Abstract
Purpose
To evaluate the relationship between mortality or relapse of bloodstream infection (BSI) due to Enterococcus faecalis and infectious diseases specialist consultation (IDC) and other factors potentially associated with outcomes.
Methods
In a tertiary-care center, consecutive adult patients with E. faecalis BSI between January 1, 2016 and January 31, 2019, were prospectively followed. The management of E. faecalis BSI was evaluated in terms of adherence to evidence-based quality-of-care indicators (QCIs). IDC and other factors potentially associated with 90-day-mortality or relapse of E. faecalis BSI were analyzed by multivariate logistic regression.
Results
A total of 151 patients with a median age of 68 years were studied. IDC was performed in 38% of patients with E. faecalis BSI. 30 cases of endocarditis (20%) were diagnosed. All-cause in-hospital mortality was 23%, 90-day mortality was 37%, and 90-day relapsing E. faecalis BSI was 8%. IDC was significantly associated with better adherence to 5 QCIs. Factors significantly associated with 90-day mortality or relapsing EfB in multivariate analysis were severe sepsis or septic shock at onset (HR 4.32, CI 2.36e7.88) and deep-seated focus of infection (superficial focus HR 0.33, CI 0.14e0.76).
Conclusion
Enterococcus faecalis bacteremia is associated with a high mortality. IDC contributed to improved diagnostic and therapeutic management.
Keywords: E. faecalis, Bloodstream infection, ID consultation
Introduction
Enterococcus spp. are important causes of both community- and hospital-acquired bloodstream infections and account for 10% of endocarditis cases worldwide [1]. Incidence of E. faecalis BSI (EfB) has been estimated to be ~ 4.5 per 100,000 annually and case fatality between 10 and 20% [2, 3].
EfB has been described as a clinical entity with different risk factors, clinical features, and microbiological characteristics than other enterococcal BSIs [2]. Specifically, EfB occurs in less seriously ill patients, has lower rates of antibiotic resistance, and is more often associated with endocarditis. E. faecalis causes both native valve and prosthetic valve endocarditis, while E. faecium endocarditis remains a rare entity [1].
The optimal management of E. faecalis invasive infections is still not clearly defined and data concerning the risk of developing endocarditis are divergent. In a recent study, Dahl et al. found that infective endocarditis (IE) was diagnosed 1 out of 4 patients with EfB who systematically received echocardiography [4].
Infectious diseases specialist consultation (IDC) as a strategy to improve the quality of care has been investigated in other difficult-to-treat infections such as Staphylococcus aureus bloodstream infection and candidemia. In these studies, IDC led to better adherence to diagnostic and management standards, and was associated with lower mortality [5–12].
Recent investigations described the role of IDC in management of enterococcal BSI, suggesting that IDC consultations are associated with a greater likelihood of elimination of bacteremia [13] and improved outcome [14–16]. In the present paper, we evaluated the epidemiology, clinical characteristics, and outcomes of patients with EfB admitted to our hospital between January 1, 2016, and January 31, 2019, with a focus on the impact of ID specialist consultation on diagnostic work-up and outcome.
Patients and methods
Setting, case identification, and study design
The study was conducted from January 1, 2016, to January 31, 2019, at the Medical Center of the University of Freiburg, Germany, a 1600-bed tertiary-care center with 73,000 admissions and 824,000 outpatient contacts per year. Consecutive adult patients with clinical evidence of infection and blood cultures growing E. faecalis were prospectively included and followed for at least 90 days. Identification and susceptibility testing of all blood culture isolates was performed according to standard protocols.
Data collection
The following data were recorded for each patient: age, sex, underlying disease, comorbidity according to the Charlson Comorbidity Index, date of hospital admission, stay or admission to an intensive care unit (ICU), and clinical parameters at EfB onset. Initial portal of entry of EfB, main focus, diagnostic investigations, antimicrobial therapy, and outcomes were documented. The data were retrieved directly or electronically from clinical charts and reports including diagnostic (e.g., laboratory, microbiological, or radiographic) studies. All patients were followed during their hospital stay and for at least 90 days after onset. Mortality, hospital readmissions, and relapsing infection were assessed by reviewing medical records of our institution and/or seeing the patient in the infectious disease (ID) outpatient department.
The Institutional Review Board of the University Medical Center Freiburg considered the collection of routine data as evaluation of service and waived the need for written informed consent.
