mm in diameter and continuous with the cecum with contrast enhancement medial to the right femoral vein, suggesting that it was the appendix. B-mode US showed a blind-ended isoechoic structure (5 mm in diameter) which was continuous with the cecum, a surrounding reticular hyperechoic area, and an anechoic area medial to the right femoral vein, which were diagnosed as the appendix, mesoappendix, and ascites, respectively (Fig. 5a). B-mode US showed a clear appendiceal wall structure, and color Doppler US showed pulsatile blood flow signals in the appendiceal wall (Fig. 5b, Additional file 3: video S3). Based on these findings, she was diagnosed with de Garengeot hernia. Antibiotics (levofloxacin 500 mg/day) were administered to prevent potential development of appendicitis, and an elective surgery was performed seven days later.
Fig. 4.
Computed tomography (Case 2). a Axial image showing a well-defined structure 6 mm in diameter (Ap) with contrast enhancement on the medial side of the right femoral vein (FV). b Coronal image showing a tubular structure continuous with the cecum. Ap appendix, FA femoral artery
Fig. 5.
Ultrasonography (US) (Case 2). a B-mode US showing a blind-ended isoechoic tubular structure (5 mm in diameter) continuous with the cecum, a surrounding reticular hyperechoic area, and an anechoic area on the medial side of the right femoral vein. They were diagnosed as appendix (Ap), mesoappendix (M), and ascites (A), respectively. b Color doppler US showing pulsatile blood flow signals in the appendiceal wall
The patient was placed in the supine position under general anesthesia, and one 5-mm port each was placed on the umbilicus, umbilical level of the right side of the abdomen, and left lower abdomen. Laparoscopy revealed an incarcerated appendiceal tip in the right femoral ring, which was not reducible by traction (Fig. 6a, Additional file 4: video S4). The peritoneum was incised, and parietalization performed. The appendiceal tip was restored to the free abdominal cavity during ablation of the preperitoneal space. Because there was no enlargement, congestion, or color change in the appendix (Additional file 5: video S5), appendicectomy was not performed. Versatex mesh 14 cm × 9 cm (Covidien) was placed in the preperitoneal space and fixed with an Absorber Tack 5 mm (Covidien). The peritoneum was closed with continuous suturing using a 3–0 Polysorb (Covidien).
Fig. 6.
Laparoscopic image (Case 2). a The appendiceal tip was incarcerated in the right femoral ring. b The appendiceal tip was restored to the free abdominal cavity during ablation of the preperitoneal space. No enlargement, congestion, or color changes were noted in the appendix
The postoperative course was uneventful, and she has no signs of hernia recurrence or appendicitis 5 months postoperatively.
Discussion
Because de Garengeot hernia is a rare disease, it is often difficult to diagnose preoperatively. In addition, the disease is frequently associated with acute appendicitis, necessitating emergent herniorrhaphy and appendectomy [8–11]. But emergency surgery can impose social and psychological burden on patients. In the two abovementioned cases, we performed elective herniorrhaphy without appendectomy because the clinical US and intraoperative findings did not indicate significant inflammation or circulatory compromise in the appendix.
To the best of our knowledge, there have been nine cases of de Garengeot hernia wherein appendix-preserving herniorrhaphy was performed in English and Japanese literature (Table 1) [10, 12–14]. The median age was 76 years (range: 70–78 years), and all patients were female. At presentation, the median white blood cell count and CRP level were 4520/μL (range: 3400–9500) and 0.04 mg/dL (range: 0.02–2.23), respectively. Most cases were diagnosed as de Garengeot hernia using CT, and US was performed in three cases (including ours). In our two cases, B-mode US showed a clear appendiceal wall structure and no enlargement of the appendix, and color Doppler US showed pulsatile blood flow signals in the appendiceal wall, suggesting the absence of inflammation or circulatory compromise. In case 2, we anticipated the development of appendicitis because of the slightly elevated WBC and CRP levels, and therefore administered antibiotics. Elective surgery was performed 28 and seven days later in case 1 and 2, respectively. Among the nine cases with appendix-preserving herniorrhaphy, the anterior approach was used in seven cases, and TAPP in our two cases. The appendix was preserved on the basis of laparoscopic findings.
Table 1.
