Abstract
Objectives:
To investigate the association between malocclusion/dentofacial anomalies and dental caries among adolescents.
Materials and Methods:
A cross-sectional study was conducted with 509 adolescents aged 11 to 14 years enrolled at public schools in the city of Osório in southern Brazil. Parents/caregivers answered a structured questionnaire on demographic and socioeconomic variables. A trained examiner recorded the presence of malocclusion (Dental Aesthetic Index [DAI]), traumatic dental injury, and dental caries. Data analysis involved the chi-square, Mann-Whitney, and Kruskal-Wallis tests. Poisson regression with robust variance was used for the multivariable analysis.
Results:
A total of 44.8% of the adolescents had dental caries (mean DFMT = 1.33 ± 1.84). The DAI index ranged from 15 to 77 (mean = 29.0 ± 7.9); 43.6% of the sample had severe malocclusion and 11.6% had traumatic dental injury. The prevalence and severity of dental caries were significantly greater among adolescents with severe malocclusion. The multivariate analysis demonstrated that adolescents with severe or handicapping malocclusion had a 31% greater probability of having dental caries (prevalence ratio: 1.31; 95% CI: 1.02–1.67), independently of demographic, socioeconomic, or clinical aspects. The orthodontic characteristics associated with the occurrence and severity of caries were maxillary irregularity ≥3 mm (P = .021) and abnormal molar relationship (P = .021).
Conclusions:
Handicapping malocclusion, maxillary irregularity, and abnormal molar relationship were associated with the occurrence and severity of dental caries. The findings suggest that the prevention and treatment of these conditions can contribute to a reduction in dental caries among adolescents.
Keywords: Malocclusion, Adolescent, Dental caries
INTRODUCTION
Dental caries is highly prevalent among adolescents and can exert an impact on quality of life.1–6 The development of cost-effective prevention strategies requires the recognition of risk factors.7 It is plausible that malocclusions contribute to the occurrence of caries by facilitating the accumulation of plaque and hindering its removal.8–9 Although studies have suggested such an association,8,10–12 there is no consistency in the findings, especially among investigations with an adequate sample size and the use of multivariable analysis. Moreover, most studies do not explore the influence of different dentofacial anomalies.8,10–13 In a systematic review of the literature on the relationship between dental crowding and caries, the authors found a lack of studies with adequate methodological quality to allow drawing clear conclusions regarding such an association.9
Clarifying the role of malocclusion and dentofacial anomalies in the occurrence of dental caries can assist in clinical decision making as well as establishing public health priorities. The Dental Aesthetic Index (DAI) is an adequate tool for this purpose. The DAI is used to classify malocclusions and orthodontic treatment needs and is integrated with the International Collaboration Study of Oral Health Outcomes of the World Health Organization (WHO).14
The aim of the present study was to investigate the association between malocclusion using the DAI and dental caries, considering demographic, socioeconomic, and clinical factors. The hypothesis is that severe forms of malocclusion exert an impact on the occurrence and severity of dental caries. A further aim was to explore associations between the various dentofacial anomalies and both the occurrence and severity of dental caries.
MATERIALS AND METHODS
Subject and Study Design
The present cross-sectional study is part of a project for evaluating oral health outcomes among adolescents enrolled at public schools in the City of Osório in southern Brazil. This city has a population of approximately 40,000 and a fluoridated public water supply. The source population was 1996 adolescents aged 11 to 14 years. The exclusion criterion was a current or past use of an orthodontic appliance.
The sample size was calculated based on an estimate of the relationship between malocclusion and quality of life, an 80% power, 95% level of confidence, mean score of 15.5 ± 12.2 on the Child Perceptions Questionnaire11–14 among adolescents with no need for orthodontic treatment (nonexposed), and 20.5 ± 16.9 among those with orthodontic treatment needs (exposed) and an exposed-to-nonexposed ratio of 1:3.15 As one-stage cluster sampling was employed, a 1.4 design effect was used to increase the precision of the study, leading to a minimum sample of 498 adolescents. Considering a possible 20% dropout rate and a prediction that 10% of adolescents would have a history of orthodontic appliance use, 700 adolescents were assessed for eligibility. All 12 public schools in the city of Osório constituted the cluster units, five of which were randomly selected following stratification based on size of the school (large [n = 1], medium [n = 2], and small [n = 2]) to obtain a representative sample.