Definitions
The day of sampling the first blood culture positive for E. faecalis was considered the date of EfB onset. Community-acquired EfB was considered as EfB diagnosed before, at, or within 48 h after hospital admission. Healthcare-associated EfB was defined as EfB within 48 h of admission in an outpatient with (1) close healthcare contact or (2) hospitalization for 2 or more days within 90 days or (3) continuous residency in a nursing home before EfB. All other EfB cases were defined as hospital acquired. ICU admission was defined between 24 h before and 48 h after onset. The focus of infection was defined as a focal infection with typical signs or symptoms of infection, isolation of E. faecalis at the site of infection, and/or imaging results compatible with focal infection. Catheters were considered as the source of EfB if both central line and peripheral blood cultures were growing E. faecalis, and catheter tip cultures grew E. faecalis as well. Endocarditis was diagnosed according to the modified Duke criteria [17]. Severe neutropenia was defined as an absolute neutrophil count of less than 500/mL. We considered severe immunosuppression in the presence of primary immunodeficiency disorders, uncontrolled disease in HIV-positive patients, high-dose steroid therapy, and immunosuppressive combination therapy with two or more drugs with different mode of action, hematopoietic stem cell transplantation within the past 6 months, and solid organ transplant. Infections of a removable catheter and uncomplicated urinary infections were considered as superficial foci. Biliary tract and other intraabdominal infections, spondylodiscitis, osteomyelitis, and endocarditis were considered deep-seated foci. Embolization was defined by signs on clinical examination or by findings using imaging techniques. EfB were considered complicated if any of the following criteria were present: severe sepsis/septic shock within 24 h before or after onset, persistent positive blood cultures, presence of deep-seated focus (for example, undrained abscess, empyema, and osteomyelitis) or endocarditis, need of surgical or non-invasive intervention, presence of a non-removable foreign body or an intravascular device (prosthetic joint, prosthetic heart valve, implantable electronic cardiac devices, long term intravascular catheter, and vascular prosthesis), and local spread of infection. Persistent positive blood cultures were defined as the continued presence of E. faecalis in blood cultures at day 3 or later after beginning of effective therapy. Relapse of bacteremia was defined as the isolation of E. faecalis (with the same resistance profile) from blood cultures within 90 days after EfB onset and following end of treatment for the initial episode.
Infectious disease (ID) specialist consultation and quality-of-care indicators
An ID service has been established in our hospital since 2002. IDCs for EfB are performed on request of the primary physician in charge. IDC comprised chart review and physical examination of the patient with written recommendations for diagnostic work-up, therapy, and follow-up examinations based on established guidelines, literature review, and individual case discussions with the physicians in charge. During the 3-year study period, senior consultants of the ID service did not change. To evaluate the impact of IDC on the management of EfB, we identified five evidence-based quality-of-care indicators (QCIs) based on clinical experience and extrapolated from the literature [14, 15, 18], which were defined according to Table 1.
Table 1.
Definition of quality-of-care indicators
| Quality of care indicator | Definition |
|---|---|
| Follow-up blood cultures | Performance of control blood cultures 48–96 h after onset of bacteraemia, regardless of clinical evolution |
| Early source control | Removal of non-permanent vascular catheter whenever the catheter was suspected or confirmed as the source of EfB, or eradication/drainage of a deep-seated focus (e.g., drainage of abscess, stent placement in case of ureter or biliary obstruction) within 48–72 h |
| Echocardiography in patients at risk of endocarditis | Performance of echocardiography especially in patients with complicated bacteraemia or other predisposing conditions for endocarditis such as community-acquired EfB or unknown origin of bacteraemia |
| Appropriate definitive therapy |
Definitive therapy with intravenous ampicillin (at least 2 g every 6 h or adjusted to renal function a), or Definitive combination therapy in patients with endocarditis, endovascular prosthesis infection or osteomyelitis, or Definitive therapy with the narrowest antimicrobial spectrum in case of polymicrobial bacteraemiab, started within 72–96 h after EfB onset |
| Treatment duration according to the complexity of infection | Duration of antimicrobial therapy for 3–7 days for uncomplicated bacteraemia, 7–14 days for uncomplicated bacteraemia with presence of non-removable intravascular device, ≥ 42 days in case of suspected or confirmed endocarditis |
aDosing was adjusted to renal function according to the Stanford Health Care Antimicrobial Dosing Reference Guide [19].
bAdequate antimicrobial monotherapy was defined as administration of a cell wall-active agent [a b-lactam (agent of first choice: ampicillin)]. Combination therapy was defined as adequate monotherapy plus additional administration of gentamicin (standard dose 3 mg/kg/24 h i.v. or i.m. or adjusted to renal function) or ceftriaxone (2 mg/12 h i.v. or i.m. or adjusted to renal function). For patients with polymicrobial bacteremia, adequate antimicrobial therapy was defined as administration of daptomycin, linezolid, ampicillin/sulbactam, or piperacillin/tazobactam. In polymicrobial bacteremia with the presence of S. aureus, additional therapy with flucloxacillin or cefazolin was considered adequate
Study endpoints
The primary endpoint of the study was death or relapsing EfB within 90 days. Secondary endpoint was all-cause in-hospital mortality and the adherence to quality-of-care indicators in EfB patients.
Statistical methods
Continuous variables were summarized with medians and interquartile ranges (IQR) and categorical variables with frequencies and percentages. Proportions were compared using the Pearson χ2, medians using the Wilcoxon rank‐sum test.