Reported cases of appendix preserving herniorrhaphy for de Garengeot hernia in English and Japanese literature
| No. | Year | Author | Country | Number of patients | Age | Sex | WBC count (/μl) | CRP (mg/dL) | Diagnosis of de Garengeot hernia by CT | US findings | Preoperative diagnosis of appendicitis | Duration between diagnosis and surgery | Intraoperative findings of the appendix | Surgical method |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 ~ 4 | 2007 | Sharma [10] | UK | 4 | nd | nd | nd | nd | nd | nd | Not diagnosed | < 10 h | Normal appendix | A |
| 5 | 2014 | Mizuno [12] | Japan | 1 | 70 | Female | 5000 | 0.04 | ( +) | Not performed | No | nd | Very slight inflammation of appendix | A |
| 6 | 2016 | Jin [13] | UK | 1 | 78 | Female | WNL | WNL | ( +) | A cystic mass and bowel loop within the hernia sac | Incarcerated appendix | Emergency surgery | A healthy appendix | A |
| 7 | 2020 | Uchida [14] | Japan | 1 | 78 | Female | 4040 | Negative | ( +) | Not performed | nd | nd | No inflammation | A |
| 8 | – | Case1 | Japan | 1 | 76 | Female | 3400 | 0.02 | ( +) | Normal diameter, and clear wall structure of the appendix. Color doppler showed pulsatile blood flow signals in the appendiceal wall | No | 28 days |
Gomes: Grade 1 Guenter: Class1 |
TAPP |
| 9 | – | Case2 | Japan | 1 | 70 | Female | 9500 | 2.23 | ( +) | Same as above | No | 7 days |
Gomes: Grade0 Guenter: Class1 |
TAPP |
A anterior approach, TAPP transabdominal preperitoneal approach, nd not described, WNL within normal limit
US and CT are highly useful because they can easily obtain tomographic images of the entire appendix. US is different from CT because it has a high spatial resolution and real-time capability, and can obtain tomographic images in any axis and evaluate vascularity using the color Doppler method although it depends on sonographers’ skill and experience. The US criteria for appendicitis include (1) enlargement of the appendix (> 6 mm), (2) maximum tenderness with a probe just above the appendix, (3) appendiceal wall thickness (≥ 3 mm), (4) loss of wall structure, (5) hyperechoic periappendiceal tissue, (6) periappendiceal fluid retention, (7) appendicolith, and (8) hypervascularity (early stage) or avascularity (necrotic stage) of the appendiceal wall [15, 16] (Table 2). The presence of complex periappendiceal fluid, as well as greater maximum appendiceal diameter and the presence of an appendicolith are significantly associated with perforation [17]. In this report, the US findings included an unswollen appendix, clear wall structure, and pulsatile blood signals, which suggested the absence of acute appendicitis and circulatory compromise.
Table 2.
US signs of acute appendicitis [16]
| Direct signs | Indirect signs |
|---|---|
| Non-compressibility of the appendix | Free fluid surrounding appendix |
| Perforation: appendix might be compressible | Local abscess formation |
| Diameter of the appendix > 6 mm | Increased echogenicity of local mesenteric fat |
| Single wall thickness ≥ 3 mm | Enlarged local mesenteric lymph nodes |
| Unclear wall structure | Thickening of the peritoneum |
| Hypoechoic fluid-filled lumen | Secondary small bowel obstruction |
| Hyperechoic mucosa/submucosa | |
| Hypoechoic muscularis layer | |
| Appendicolith: hyperechoic with posterior shadowing | |
| Colour Doppler and contrast-enhanced US: | |
| Hypervascularity in early stages of acute appendicitis | |
| Hypo- to avascularity in abscess and necrosis |
The indication for appendectomy during surgery for de Garengeot hernia should be determined based on intraoperative findings. Gomes et al. [18] and Guenther et al. [19] classified the severity of appendicitis based on intraoperative gross findings in the appendix (Tables 3 and 4). Case 1 and 2 corresponded to Grades 1 and 0 of the Gomes classification and Class 1 of the Guenther classification, respectively.
Table 3.
Laparoscopic grading system of acute appendicitis based on the gross findings of the appendix proposed by Gomes et al. [18]
| Grade | Laparoscopic findings |
|---|---|
| Grade 0 | Normal looking appendix |
| Grade 1 | Hyperemia and edema |
| Grade 2 | Fibrinous exudate |
| Grade 3A | Segmental necrosis |
| Grade 3B | Base necrosis |
| Grade 4A | Abscess |
| Grade 4B | Regional peritonitis |
| Grade 5 | Difuse peritonitis |
Table 4.
