Abstract
This study examined the disease‐specific quality of life (QoL) in lipoedema patients undergoing treatment for the condition with liposuction. We conducted a retrospective analysis of all patients (n = 69) who underwent liposuction for treatment of lipoedema between 2004 and 2019, and gathered data on patient age, body mass index, the number of liposuction sessions, and the amount of fat removed per side. The study also prospectively evaluated the QoL in 20 lipoedema patients before and after liposuction using the Freiburg Life Quality Assessment for lymphatic diseases questionnaire. The mean age was 50.6 ± 12.8 years, and the average number of liposuction sessions performed was 2.9 ± 1.9, with a mean volume of 1868 ± 885.5 mL of fat removed per side. Before treatment with liposuction, disease‐specific QoL in patients with lipoedema was low on every single subscale as well as on the global score and showed a significant improvement in all aspects after liposuction. There was a significant correlation between a higher number of liposuction treatment sessions and general health status in lipoedema patients (P = .007). Liposuction greatly improves the QoL in lipoedema patients. A higher number of liposuction treatment sessions seem to have a positive effect on general health status in these patients.
Keywords: lipoedema, lipolymphoedema, liposuction, lymphoedema, quality of life
1. INTRODUCTION
The term lipoedema describes a chronic condition featuring bilaterally distributed, abnormally large deposits of subcutaneous fat in the upper or lower extremities. 1 The disease is progressive and almost exclusively affects women. 2 The prevalence of lipoedema is still not known for certain, although the estimated incidence of one in nine adult women found by an older unpublished epidemiological study 3 is routinely cited in the literature on lipoedema.
The condition is well described, and a definition of lipoedema as code EF02.2 has been proposed for the 11th Revision of the International Classification of Diseases (ICD‐11), 4 which is set to take effect in 2022. The German version of the ICD‐10 includes separate codes for lipoedema stage I, II, II, and other, or unspecified lipoedema. 5 However, misdiagnoses still seem to be the rule rather than the exception, mostly due to lack of information and awareness about this disease. 2 , 6 , 7 , 8
In the lower extremities, the condition is associated with considerable pain, pressure, easy bruising, and tenderness, which does not respond to weight loss. 9 Patients often report steadily reduced daily activity levels and a high psychosocial burden, in conjunction with low levels of self‐esteem due to high degree of aesthetic deformity. 7 , 10 Left untreated patients with lipoedema may develop secondary lymphoedema, depression, 11 anxiety, 9 and eventually become immobilised. 12
The aetiology of the disease is yet unknown and curative treatment for lipoedema does not exist. 13 Current treatment strategies focus on pain relief and reduction of disproportionate swelling through either conservative or surgical treatment. Conservative treatment includes lifestyle counselling, weight control regimens, exercise, gentle compression, and combined decongestive therapy. 1 Although conservative treatment can alleviate symptoms in early stages of lipoedema, the benefits are often temporary. 2 , 7
In recent years, surgical treatment of lipoedema with tumescent liposuction technique to remove excess fat tissue has produced good long‐term results with very low complication rates. 14 , 15 , 16 In many patients, conservative therapy could be reduced or stopped altogether. 17 The Dutch guidelines on lipoedema recommend that tumescent liposuction should be considered the treatment of choice for patients with a favourable health profile and/or inadequate response to conservative and supportive measures. However, the guidelines that lacked reporting the quality of supporting evidence and strength of recommendations were not provided. 18 A recent review by the Canadian Agency for Drugs and Technologies in Health with five included studies found limited evidence that liposuction seemed to be beneficial in lipoedema patients. 19 Furthermore, a prospective study with 38 patients undergoing aesthetic liposuction using a self‐developed, indication‐specific questionnaire found a significant improvement in quality of life (QoL) in general, in addition to improved body image, emotional stability, and reduction in overall psychological distress. 20
In many countries, liposuction treatment is not covered by many medical insurance policies because it is generally considered a “cosmetic” intervention. In Germany, the joint federal committee of physicians and health insurance companies has reached a provisional 4‐year agreement for insurance coverage of liposuction. Liposuction treatment based on tumescent technique and including multiple sessions, if necessary, is currently covered in stage III lipoedema patients with bulging fat deposits until December of 2024. 21
Although numerous studies have shown positive effects from liposuction in lipoedema patients such as pain relief, improved mobility, and higher levels of self‐esteem, 13 , 15 , 16 , 17 , 22 there is currently still no specific instrument available to assess lipoedema‐related outcomes. In the past, these studies have collected clinical data on patient outcomes using the visual analogue scale and other standardised questionnaires, but we were unable to identify any studies examining the effect of liposuction on health‐related QoL using a validated questionnaire. The aim of this study was, therefore, to evaluate changes in the disease‐specific QoL in lipoedema patients undergoing liposuction treatment using a validated questionnaire.