We investigated the effect of various patient characteristics and IDC on mortality or relapse of EfB 90 days after onset. The hazard risk for death or relapsing infection [along with the 95% confidence interval (CI)] was estimated with a Cox regression with inclusion of variables known to be relevant for the outcome. A sensitivity analysis was conducted using a propensity score-adjusted Cox regression. The propensity score for ID consultation was based on age, sex, Charlson score, ICU admission at onset, mode of acquisition, endocarditis or deep-seated focus, and presence of intravascular device or foreign body. In addition, severe sepsis or septic shock at onset was included in the Cox regression. ID consultation was expressed as time-dependent covariable for avoiding immortal time bias. A p value of < 0.05 was considered statistically significant in all analyses.
Statistical analyses were performed with IBM SPSS Statistics 25.0 and STATA version 12.1 (StataCorp; College Station, TX, United States of America).
Results
Clinical features
As shown in the study flowchart (Fig. 1), 164 consecutive adult patients with clinical evidence of infection and blood cultures growing E. faecalis were identified during the 3-year period. Patients with central line colonization (n = 13) without a positive peripheral blood culture and no sign or symptoms of infection were not included. A total of 151 patients with a median age of 68 years were eligible for inclusion in the study. Patient characteristics are shown in Table 2. 60 (40%) patients suffered from polymicrobial bloodstream infections. 64 (42%) required ICU admission. Malignancies including hematological and solid tumors (65, 43%), chronic renal failure (45, 30%), and diabetes mellitus (39, 26%) were the most common underlying conditions. 78 (52%) of infections were hospital-acquired and 34 (23%) healthcare-related. All 151 E. faecalis isolates were susceptible to ampicillin and vancomycin. High-level gentamicin resistance was detected in 45 (30%) isolates. In 36 (24%) patients, the portal of entry was unknown. Among the hospital-acquired infections, intravascular devices, and surgical interventions (23%, respectively) were the most common source of EfB. Healthcare-associated and community-acquired infections showed high rates of biliary tract (27% and 20%, respectively) and urinary tract infections (27% and 15%, respectively) (data not shown). 30 cases of endocarditis (20%) were diagnosed.
Fig. 1.
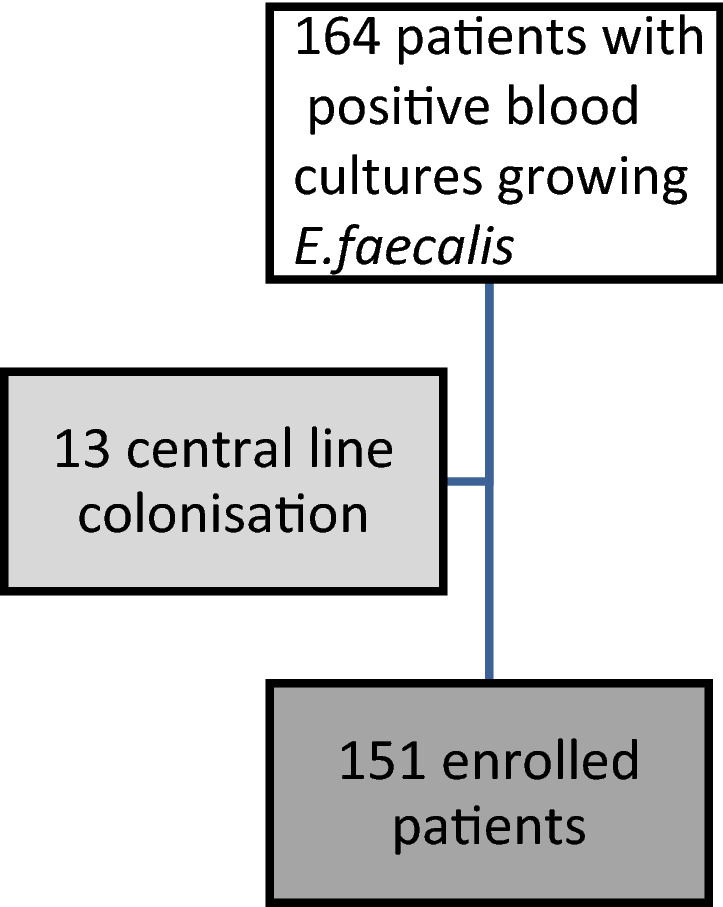
Study flowchart
Table 2.