Data Collection
The data were collected by a single examiner who had undergone training and calibration exercises. A questionnaire addressing demographic and socioeconomic data was administered to parents/caregivers, and the participants were submitted to a clinical dental examination.
Demographic and Socioeconomic Data
Parents/caregivers answered a structured questionnaire addressing the gender, age, and ethnicity of the adolescent, family structure (nuclear or nonnuclear), mother's schooling (completed years of study), and household income (income of all residents in the home and categorized based on the Brazilian monthly minimum wage [approximately US $240]). Ethnicity was defined by the parents/caregivers as white, brown, or black and was dichotomized as white or nonwhite.
Clinical Dental Exam
Examinations were performed at the schools with the adolescent seated in a chair. Malocclusion was evaluated based on the DAI, as recommended by WHO.16 This index involves evaluating parameters of dentofacial anomalies: missing teeth, crowding of the anterior segment, spacing in the anterior segment, diastema in the anterior segment, largest anterior maxillary irregularity, largest anterior mandibular irregularity, anterior maxillary overjet, anterior mandibular overjet, anterior open bite, and anteroposterior molar relationship. These parameters are scored separately, multiplied by a coefficient, and summed to generate the total score, allowing the categorization of normal occlusion or minor malocclusion (≤25 points), definite malocclusion with elective treatment need (26 to 30 points), severe malocclusion with highly desirable treatment need (31 to 35 points), and handicapping malocclusion for which treatment is required (≥36 points). Traumatic dental injury was used as a control variable and recorded based on the criteria proposed by Andreasen.17 The number of decayed, missing, and filled teeth (DMFT) was recorded using the criteria proposed by WHO.16 Intra-examiner agreement was determined using Kappa coefficients, which were 0.82, 0.92, and 1.00 for malocclusion, caries, and traumatic dental injury, respectively.
Data Analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS version 16.0; SPSS Inc, Chicago, Ill). The chi-square, Mann-Whitney, and Kruskal-Wallis tests were used to determine associations between dental caries and independent variables. Poisson regression with robust variance was used for calculating crude prevalence ratios (PRs). The multivariable model involved a hierarchical approach on three levels: (1) demographic variables (gender, age, and ethnicity of the adolescent); (2) socioeconomic variables (household income, family structure, and mother's schooling); and (3) clinical oral conditions (traumatic dental injury and malocclusion). The backward stepwise procedure was used to select variables on each level, eliminating variables with a P value greater than 0.20 one by one. In the final model, PRs were estimated for the variables selected after adjusting for those that remained in the multivariate model on the same and higher levels. The chi-square (categorical outcome variable), Kruskal-Wallis, and Mann-Whitney (quantitative outcome) tests were used to explore associations between dental caries and components of the DAI. A P value <.05 was indicative of statistical significance.
Ethical Considerations
This study received approval from the Human Research Ethics Committee of the Universidade Luterana do Brasil. Participation in the study was authorized by parents who signed a statement of informed consent.
RESULTS
The final sample was composed of 509 male and female adolescents aged 11 to 14 years (mean and standard deviation: 12.4 ± 1.1 years). Mother's schooling ranged from 0 to 16 years (mean: 6.9 ± 3.2 years). Most families had a nuclear structure (62.3%) and a household income of twice the monthly minimum wage (70.0%). The prevalence of traumatic dental injury was 11.6%. The DAI index ranged from 15 to 77 (mean = 29.0 ± 7.9). A total of 32.4% of the sample (165/509) had normal occlusion or mild malocclusion, 24.0% (122/509) had defined malocclusion, 21.6% (110/509) had severe malocclusion, and 22.0% (112/509) had handicapping malocclusion (Table 1). Thus, 43.6% of the adolescents had malocclusions for which treatment was either highly desirable or required (DAI ≥ 31).