2. PATIENTS AND METHODS
2.1. Patients
We conducted a two‐part study of 69 female patients having liposuction on the lower extremity for stage 3 lipoedema between January 2004 and August 2019 at the Department for Plastic and Aesthetic, Reconstructive and Hand Surgery at the AGAPLESION Markus Hospital in Frankfurt am Main, Germany. Tumescent, lymph‐sparing liposuction was performed on the lower extremity according to the guidelines of the German Society of Phlebology, and under local anaesthesia, in most lipoedema patients. 1 Some patients received general anaesthesia additionally due to psychological reasons. We obtained written informed consent from all patients for the liposuction procedure.
The first part of the study was a retrospective analysis examining parameters such as patient age, weight before and after liposuction, body mass index (BMI), number of liposuction sessions, amount of fat removed per side, and mean amount of fat removed per side. The second part of the study was a prospective pilot study of the QoL associated with liposuction for the treatment of lipoedema in the last consecutive 20 patients treated at our centre.
The inclusion criteria were as follows:
female
diagnosis of lipoedema between January 2004 and August 2019
aged 16 to 85 years
stage 3 lipoedema with bulging fat deposits
unsuccessful conservative therapy (>1 year)
liposuction treatment coverage by statutory health insurance
informed consent for the liposuction procedure
Patients were excluded if they had:
lipoedema stage 1 or 2
liposuction purely for aesthetic reasons
Additionally, we excluded pilot study patients if they were unwilling or unable to fill out the health‐related QoL questionnaire. We delivered the questionnaire to pilot study participants immediately before surgery and at the 6‐month follow‐up post surgery. Data on the variables mentioned earlier were extracted from all patients' records.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were followed for the reporting of this study. The study protocol is in accordance with the ethical guidelines of the 1975 Declaration of Helsinki.The ethics committee of the federal states' Medical Association approved the research protocol.
2.2. Health‐related QoL assessment
We assessed health‐related QoL in 20 patients using the short version of the Freiburg Life Quality Assessment in its disease‐specific variant for lymphatic diseases (FLQA‐lk). Both the original 92‐item questionnaire and the short form have shown high internal consistency and convergent validity for patients with lymphatic diseases. 23 , 24 The short version of the disease‐specific variant consists of 30 items in five different subscales and three visual analogue scales. Each of the five subscales physical complaints, daily life, social life, emotional well‐being, and therapy of lymphatic disorder includes six questions to be answered on a five‐point Likert scale ranging from 1 (best QoL) to 5 (worst QoL). Scoring was performed on a single item basis and included an additional global score, with one equalling the best QoL and five being the worst QoL. The three visual analogue scales feature numeric scales for general health status, health status concerning lymphatic disease and QoL, each ranging from 0 (very poor) to 10 (very good), as part of the global assessment of generic QoL in the last week.