Epidemiological, clinical characteristic, and outcomes of 151 patients with E. faecalis bacteremia
| Variable | All patients n = 151 |
ID consultation n = 58 |
No ID consultation n = 93 |
p value |
|---|---|---|---|---|
| Median age (IQR) | 68 (59–78) | 72,5 (60–80) | 68 (57–77) | 0.12 |
| Female sex | 41 (27%) | 11 (19%) | 30 (32%) | 0.07 |
| Charlson index ≥ 5 | 37 (24%) | 18 (44%) | 19 (20%) | 0.14 |
| ICU admission | 64 (42%) | 23 (40%) | 41 (44%) | 0.59 |
| Polymicrobial BSI | 60 (40%) | 19 (32%) | 41 (44%) | 0.17 |
| Underlying conditions | ||||
| ^Diabetes mellitus | 39 (26%) | 18 (31%) | 21 (23%) | 0.22 |
| ^Chronic renal disease | 45 (30%) | 23 (40%) | 22 (24%) | 0.04 |
| ^Chronic liver disease | 15 (10%) | 5 (9%) | 10 (11%) | 0.25 |
| ^Malignancy | 65 (43%) | 15 (26%) | 50 (54%) | 0.002 |
| ^Pacemaker | 20 (13%) | 13 (22%) | 7 (8%) | 0.009 |
| ^Prosthetic heart valve | 25 (17%) | 18 (31%) | 7 (8%) | < 0.001 |
| ^Intravenous drug abuse | 4 (3%) | 2 (3%) | 2 (2%) | 0.63 |
| ^Severe neutropenia | 2 (1%) | 0 | 2 (2%) | 1.30 |
| ^Severe immunosuppression | 20 (13%) | 6 (10%) | 14 (15%) | 0.40 |
| Acquisition | ||||
| ^Hospital-acquired | 78 (52%) | 26 (45%) | 52 (56%) | 0.18 |
| ^Community-acquired | 39 (26%) | 23 (39%) | 16 (17%) | 0.001 |
| ^Healthcare-associated | 34 (23%) | 9 (16%) | 25 (27%) | 0.06 |
| Complicated bacteraemiaa | 106 (70%) | 50 (86%) | 56 (60%) | 0.001 |
| ^Hemodynamic instability/shock | 28 (19%) | 10 (17%) | 18 (19%) | 0.75 |
| ^Persistent positive blood culture | 15 (10%) | 11 (19%) | 4 (4%) | 0.004 |
| ^Endocarditis or deep-seated focus | 82 (54%) | 39 (67%) | 43 (46%) | 0.045 |
| ^Intravascular device or foreign body | 39 (26%) | 26 (45%) | 13 (14%) | < 0.001 |
| Portal of entry | ||||
| ^Unknown | 36 (24%) | 25 (43%) | 11 (12%) | < 0.001 |
| ^Intravascular device | 25 (17%) | 11 (19%) | 14 (15%) | 0.53 |
| ^Abdominal surgery | 24 (16%) | 3 (5%) | 21 (23%) | 0.004 |
| ^Biliary tract or stent | 23 (15%) | 5 (9%) | 18 (19%) | 0.07 |
| ^Urinary tract | 21 (14%) | 3 (5%) | 18 (19%) | 0.07 |
| ^Gastrointestinal tract | 15 (10%) | 9 (16%) | 6 (6%) | 0.14 |
| ^others | 7 (4%) | 2 (3%) | 5 (5%) | 0.79 |
| Main focus | ||||
| ^Unknown | 23 (15%) | 9 (15%) | 14 (14%) | 0.94 |
| ^Intravascular device | 20 (13%) | 7 (12%) | 13 (14%) | 0.74 |
| ^Endocarditis | 30 (20%) | 30 (52%) | 0 | < 0.001 |
| ^Left (native) | 14 (47%) | 14 (47%) | ||
| ^Left (prosthetic) | 12 (40%) | 12 (40%) | ||
| ^Right (native) | 1 (3%) | 1 (3%) | ||
| ^Pacemaker | 3 (10%) | 3 (10%) | ||
| ^Osteomyelitis/ | 3 (2%) | 1 (2%) | 2 (2%) | 0.85 |
| ^Spondylodiscitis | ||||
| ^Biliary tract/stent | 25 (17%) | 5 (9%) | 20 (22%) | 0.38 |
| ^Other intraabdominal focus | 24 (16%) | 3 (5%) | 21 (23%) | 0.004 |
| ^Urinary tract | 21 (14%) | 2 (3%) | 19 (20%) | 0.003 |
| ^Others | 5 (3%) | 1 (2%) | 4 (4%) | 0.39 |
| Outcome | ||||
| All-cause in-hospital mortality | 35 (23%) | 12 (21%) | 23 (25%) | 0.57 |
| 90-day mortality | 43 (37%) | 16 (37%) | 27 (38%) | 0.95 |
| Relapse of E. faecalis BSI | 9 (8%) | 0 | 9 (13%) | 0.05 |
aMore than one complication is possible in each patient
Overall, ID physicians were involved in 58 (38%) of EfB cases. IDC were performed during the first week after EfB onset (median 3 days). Patients in the IDC group had more frequently chronic renal failure, higher presence of pacemaker, or prosthetic heart valve, and suffered more frequently from complicated bacteremia (86% vs 60%). Malignancy was more frequently found in the non-IDC group (54 vs 26%) (Table 2).
Outcomes
All-cause in-hospital mortality was 23% (35 of 151 patients). Of the patients who survived, 48% were discharged home, 25% were transferred to other medical facilities, and 3% were discharged to a nursing home. 36 patients were lost to follow-up before day 90 after onset. Death within 90 days after EfB onset was reported in 43 of the 115 evaluable patients (37%). No significant difference of in-hospital and 90-day-mortality was observed between the IDC and no-IDC group. Relapsing within 90 days was observed in 9 patients (8%), all of which in the non-IDC group.