Classification of De Garengeot Hernia according to the gross appearance of the appendix proposed by Guenter et al. [19]
| Class | Description |
|---|---|
| Class 1 | Normal appearing appendix |
| Class 2 | |
| 2A | Erythematous, inflamed, or congested appendix |
| 2B | Erythematous, inflamed, or congested appendix |
| AND | |
| Erythema of the cecum or other segment of large or small intestine | |
| Class 3 | |
| 3A | Necrosis of the appendix, isolated to the tip |
| 3B | Necrosis of the appendix, involving the entire appendix |
| Class 4 | Necrosis of the appendix |
| AND | |
| Necrosis of the cecum or other segment of large or small intestine | |
| Class 5 | Perforated appendix, abscess, or fistula |
There is a risk of mesh infection when inflamed appendicitis is resected. After confirming that there is no appendiceal inflammation by laparoscopy, herniorrhaphy with mesh makes the surgery safer. Because the appendix is important to produce IgA and regulation of intestinal microflora [20, 21, 21], unnecessary appendectomy should be avoided.
When de Garengeot hernia is diagnosed, precise evaluation of inflammation and circulatory compromise in the appendix allows determination of the level of surgical emergency (emergency/elective). If the intraoperative findings do not show appendicitis or circulatory compromise, the appendix can be preserved.
Supplementary Information
Additional file 1: Video S1. Color Doppler US showed pulsatile blood flow signals in the appendiceal wall.
Additional file 2: Video S2. Laparoscopy showed incarceration of the median umbilical fold into the right femoral ring and the free appendix in the abdominal cavity. A fibrous band was also found between the right femoral ring and appendiceal tip, suggesting that the appendiceal tip had previously been in the femoral ring.
Additional file 3: Video S3. Color Doppler US showed pulsatile blood flow signals in the appendiceal wall.
Additional file 4: Video S4. Laparoscopy revealed an incarcerated appendiceal tip in the right femoral ring, which was not reducible by traction.
Additional file 5: Video S5. The appendiceal tip was restored to the free abdominal cavity during ablation of the preperitoneal space. There was no enlargement, congestion, or color change in the appendix.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Abbreviations
- CRP
C-reactive protein
- CT
Computed tomography
- TAPP
Transabdominal preperitoneal approach
- US
Ultrasonography
- WBC
White blood cell
Authors' contributions
HI was responsible for data collection and interpretation, and wrote the manuscript. NY helped draft the manuscript. KS and YK performed the diagnosis, surgery, general anesthesia, and perioperative management of the patient. All authors read and approved the final manuscript.
Funding
This work is supported by Japanese Red Cross Aichi Medical Center Nagoya Daiichi Hospital to HI (NFRCH 21-0013). The funder had no role in study design, data collection, data analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Informed consents were obtained from the patients for the publication of this case reports and any accompanying images.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nakayama T, Shiraishi K, Nishiumi T, Mori S, Isobe K, Furuta Y. A clinical study of femoral hernia. Surgery. 2004;66:211–215. [Google Scholar]
- 2.Yamamoto R, Shinozaki H, Kase K, Sasaki J, Kobayashi K. Clinical study on 44 cases of femoral hernia. J Abdom Emerg Med. 2012;32:19–23. [Google Scholar]
- 3.Sasaki T, Kameyama N, Tomita M, Mitsuhashi H, Matsumoto N, Obuchi T, Yoshikawa Y. Incarcerated and strangulated groin hernias: 37 cases in our hospital. J Abdom Emerg Med. 2012;32:1227–1230. [Google Scholar]
- 4.Koizumi M, Sata N, Taguchi M, Ksahara N, Ishiguro Y, Endo K, Sasanuma H, Sakuma Y, Shimizu A, Lefor A, Yasuda Y. Surgical evaluation of femoral hernia: a retrospective analysis. Jichi Med Univ J. 2012;35:87–91. [Google Scholar]
- 5.Watanabe M, Hayashi D. A clinical study on 47 cases of incarcerated femoral hernia. J Abdom Emerg Med. 2014;34:607–612. [Google Scholar]
- 6.Linder S, Linder G, Masson C. Treatment of de Garengeot’s hernia: a meta-analysis. Hernia. 2019;23:131–141. doi: 10.1007/s10029-018-1862-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akopian G, Alexander M. De Garengeot hernia; appendicitis within a femoral hernia. Am Surg. 2005;71:526–527. doi: 10.1177/000313480507100617. [DOI] [PubMed] [Google Scholar]