2.3. Data analysis
Owing to the explorative nature of this study, data analysis was mostly based on descriptive statistics, with all data being reported as mean ± standard deviation (SD) and minimum to maximum ranges. The FLQA‐lk data are presented as mean ± SD (range) of total scores and for subscales. The t‐test for paired samples or Wilcoxon's signed‐rank tests were mainly used to examine differences in FLQA‐lk before and after surgery. Spearman's rank correlation coefficient was calculated for the correlation analyses between FLQA‐lk and BMI, the number of liposuction sessions or the total amount of fat removed per side, and then tested for significant differences from zero. A P value of <.05 was defined as being statistically significant.
3. RESULTS
3.1. Patient characteristics
A total of 69 female patients underwent liposuction for treatment of lipoedema at our centre between January 2004 and August 2019, after having exhausted all conservative therapy options. The mean age was 50.6 ± 12.8 years at the time of surgery, and the average BMI was 33.4 ± 7.1. The average number of liposuction sessions performed was 2.9 ± 1.9, with some women needing as few as one or as many as 12 sessions. The mean volume of fat removed per side was 1868 ± 885.5 mL. An overview of the patients' demographic and descriptive data is presented in Table 1.
TABLE 1.
Demographic and descriptive data
| Number of patients (n) | Mean ± SD | Range | |
|---|---|---|---|
| Age (years) | 69 | 50.6 ± 12.8 | 24 ± 58 |
| BMI (kg/m2) | 56 | 33.4 ± 7.1 | 22.0 ± 50.5 |
| Number of liposuction sessions | 69 | 2.9 ± 1.9 | 1 ± 12 |
| Total liposuction volume/side (mL) | 69 | 5133.0 ± 3868.3 | 150 ± 23 250 |
| Mean liposuction volume/side (mL) | 69 | 1868.0 ± 885.5 | 150 ± 5850 |
3.2. Disease‐specific QoL (FLQA‐lk)
All 20 patients completed both FLQA‐lk questionnaires before liposuction and 6 months after treatment, answering each question. Before treatment with liposuction, disease‐specific QoL in patients with lipoedema was low (score > 4.0) on every single subscale as well as on the global score (Table 2; Figure 1). The lipoedema patients had the least QoL in their social lives (4.3 ± 0.4), followed by daily lives (4.2 ± 2.8) and physical complaints (4.2 ± 0.4). The generic QoL was also rather low in lipoedema patients, with the highest degree of dissatisfaction occurring in the area of health status concerning lymphatic disease (3.5 ± 1.4). The mean QoL score was 3.7 ± 1.4, with the patients rating their general health status slightly higher (4.4 ± 1.7) (Figure 2A‐C).
TABLE 2.
Disease‐specific quality of life (QoL) before and after liposuction treatment in lipoedema patients
| Liposuction (mean ± SD) | ||||
|---|---|---|---|---|
| N | Before | After | P | |
| Subscales | ||||
| Physical complaints | 20 | 4.2 ± 0.4 | 2.9 ± 1.0 | <.001 a |
| Daily life | 20 | 4.2 ± 2.8 | 2.8 ± 1.1 | <.001 a |
| Social life | 20 | 4.3 ± 0.4 | 2.8 ± 1.1 | <.001 a |
| Emotional well‐being | 20 | 4.1 ± 0.5 | 3.0 ± 1.0 | <.001 a |
| Therapy of lymphatic disorder | 13 | 4.1 ± 0.5 | 3.1 ± 1.2 | .003 a |
| Global score | 20 | 4.2 ± 0.4 | 2.9 ± 1.0 | <.001 a |
| Generic QoL | ||||
| General health status | 20 | 4.4 ± 1.7 | 6.9 ± 1.7 | <.001 b |
| Lymphatic disease health status | 20 | 3.5 ± 1.4 | 6.2 ± 1.8 | <.001 a |
| QoL | 20 | 3.7 ± 1.4 | 6.6 ± 1.5 | <.001 b |
t‐test.
Wilcoxon signed‐rank test.
FIGURE 1.