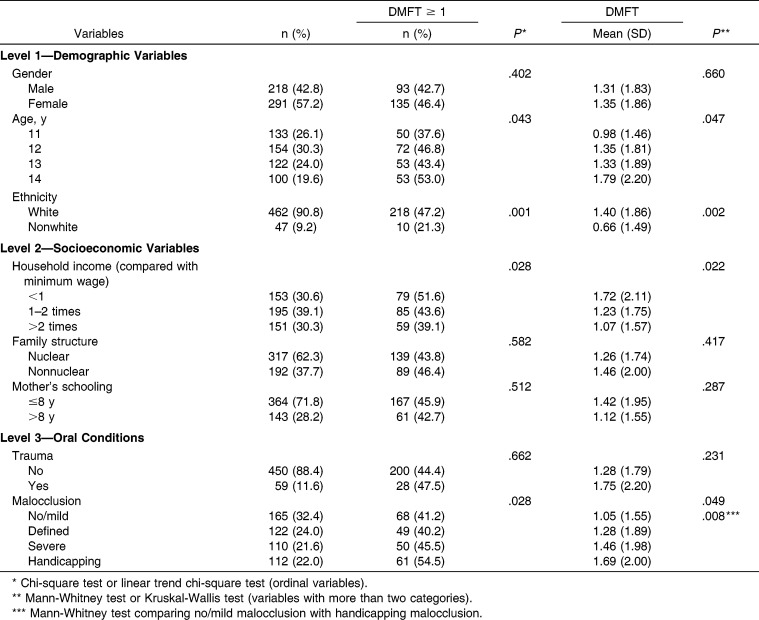
Table 1.
Absolute and Relative Frequencies of Dental Caries (DMFT) Among Adolescents According to Demographic, Socioeconomic, and Clinical Characteristics
The DMFT index ranged from 0 to 8 (mean = 1.33 ± 1.84; median = 0). A total of 228 adolescents (44.8%) had caries experience (DMFT ≥ 1). The prevalence and severity of caries were significantly greater among older adolescents, those ethnically classified as white, those from families with a lower household income, and those with greater malocclusion severity (Table 1).
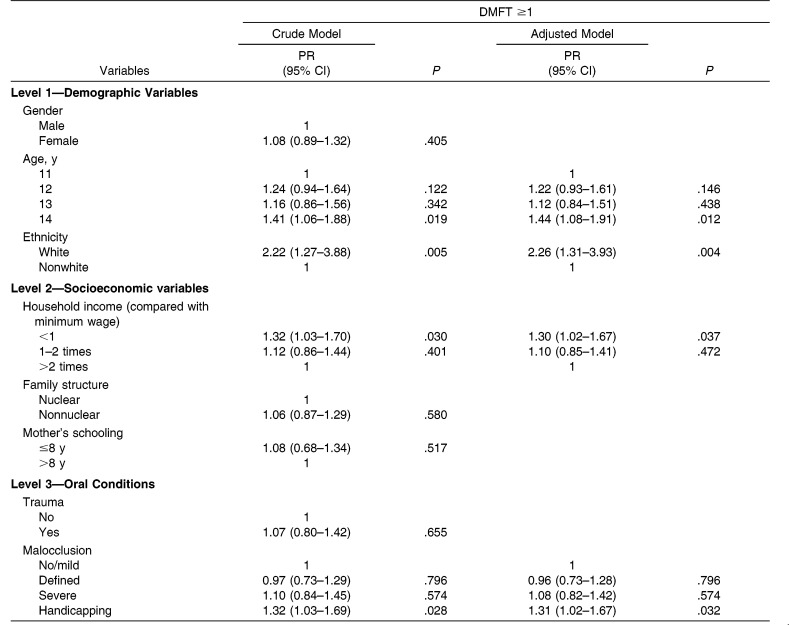
In the crude model, the same variables were associated with the outcome (Table 2). After adjustments for confounding variables, the occurrence of dental caries was 31% higher among adolescents with handicapping malocclusion than those having no malocclusion or mild malocclusion. The probability of caries experience was 44% higher among 14-year-olds compared with 12-year-olds, 2.2-fold higher among whites compared with nonwhites, and 30% higher among adolescents from families that earned less than the minimum wage compared with those from families that earned more than twice the minimum wage.