Adherence to quality-of-care indicators
As shown in Table 3, follow-up blood culture (91% vs. 52%, p < 0.001) and echocardiography (84% vs. 25%, p < 0.001) were more frequently performed in the IDC group. The source of bacteremia was better controlled in patients followed by an ID specialist (89% vs 65%, p = 0.001). In the IDC group, early appropriate definitive therapy was more frequently prescribed (78% vs 30%, p < 0.001) and the duration of treatment was more frequently appropriate according to the complexity of infection (76% vs 43%, p = 0.001).
Table 3.
Adherence to quality-of-care indicators in 151 patients with E. faecalis bacteremia, with and without ID consultation
| Quality-of-care indicators | Tot | ID consultation n = 58 |
No ID consultation n = 93 |
RR for adherence to QCI (95% CI) | p value |
|---|---|---|---|---|---|
| Follow-up blood cultures | 105 | 53 (91%) | 52 (56%) | 1.63 (1.34–1.99) | < 0.001 |
| Early source/focus control | 100 | 50 (89%) | 50 (65%) | 1.37 (1.14–1.66) | 0.001 |
| Echocardiography | 72 | 49 (84%) | 23 (25%) | 3.41 (2.36–4.95) | < 0.001 |
| Use of intravenous ampicillin as definitive therapy | 72 | 45 (78%) | 27 (30%) | 2.61 (1.85–3.69) | < 0.001 |
| Adequate treatment duration | 83 | 44 (76%) | 39 (43%) | 1.77 (1.34–2.35) | 0.001 |
A p value of < 0.05 was considered statistically significant
Factors associated with death or recurrence within 90 days
To evaluate the impact of factors potentially associated with death or relapse of EfB, a univariate and a multivariate analyses were performed in a Cox regression model; results are shown in Table 4. Severe sepsis or septic shock within 24 h before or after onset (HR 4.05, CI 2.30–7.15; HR 4.32, CI 2.36–7.88) and deep-seated focus of infection (superficial focus HR 0.38, CI 0.17–0.86; HR 0.33, CI 0.14–0.76) were significantly associated with mortality and recurrence of bacteremia within 90 days, both in univariate and multivariate analyses. The mortality was higher in patients with hospital-acquired and healthcare-associated EfB, but the difference was not significant. Also, IDC was associated with survival or relapse of EfB with an adjusted HR of 0.87 (0.45–1.66) that was not statistically significant. The propensity score-adjusted Cox regression supported the results of the multivariate analysis and did not show an impact of IDC on mortality (Table 5).
Table 4.
Univariate and multivariate analyses of characteristics and factors potentially associated with death or relapse within 90 days in 151 cases of E. faecalis bacteremia
| Variable | Subgroup | Mortality or recurrence of bacteraemia after 90 days | |||||
|---|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | ||||||
| HR | 95% CI | p value | HR | 95% CI | p value | ||
| Sex | Male | 1 | 1 | 0.87 | |||
| Female | 0.95 | 0.52–1.75 | 0.87 | 0.95 | 0.50–1.80 | ||
| Age (years) | 1.004 | 0.99–1.03 | 0.63 | 1.01 | 0.99–1.04 | 0.30 | |
| Charlson Score ≥ 5 | 1.27 | 0.70–2.31 | 0.44 | 1.00 | 0.5–1.98 | 0.99 | |
| Severe sepsis or septic shock at onset | 4.05 | 2.30–7.15 | < 0.001 | 4.32 | 2.36–7.88 | < 0.001 | |
| Main infection focus | 0.031 | 0.027 | |||||
| Deep-seated focus | 1 | 1 | |||||
| Unknown focus | 1.004 | 0.47–2.16 | 0.99 | 1.18 | 0.49–2.82 | 0.72 | |
| Superficial focus | 0.38 | 0.17–0.86 | 0.02 | 0.33 | 0.14–0.76 | 0.009 | |
| Mode of acquisition | 0.44 | 0.19 | |||||
| Community-acquired | 1 | 1 | |||||
| Hospital-acquired | 1.31 | 0.66–2.61 | 0.43 | 1.37 | 0.62–3.01 | 0.44 | |
| Healthcare-associated | 1.64 | 0.76–3.51 | 0.20 | 2.14 | 0.92–5.00 | 0.08 | |
| ID specialist consultation | 0.92 | 0.49–1.73 | 0.80 | 0.87 | 0.45–1.66 | 0.66 | |
IDC is expressed as time-dependent covariable
Table 5.