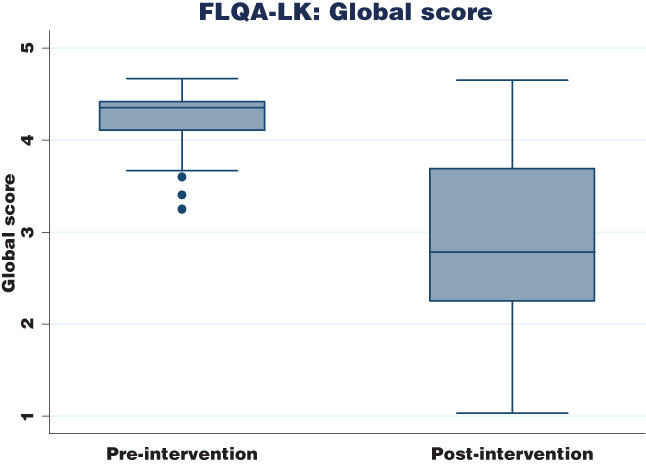
Changes in FLQA‐lk global scores in lipoedema patients before and after liposuction. FLQA‐lk, Freiburg Life Quality Assessment in its disease‐specific variant for lymphatic diseases
FIGURE 2.
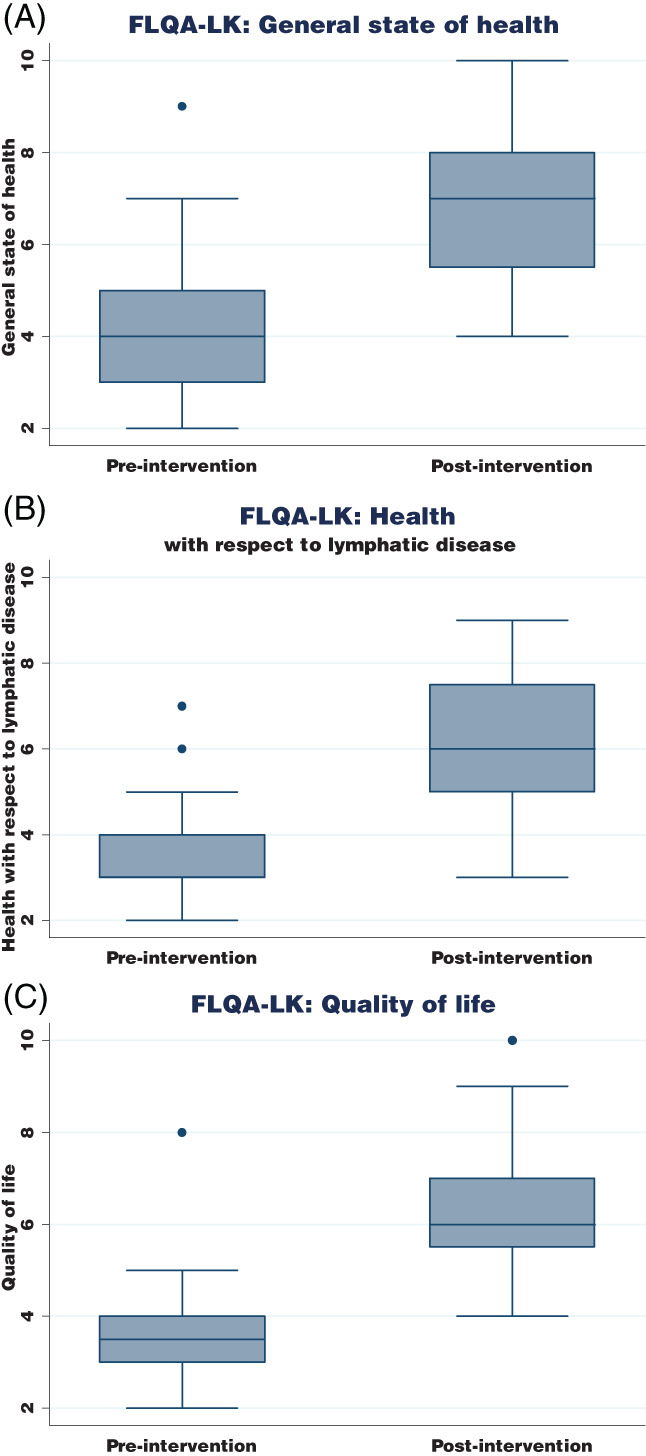
A, Effect of liposuction treatment on general state of health. B, Health status concerning lymphatic disease as measured by the FLQA‐lk questionnaire. C, Health status concerning quality of life as measured by the FLQA‐lk questionnaire. FLQA‐lk, Freiburg Life Quality Assessment in its disease‐specific variant for lymphatic diseases
Following liposuction treatment, lipoedema patients showed a significant improvement regarding disease‐specific QoL on all subscales and for the global score (2.9 ± 1.0) (Figure 1). The best QoL was found in the areas of social and daily life (both 2.8 ± 1.1), followed by physical complaints with a mean score of 2.9 ± 1.0. Regarding the generic QoL, the most considerable difference was found in the area of QoL, which improved to 6.6 ± 1.5. Health status concerning lymphatic disease had the second‐highest difference in mean scores compared to before liposuction, and also the lowest of the three general QoL scores (6.2 ± 1.8). Finally, the general health status had the highest mean score after liposuction treatment (6.9 ± 1.7) (Figure 2A‐C).
3.3. Correlations