Table 2.
Crude and Adjusted Prevalence Ratios and 95% Confidence Intervals for History of Dental Caries Among Adolescents According to Demographic, Socioeconomic, and Clinical Characteristics
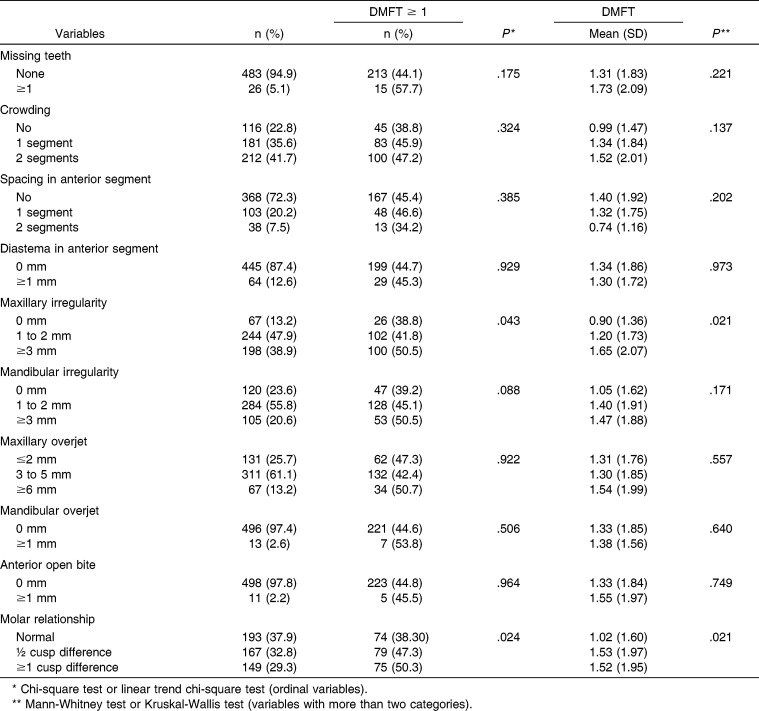
Table 3 shows that the occurrence of dental caries was significantly higher among adolescents with maxillary irregularity (P = .043) and those with an abnormal molar relationship (P = .024). Likewise, caries severity was significantly greater among adolescents with maxillary irregularity (P = .021) and those with a molar relationship with a difference of at least a half cusp (P = .021).
Table 3.
Absolute and Relative Frequencies of Dental Caries Experience (DMFT ≥ 1) and DMFT Index Among Adolescents According to Dentofacial Anomalies (DAI)
DISCUSSION
The main finding of our study was that malocclusion exerted an impact on the occurrence of dental caries independently of demographic, socioeconomic, and clinical aspects. Dental caries has a multifactorial etiology, and there is consensus in the literature that socioeconomic, behavioral, and biological aspects contribute substantially to its network of causality.18 The present findings demonstrate the significant participation of malocclusion in this process, which increased the likelihood of the occurrence of dental caries more than 30%. Furthermore, a clear dose-response effect was found, as an increase in the severity of dental caries (demonstrated by the DMFT index) was related to an increase in malocclusion severity and the need for orthodontic treatment. This association has also been reported in a previous study conducted with adolescents in India.12
Despite a tendency for investigations to indicate an association between malocclusion and caries,8,10–12 most studies have not addressed specific dentofacial anomalies.8,12 The term malocclusion encompasses a set of different conditions, and knowing which are related to the occurrence of caries is essential to guiding dental care. The recognition of an increased risk of caries as a result of certain traits of malocclusion would augment the indication for the orthodontic treatment of these traits.19 In the present study, maxillary irregularity and an abnormal molar relationship were the occlusal characteristics that contributed most to this association. Moreover, individuals with crowding, mandibular irregularity, maxillary and mandibular overjet, and anterior open bite also had greater caries severity in our study, although these associations did not achieve statistical significance. Previous studies describe greater caries experience among individuals with mandibular overjet and increased overbite in the mixed dentition20 as well as individuals with anterior segment crowding, accentuated maxillary overjet, and anterior open bite in the permanent dentition.12
There is no obvious explanation for why handicapping malocclusion, maxillary irregularity, and an abnormal molar relationship represent a greater likelihood of dental caries, but some speculations could be made. The development of caries occurs at sites in which biofilm remains for prolonged periods of time.21 It is plausible that the orthodontic conditions cited lead to a greater accumulation of plaque and hinder its removal. Collecting data on plaque level and hygiene habits in future studies could contribute toward clarifying this relationship. It is also possible that malocclusion and dental caries share common risk factors. Indeed, conditions such as myofascial dysfunction could lead to the development of caries and malocclusion in an independent fashion in the same individual.20 Social aspects inevitably exert an impact on biological factors and could also be a common cause of the two conditions. Although malocclusion is predominantly determined by genetics, some studies have found an association between socioeconomic status (SES) and this outcome in adolescents.13,22 Furthermore, the level of association between dental caries may vary according to the SES of the sample, suggesting that the relationship between these variables be assessed in a wider context of SES and background factors.23