Propensity score-adjusted Cox regression. IDC is expressed as time-dependent covariable
| Variable | Multivariate analysis | ||
|---|---|---|---|
| HR | 95% CI | p value | |
| Propensity scorea | 0.67 | 0.20–2.24 | 0.52 |
| Severe sepsis or septic shock at onset | 4.00 | 2.25–7.07 | < 0.001 |
| ID specialist consultation | 0.95 | 0.50–1.79 | 0.87 |
aThe propensity score for ID consultation was based on age, sex, Charlson score, ICU admission at onset, mode of acquisition, endocarditis or deep-seated focus, and presence of intravascular device or foreign body
Discussion
The key findings of this study were that among EfB patients severe sepsis/septic shock and deep-seated infection are strongly associated with mortality or relapse, whereas IDC as performed in our center resulted in improved diagnostic management and antimicrobial therapy, but its impact on 90-day mortality or relapse was uncertain.
Clinical epidemiological findings in this study were comparable to those reported in the other studies from different parts of the world [2, 3, 20, 21]. In our study, we found a higher frequency of infectious endocarditis (IE) (20%) than in some previous studies [3, 15, 22] but comparable to recent findings of a Danish study reporting endocarditis in 26% of the EfB patients [4]. Fernández-Hidalgo et al. reported an increase of Ef-IE of 10% from 2000 to 2018, with Ef-IE accounting for 23% of all endocarditis cases [22]. These results show that patients with EfB are at high risk of IE and underline the importance of performing echocardiography, especially in patients with predisposing conditions for IE, unknown focus, and persistent positive blood cultures. Our case collection was based in a tertiary-care center with an endocarditis team and a cardiovascular surgery department; this may have introduced a referral bias toward a selection of more severe cases. This may also explain the slightly higher mortality compared to several previous studies [2, 3].
An ID service has been established in our hospital since 2002; in 2018, ~ 2000 consultations were performed by our consultation service. During the period of the study, ID physicians were involved in 38% EfB cases on request of the primary physician in charge. Many previous studies evaluated the role of an expert consultation service in S. aureus bacteremia, where the high risk of IE and invasive infection is well known [23–27]. A previous work from our group suggested better diagnostic management, more adequate treatment, and lower mortality rate of patients with S. aureus bacteremia followed by IDC [5]. In this study, IDC significantly contributed to better therapeutic decision, but did not significantly impact on 90-day mortality or EfB-relapse in the multivariate analysis, even though relapsing EfB was observed only in the non-IDC group. A propensity score for ID consultation was calculated considering demographic factors (age, sex), comorbidities (Charlson score), ICU admission at onset as a proxy of severity of illness, and factors that showed a statistical different distribution among the IDC and non-IDC group. However, the propensity score-adjusted Cox regression supported the results of the multivariate analysis. The most likely explanations are the small study population, further unmeasured confounding, and the high prevalence of complex underlying conditions making survival as an endpoint perhaps insensitive for the range of possible improved outcomes. Previous studies described IE as leading cause of recurrent EfB [15]. In this study, endocarditis was diagnosed in 52% of patients followed by IDC; therefore, the absence of relapse in all IDC-patients is noteworthy. We believe that a better adherence to important practice guidelines and recommendations for management of Ef-IE played a major role.
To our knowledge, a few studies evaluated the impact of IDC on management and outcome in enterococcal bacteremia. A recent study from Italy assessed the impact of ID consultation in 368 patients with monomicrobial enterococcal bacteremia, showing an improved 30-day and 1-year mortality in the IDC group. In accordance to our findings, they reported more frequent adequate therapy, echocardiography, and follow-up blood cultures in patients visited by an ID specialist [15]. Similarly, Lee et al. reported better diagnostic management associated with IDC in 205 patients with enterococcal bacteremia. A lower all-cause 30-day mortality was associated with IDC in this study; however, IDC did not impact on 90-day mortality [16].
A recent investigation from Japan evaluated the impact of IDC on enterococcal bacteremia in children; ID consultations were significantly associated with appropriate empiric and definitive therapy, appropriate treatment duration, and lower risk of 1-year mortality [28]. Zasowski et al. reported that IDC within 24 h was significantly associated with a lower risk for delayed appropriate therapy, and therefore with a lower 30-day mortality in 190 patients with enterococcal BSI [14]. Jindai et al. found that blood culture sterilization occurred more frequently when IDC was obtained [13].
In this study, we specifically focused on management of E. faecalis bacteremia, and we evaluated the impact of IDC in terms of quality of diagnostic work-up, quality of therapy, and outcome. As EfB has been less investigated in this respect, we based our choice of quality-of-care indicators on our previous clinical experience and on established recommendations for treatment of EfB. Since both EfB and S. aureus BSI are connected with a high risk of endocarditis [1], we extrapolate the QCIs from those established for S. aureus infections [18]. Our findings underline that expert advice can lead to a better adherence to guidelines, to a more detailed evaluation, early effective therapy, and appropriate treatment duration.
Of note is that we focused on bloodstream infection due to E. faecalis and did not include other enterococci. E. faecalis and E. faecium are considered two different bacterial species and may be associated with different clinical syndromes. E. faecium endocarditis, for example, is rare [2], and E. faecium may be associated with different underlying diseases and risk factors. A limitation of this study is its single-center nature. Moreover, some information were missing in clinical charts and reports and some of the relevant data may have been missed during review of the medical records. Patient follow-up after discharge was incomplete, and 36 patients were lost to follow up before day 90 after onset; therefore, we may have missed deaths and recurrences. In addition, the two groups of patients with and without IDC had comparable demographic characteristics, but differed regarding relevant clinical findings and underlying conditions. Polymicrobial bacteremia was included in this study and concomitant bacteria may have contributed to mortality. Finally, we evaluated overall mortality rather than attributable mortality, which, however, is difficult to determine.