Correlation analyses failed to show any significant correlations between BMI and general health status, health status concerning lymphatic disease, or QoL (P > .05) (Table 3). There was a significant negative correlation to be found when examining the number of liposuction sessions performed and general health status (P = .007). This suggests that a higher number of liposuction treatment sessions has a positive effect on general health status in lipoedema patients. A trend towards significance was noted for the number of liposuction sessions performed and health status concerning lymphatic disease (P = .078), whereas the number of liposuction treatments did not seem to affect QoL (P = .197). There was no significant association between total liposuction volume per side and general health status, with health status concerning lymphatic disease or QoL (Figures 3 and 4).
TABLE 3.
Correlation analyses for generic quality of life (QoL) and clinical data
| Variable | Mean difference before and after liposuction | n | r* | P |
|---|---|---|---|---|
| BMI | General health status | 19 | 0.080 | .745 |
| Lymphatic disease health status | 19 | 0.064 | .795 | |
| QoL | 19 | 0.023 | .924 | |
| Number of liposuction sessions | General health status | 20 | −0.582 | .007 |
| Lymphatic disease health status | 20 | −0.403 | .078 | |
| QoL | 20 | −0.301 | .197 | |
| Total liposuction volume/side (mL) | General health status | 20 | −0.262 | .264 |
| Lymphatic disease health status | 20 | 0.035 | .882 | |
| QoL | 20 | −0.301 | .198 |
Note: r* = Spearman's.
FIGURE 3.
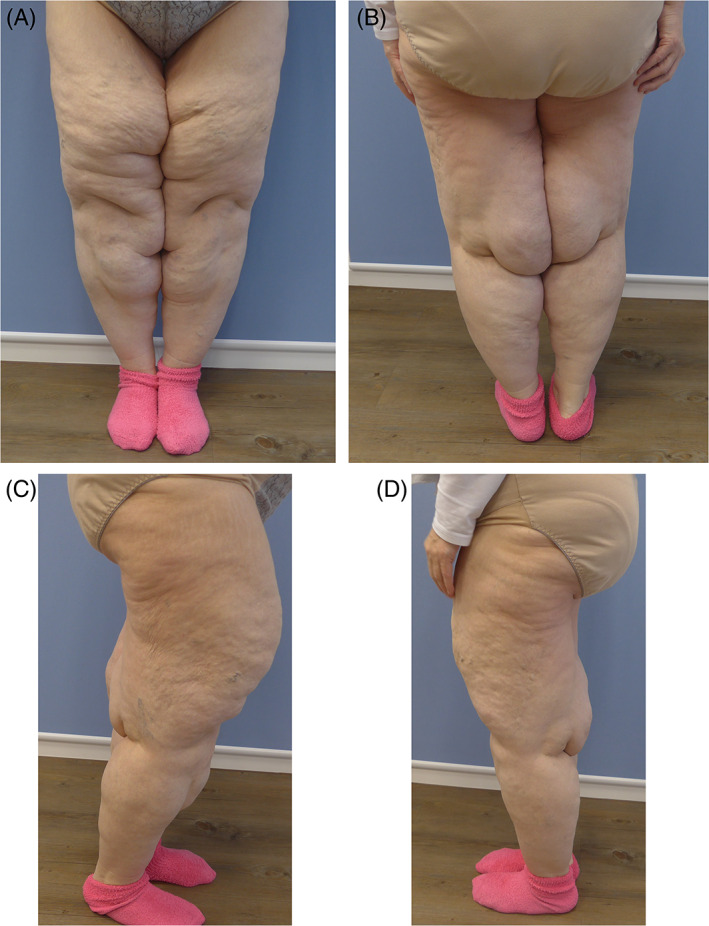
A‐D, Preoperative view of a 43‐year‐old female patient with lipoedema stages II and III
FIGURE 4.