- 8.Priego P, Lobo E, Moreno I, Sanchez-Picot S, A Gil Olarte M, Alonso N, Fresneda V. Acute appendicitis in an incarcerated crural hernia: analysis of our experience. Rev Esp Enferm Dig. 2005;97:707–715 [DOI] [PubMed]
- 9.Gurer A, Ozdogan M, Ozlem N, Yildirim A, Kulacoglu H, Aydin R. Uncommon content in groin hernia sac. Hernia. 2006;10:152–155. doi: 10.1007/s10029-005-0036-4. [DOI] [PubMed] [Google Scholar]
- 10.Sharma H, Jha PK, Shekhawat NS, Memon B, Memon MA. De Garengeot hernia: an analysis of our experience. Hernia. 2007;11:235–238. doi: 10.1007/s10029-007-0208-5. [DOI] [PubMed] [Google Scholar]
- 11.Tsuruta S, Miyake H, Nagai H, Yoshioka Y, Yuasa N, Fujino M. Clinicopathological characteristics of de Garengeot hernia: six case reports and literature review. Surg Case Rep. 2021;7:14. doi: 10.1186/s40792-020-01098-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mizuno T, Kawabe A, Okamura T, Yamashita K, Isogai J, Suzuki K. A case of femoral hernia with incarceration of the appendix identified in abdominal CT. J Jpn Surg Assoc. 2014;75:1730–1734. doi: 10.3919/jjsa.75.1730. [DOI] [Google Scholar]
- 13.Jin Z, Imtiaz M, Nnajiuba H, Samlalsingh S, Ojo A. De Garengeot’s hernia: two case reports with correct preoperative identification of the vermiform appendix in the hernia. Case Rep Surg. 2016 doi: 10.1155/2016/2424657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uchida F, Shima Y, Nakatsukasa T, Tanoue Y, Hara R, Taniguchi Y, Fukuda T. A case of de Garengeot hernia, could be diagnosed by preoperative CT preserved appendix and repaired by using mesh. Surgery. 2020;82:79–82. [Google Scholar]
- 15.Hata J, Imamura Y, Manabe N, Kawai R, Naitou R, Kamata T, et al. Clinical imaging of appendiceal lesions: from the perspective of abdominal echocardiography. Stomach Intest. 2014;49:475–482. [Google Scholar]
- 16.Mostbeck G, Adam J, Nielsen M, Claudon M, Clevert D, Nicolau C, Nyhsen C, Owens C. How to diagnose acute appendicitis: ultrasound first. Insights Imaging. 2016;7:255–263. doi: 10.1007/s13244-016-0469-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carpenter J, Robert C, Zhang W, Lopez M, Mangona K, Guillerman P. Diagnostic performance of US for differentiating perforated from nonperforated pediatric appendicitis: a prospective cohort study. Radiology. 2017;282:3. doi: 10.1148/radiol.2016160175. [DOI] [PubMed] [Google Scholar]
- 18.Gomes C, Sartelli M, Saverio S, Ansaloni L, Catena F, Coccolini F, et al. Laparoscopy grading system of acute appendicitis: new insight for future trials. Surg Laparosc Endosc Percutan Tech. 2012;22:463–466. doi: 10.1097/SLE.0b013e318262edf1. [DOI] [PubMed] [Google Scholar]
- 19.Guenther T, Theodorou C, Grace N, Riderknecht T, Wiedeman J. De Garengeot hernia: a systematic review. Surg Endosc. 2021;35:503–513. doi: 10.1007/s00464-020-07934-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Masahata K, Umemoto E, Takeda K, et al. Generation of colonic IgA-secreting cells in the caecal patch. Nat Commun. 2014;10:3704. doi: 10.1038/ncomms4704. [DOI] [PubMed] [Google Scholar]
- 21.Sahami S, Kooij I, Van den Brink G, et al. The link between the appendix and ulcerative colitis: clinical relevance and potential immunological mechanisms. Am J Gastroenterol. 2016;111:163. doi: 10.1038/ajg.2015.301. [DOI] [PubMed] [Google Scholar]
- 22.Mathilde J, Merecedes G, Stephanie C, et al. The immunological functions of the appendix: an example of redundancy? Semin Immunol. 2018;36:31. doi: 10.1016/j.smim.2018.02.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Video S1. Color Doppler US showed pulsatile blood flow signals in the appendiceal wall.
Additional file 2: Video S2. Laparoscopy showed incarceration of the median umbilical fold into the right femoral ring and the free appendix in the abdominal cavity. A fibrous band was also found between the right femoral ring and appendiceal tip, suggesting that the appendiceal tip had previously been in the femoral ring.
Additional file 3: Video S3. Color Doppler US showed pulsatile blood flow signals in the appendiceal wall.
Additional file 4: Video S4. Laparoscopy revealed an incarcerated appendiceal tip in the right femoral ring, which was not reducible by traction.
Additional file 5: Video S5. The appendiceal tip was restored to the free abdominal cavity during ablation of the preperitoneal space. There was no enlargement, congestion, or color change in the appendix.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.