Some investigators of this topic failed to perform multivariable analysis, indicating that the association found between malocclusion and caries was at least partially due to confounding variables. Although no significant change in estimates occurred after adjustment of the model in the present study, it should be pointed out that two demographic variables (age and ethnicity) and one socioeconomic variable (income) were associated with the outcome and represent potential confounding factors.
The possibility of reverse causality bias is a critical methodological aspect of the relationship between malocclusion and caries that constitutes a limitation in most studies investigating this issue, including the present study. This can occur when a cross-sectional design is employed, which does not allow the determination of the order of occurrence of these conditions. Most authors report their findings presupposing that malocclusion is the exposure factor and dental caries is the outcome. However, some studies report that adolescents with caries are more likely to exhibit some type of malocclusion.8,10–13 In practice, it is possible that the association occurs in both directions, as in the association between pacifier use and the interruption of breastfeeding.24 However, considering the fact that orthodontic conditions, such as an abnormal molar relationship, are established as soon as these teeth enter into occlusion and the fact that dental caries is a chronic disease that requires time to develop, malocclusion is expected to occur prior to dental caries in most adolescents. Prospective cohort studies are needed to clarify this issue.
Other possible limitations should be addressed. The DAI can underestimate the occurrence of malocclusion, as it does not include all occlusal traits.23 However, this index is recommended by WHO and has been widely employed in epidemiological studies. Second, approximately 20% of the adolescents eligible for the study refused to participate. However, it is unlikely that selection bias had occurred, since a previously reported sensitivity analysis found no significant differences between analyzed and nonanalyzed individuals with regard to age or ethnicity.25 Moreover, it is unlikely that the fact that exposure and the outcome were recorded by a single examiner led to measurement bias, as malocclusion was defined based on objective scores; furthermore, knowledge of exposure does not greatly affect the measurement of a hard outcome.26
The implications of these findings underscore the need for dentists to evaluate clinical conditions in a comprehensive fashion. Understanding that malocclusion and orthodontic characteristics are indicators for the occurrence of dental caries constitutes an additional factor beyond esthetics to indicate orthodontic treatment in children and adolescents, especially when malocclusion is more severe, which is more perceptible, thus exerting a negative impact on oral health–related quality of life. Such care involves the prevention and early treatment of malocclusion in the primary and mixed dentition phases as soon as it is possible. As malocclusion can have a negative effect on quality of life25,27–28 and is a risk factor for dental caries, early prevention and treatment represent actions addressing common risk factors that seem to constitute the best health promotion strategy.29
The findings of the present study can be generalized to populations with similar cultural and demographic characteristics to populations in southern Brazil, such as varied socioeconomic levels in a predominantly white population living in a developing country. It is possible that the strength of the association between malocclusion and dental caries may be even greater in populations having a higher exposure factor or outcome.