Conclusion
In our study, we observed a relative high mortality of patients with EfB, which may be related to underlying conditions and severe manifestations, as the study was conducted at a tertiary-care referral center. Endocarditis is a frequent condition in patients with EfB and echocardiography should be included in the diagnostic work-up. IDC contributed to an improved diagnostic and therapeutic management of patients with EfB. No relapsing EfB within 90 days was observed in patients followed by an ID specialist.
Author contributions
CC, SR, and WVK conceptualized the study. CC, MM, SR, and WVK were consultants of the ID service. CC acquired data for the article. BB performed microbiological studies. CC, MM, and GS performed statistical analysis. CC wrote the manuscript and did the review of the literature. SR, BB, MM, and WVK revised the article critically for important intellectual content. CC, SR, BB, MM, and WVK gave final approval for the article to be published.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
Not applicable.
Declarations
Conflict of interest
We declare no competing interests.
References
- 1.Cahill TJ, Prendergast BD. Infective endocarditis. Lancet. 2016;387(10021):882–893. doi: 10.1016/S0140-6736(15)00067-7. [DOI] [PubMed] [Google Scholar]
- 2.Billington EO, Phang SH, Gregson DB, Pitout JD, Ross T, Church DL, et al. Incidence, risk factors, and outcomes for Enterococcus spp. blood stream infections: a population-based study. Int J Infect Dis. 2014;26:76–82. doi: 10.1016/j.ijid.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 3.Noskin GA, Peterson LR, Warren JR. Enterococcus faecium and Enterococcus faecalis bacteremia: acquisition and outcome. Clin Infect Dis. 1995;20(2):296–301. doi: 10.1093/clinids/20.2.296. [DOI] [PubMed] [Google Scholar]
- 4.Dahl A, Iversen K, Tonder N, Hoest N, Arpi M, Dalsgaard M, et al. Prevalence of infective endocarditis in Enterococcus faecalis bacteremia. J Am Coll Cardiol. 2019;74(2):193–201. doi: 10.1016/j.jacc.2019.04.059. [DOI] [PubMed] [Google Scholar]
- 5.Rieg S, Küpper MF. Infectious diseases consultations can make the difference: a brief review and a plea for more infectious diseases specialists in Germany. Infection. 2016;44(2):159–166. doi: 10.1007/s15010-016-0883-1. [DOI] [PubMed] [Google Scholar]
- 6.Fowler VG, Sanders LL, Sexton DJ, Kong L, Marr KA, Gopal AK, et al. Outcome of Staphylococcus aureus bacteremia according to compliance with recommendations of infectious diseases specialists: experience with 244 patients. Clin Infect Dis. 1998;27(3):478–486. doi: 10.1086/514686. [DOI] [PubMed] [Google Scholar]
- 7.Jenkins TC, Price CS, Sabel AL, Mehler PS, Burman WJ. Impact of routine infectious diseases service consultation on the evaluation, management, and outcomes of Staphylococcus aureus bacteremia. Clin Infect Dis. 2008;46(7):1000–1008. doi: 10.1086/529190. [DOI] [PubMed] [Google Scholar]
- 8.Kaech C, Elzi L, Sendi P, Frei R, Laifer G, Bassetti S, et al. Course and outcome of Staphylococcus aureus bacteraemia: a retrospective analysis of 308 episodes in a Swiss tertiary-care centre. Clin Microbiol Infect. 2006;12(4):345–352. doi: 10.1111/j.1469-0691.2005.01359.x. [DOI] [PubMed] [Google Scholar]
- 9.Mylotte JM, Tayara A. Staphylococcus aureus bacteremia: predictors of 30-day mortality in a large cohort. Clin Infect Dis. 2000;31(5):1170–1174. doi: 10.1086/317421. [DOI] [PubMed] [Google Scholar]
- 10.Djelic L, Andany N, Craig J, Daneman N, Simor A, Leis JA. Automatic notification and infectious diseases consultation for patients with Staphylococcus aureus bacteremia. Diagn Microbiol Infect Dis. 2018;91(3):282–283. doi: 10.1016/j.diagmicrobio.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Buehrle K, Pisano J, Han Z, Pettit NN. Guideline compliance and clinical outcomes among patients with Staphylococcus aureus bacteremia with infectious diseases consultation in addition to antimicrobial stewardship-directed review. Am J Infect Control. 2017;45(7):713–716. doi: 10.1016/j.ajic.2017.02.030. [DOI] [PubMed] [Google Scholar]