CONCLUSIONS
Malocclusion exerted an impact on the occurrence of dental caries independently of demographic, socioeconomic, and clinical characteristics.
Maxillary irregularity and an abnormal molar relationship were the dentofacial anomalies associated with a greater occurrence and severity of caries in adolescents aged 11 to 14 years.
The findings suggest that early prevention and treatment of malocclusion might reduce the prevalence and severity of adolescent caries, a possibility that should be investigated in future cohort studies.
REFERENCES
- 1.Piovesan C, Antunes JL, Guedes RS, Ardenghi TM. Impact of socioeconomic and clinical factors on child oral health related quality of life (COHRQoL) Qual Life Res. 2010;19:1359–1366. doi: 10.1007/s11136-010-9692-7. [DOI] [PubMed] [Google Scholar]
- 2.Martins-Júnior PA, Vieira-Andrade RG, Corrêa-Faria P, Oliveira-Ferreira F, Marques LS, Ramos-Jorge ML. Impact of early childhood caries on the oral health-related quality of life of preschool children and their parents. Caries Res. 2013;47:211–218. doi: 10.1159/000345534. [DOI] [PubMed] [Google Scholar]
- 3.Alves LS, Damé-Teixeir N, Susin C, Maltz M. Association among quality of life, dental caries treatment and intraoral distribution in 12-year-old South Brazilian schoolchildren. Community Dent Oral Epidemiol. 2013;41:22–29. doi: 10.1111/j.1600-0528.2012.00707.x. [DOI] [PubMed] [Google Scholar]
- 4.Gomes MC, Pinto-Sarmento TC, Costa EM, Martins CC, Granville-Garcia AF, Paiva SM. Impact of oral health conditions on the quality of life of preschool children and their families: a cross-sectional study. Health Qual Life Outcomes. 2014;12:55. doi: 10.1186/1477-7525-12-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freire MCM, Reis SCGB, Figueiredo N, Peres KG, Moreira RS, Antunes JLF. Individual and contextual determinants of dental caries in Brazilian 12-year-olds in 2010. Rev Saúde Pública. 2013;47:1–10. doi: 10.1590/s0034-8910.2013047004322. [DOI] [PubMed] [Google Scholar]
- 6.Ministério da Saúde. Secretaria de Atenção à Saúde. Secretaria de Vigilância em Saúde. Departamento de Atenção Básica. SBBrasil 2010—Pesquisa Nacional de Saúde Bucal. 2011:92. < http://dab.saude.gov.br/CNSB/sbbrasil/arquivos/projeto_sb2010_relatorio_final.pdf. [Google Scholar]
- 7.Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century—the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2003;31(suppl 1):3–23. doi: 10.1046/j..2003.com122.x. [DOI] [PubMed] [Google Scholar]
- 8.Gábris K, Márton S, Madléna M. Prevalence of malocclusions in Hungarian adolescents. Eur J Orthod. 2006;2:467–470. doi: 10.1093/ejo/cjl027. [DOI] [PubMed] [Google Scholar]
- 9.Hafez HS, Shaarawy SM, Al-Sakiti AA, Mostafa YA. Dental crowding as caries risk factors: a systematic review. Am J Orthod Dentofacial Orthop. 2012;142:443–450. doi: 10.1016/j.ajodo.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 10.Nobile CGA, Paiva M, Fortunato L, Angelillo IF. Prevalence and factors related to malocclusion and orthodontic treatment need in children and adolescents in Italy. Eur J Public Health. 2007;17:637–641. doi: 10.1093/eurpub/ckm016. [DOI] [PubMed] [Google Scholar]
- 11.Mtaya M, Brudvil P, AФm AN. Prevalence of malocclusion and its relationship with socio-demographic factors, dental caries, and oral hygiene in 12- to 14-year-old Tanzanian schoolchildren. Eur J Orthod. 2009;31:467–476. doi: 10.1093/ejo/cjn125. [DOI] [PubMed] [Google Scholar]
- 12.Singh A, Purohit B, Sequeira P, Acharya S, Bhat M. Malocclusion and orthodontic treatment need measured by the dental aesthetic index and its association with dental caries in Indian schoolchildren. Community Dent Health. 2011;28:313–316. [PubMed] [Google Scholar]
- 13.Frazão P, Narvai PC. Socio-environmental factors associated with dental occlusion in adolescents. Am J Orthod Dent Orthop. 2006;129:809–816. doi: 10.1016/j.ajodo.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organisation (WHO) International Collaboration Study of Oral Health Outcomes (ICS II) Document 2 Oral Data Collection and Examination Criteria. Geneva: WHO; 1989. [Google Scholar]
- 15.Foster-Page LA, Thomson WM, Jokovic A, Locker D. Epidemiological evaluations of short-form versions of the Child Perception Questionnaire. Eur J Oral Sci. 2008;116:538–544. doi: 10.1111/j.1600-0722.2008.00579.x. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. The World Oral Health Report 2003 Continuous Improvement of Oral Health in the 21st Century—The Approach of the WHO Global Oral Health Programme. Geneva: WHO; 2003. [DOI] [PubMed] [Google Scholar]
- 17.Andreasen JO, Andreasen FM, Bakland LK, Flores MT. Traumatic Dental Injuries A Manual. 2nd ed. Oxford: Blackwell; 2003. [Google Scholar]
- 18.Walsh T, Worthington HV, Glenny AM, Appelbe P, Marinho VC, Shi X. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2010;1:CD007868. doi: 10.1002/14651858.CD007868.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Helms S, Petersen PE. Causal relation between malocclusion and caries. Acta Odontol Scand. 1989;47:217–222. doi: 10.3109/00016358909007704. [DOI] [PubMed] [Google Scholar]
- 20.Stahl F, Grabowski R. Malocclusion and caries prevalence: is there a connection in the primary and mixed dentitions. Clin Oral Invest. 2004;8:86–90. doi: 10.1007/s00784-003-0244-1. [DOI] [PubMed] [Google Scholar]
- 21.Fejerskov O. Changing paradigms in concepts on dental caries: consequences for oral health care. Caries Res. 2004;38:182–191. doi: 10.1159/000077753. [DOI] [PubMed] [Google Scholar]
- 22.Borzabadi-Farahani A, Eslamipour F, Asgari I. Association between orthodontic treatment need and caries experience. Acta Odontol Scand. 2011;69:2–11. doi: 10.3109/00016357.2010.516732. [DOI] [PubMed] [Google Scholar]
- 23.Borzabadi-Farahani A. A review of the evidence supporting the aesthetic orthodontic treatment need indices. Prog Orthod. 2012;13:304–313. doi: 10.1016/j.pio.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 24.Feldens CA, Vitolo MR, Rauber F, Cruz LN, Hilgert JB. Risk factors for discontinuing breastfeeding in southern Brazil: a survival analysis. Maternal and Child Health Journal. 2012;16:1257–1265. doi: 10.1007/s10995-011-0885-7. [DOI] [PubMed] [Google Scholar]
- 25.Scapini A, Feldens CA, Ardenghi TM, Kramer PF. Malocclusion impacts adolescents' oral health related quality of life. Angle Orthod. 2012;85:512–518. doi: 10.2319/062012-509.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schulz KF, Grimes DA. Blinding in randomized trials: hiding who got what. Lancet. 2002;359:696–700. doi: 10.1016/S0140-6736(02)07816-9. [DOI] [PubMed] [Google Scholar]
- 27.Ukra A, Foster Page LA, Thomson WM, Farella M, Tawse Smith A, Beck V. Impact of malocclusion on quality of life among New Zealand adolescents. NZ Dent J. 2013;109:18–23. [PubMed] [Google Scholar]
- 28.Dawoodbhoya I, Delgado-Angulob EK, Bernabé E. Impact of malocclusion on the quality of life of Saudi children. Angle Orthod. 2013;83:1043–1048. doi: 10.2319/012713-83.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol. 2000;28:399–406. doi: 10.1034/j.1600-0528.2000.028006399.x. [DOI] [PubMed] [Google Scholar]