- 12.Turner RB, Valcarlos E, Won R, Chang E, Schwartz J. Impact of infectious diseases consultation on clinical outcomes of patients with Staphylococcus aureus bacteremia in a community health system. Antimicrob Agents Chemother. 2016;60(10):5682–5687. doi: 10.1128/AAC.00439-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jindai K, Strerath MS, Hess T, Safdar N. Is a single positive blood culture for Enterococcus species representative of infection or contamination? Eur J Clin Microbiol Infect Dis. 2014;33(11):1995–2003. doi: 10.1007/s10096-014-2167-y. [DOI] [PubMed] [Google Scholar]
- 14.Zasowski EJ, Claeys KC, Lagnf AM, Davis SL, Rybak MJ. Time is of the essence: the impact of delayed antibiotic therapy on patient outcomes in hospital-onset enterococcal bloodstream infections. Clin Infect Dis. 2016;62(10):1242–1250. doi: 10.1093/cid/ciw110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bartoletti M, Tedeschi S, Scudeller L, Pascale R, Rosselli Del Turco E, Trapani F, et al. Impact on mortality of a bundle for the management of enterococcal bloodstream infection. Open Forum Infect Dis. 2019;6(12):ofz473. doi: 10.1093/ofid/ofz473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee RA, Vo DT, Zurko JC, Griffin RL, Rodriguez JM, Camins BC. Infectious diseases consultation is associated with decreased mortality in enterococcal bloodstream infections. Open Forum Infect Dis. 2020;7(3):ofaa064. doi: 10.1093/ofid/ofaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG, Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30(4):633–638. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- 18.López-Cortés LE, Del Toro MD, Gálvez-Acebal J, Bereciartua-Bastarrica E, Fariñas MC, Sanz-Franco M, et al. Impact of an evidence-based bundle intervention in the quality-of-care management and outcome of Staphylococcus aureus bacteremia. Clin Infect Dis. 2013;57(9):1225–1233. doi: 10.1093/cid/cit499. [DOI] [PubMed] [Google Scholar]
- 19.Stanford health care antimicrobial dosing reference guide. https://med.stanford.edu/bugsanddrugs.htlm.
- 20.Cabiltes I, Coghill S, Bowe SJ, Athan E. Enterococcal bacteraemia “Silent but deadly”: a population-based cohort study. Intern Med J. 2020;50(4):434-440. 10.1111/imj.14396 [DOI] [PubMed]
- 21.Suppli M, Aabenhus R, Harboe ZB, Andersen LP, Tvede M, Jensen JU. Mortality in enterococcal bloodstream infections increases with inappropriate antimicrobial therapy. Clin Microbiol Infect. 2011;17(7):1078–1083. doi: 10.1111/j.1469-0691.2010.03394.x. [DOI] [PubMed] [Google Scholar]
- 22.Fernández-Hidalgo N, Escolà-Vergé L. Enterococcus faecalis bacteremia: consider an echocardiography, but consult an infectious diseases specialist. J Am Coll Cardiol. 2019;74(2):202–204. doi: 10.1016/j.jacc.2019.03.526. [DOI] [PubMed] [Google Scholar]
- 23.Falcone M, Russo A, Venditti M. Optimizing antibiotic therapy of bacteremia and endocarditis due to staphylococci and enterococci: new insights and evidence from the literature. J Infect Chemother. 2015;21(5):330–339. doi: 10.1016/j.jiac.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 24.Fernández-Hidalgo N, Almirante B, Gavaldà J, Gurgui M, Peña C, de Alarcón A, et al. Ampicillin plus ceftriaxone is as effective as ampicillin plus gentamicin for treating Enterococcus faecalis infective endocarditis. Clin Infect Dis. 2013;56(9):1261–1268. doi: 10.1093/cid/cit052. [DOI] [PubMed] [Google Scholar]
- 25.Gavaldà J, Len O, Miró JM, Muñoz P, Montejo M, Alarcón A, et al. Brief communication: treatment of Enterococcus faecalis endocarditis with ampicillin plus ceftriaxone. Ann Intern Med. 2007;146(8):574–579. doi: 10.7326/0003-4819-146-8-200704170-00008. [DOI] [PubMed] [Google Scholar]
- 26.Pericas JM, Cervera C, del Rio A, Moreno A, Garcia de la Maria C, Almela M, et al. Changes in the treatment of Enterococcus faecalis infective endocarditis in Spain in the last 15 years: from ampicillin plus gentamicin to ampicillin plus ceftriaxone. Clin Microbiol Infect. 2014;20(12):O1075–O1083. doi: 10.1111/1469-0691.12756. [DOI] [PubMed] [Google Scholar]
- 27.Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. 2015 ESC guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM) Eur Heart J. 2015;36(44):3075–3128. doi: 10.1093/eurheartj/ehv319. [DOI] [PubMed] [Google Scholar]
- 28.Furuichi M, Horikoshi Y, Miyairi I. Infectious diseases consultation improves treatment and decreases mortality by enterococcal bacteremia in children. Pediatr Infect Dis J. 2018;37(9):856–860. doi: 10.1097/INF.0000000000001919. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