A‐D, Postoperative view of the same patient 20 months after performing three liposuctions and a L‐shaped inner thigh lift; overall volume of liposuction: 12 500 mL
4. DISCUSSION
Recently, there has been a growing body of literature focusing on the effects that lipoedema has on the patients' lives. A narrative review summarising the findings of four included observational cross‐sectional studies 11 , 25 , 26 , 27 found that health‐related QoL measured with generic instruments was markedly reduced in lipoedema patients. 10 Lipoedema patients displayed more inadequate psychological adjustment, deficits in physical and social functioning, as well as increased anxiety and depression. This corresponds to our findings, in which emotional well‐being and QoL in the social and daily life subscales were extremely low. In the review, pain, poor skin condition, and impaired limb mobility also negatively impacted health‐related QoL. 10
In both short‐ and long‐term studies, tumescent liposuction has proven to be a viable treatment option in patients for lipoedema treatment, especially when conservative treatment options are not able to provide adequate symptom relief. We found that liposuction significantly improved health‐related and disease‐specific QoL using the validated FLQA‐lk questionnaire. These findings are in line with our clinical experiences, in which lipoedema patients are highly satisfied with treatment outcomes.
To date, very few studies examining the effect of liposuction on QoL in lipoedema patients have been published. A study on 25 patients with lipoedema of the lower extremities reported significant reductions in spontaneous pain, pressure sensitivity, the sensation of tension, bruising, aesthetic impairments, and general impairment of QoL. 16 However, this study did not incorporate a validated questionnaire with multiple subscales, instead of using only a visual analogue scale ranging from zero to 10 to measure general impairment of QoL. Second, the sample size of comparable patients was even smaller than in this study, as only 13 patients had stage III lipoedema, while 11 patients were diagnosed with stage II lipoedema, and one patient had stage I lipoedema.
In another study, 189 women answered a non‐validated, 183‐item questionnaire after undergoing liposuction for surgical treatment of lipoedema. 28 The study also included patients of all three lipoedema stages, with 51% of the women having a diagnosis of lipoedema stage II. QoL improved significantly in all three stages, with 86% improvement in stage III patients. Even though complication rates were low, the perceived benefit from liposuction was highest in patients with stage I or II lipoedema, suggesting that patients may benefit from liposuction in earlier disease stages.
This study has several limitations. First, we were only able to include a very small number of lipoedema patients in this study, thus limiting the statistical analyses and generalisability of results. The fact that only 69 patients who underwent liposuction treatment for lipoedema at our hospital in a timeframe of 15 years were identified seems unusual at first glance. However, it must be taken into consideration that lipoedema is commonly misdiagnosed, even to the present day and especially in early disease stages due to lack of awareness on the condition. 2 , 6 , 7 , 8 It seems quite possible that a large number of patients would have been (mis‐)diagnosed with lymphoedema or other conditions, which would have had a direct impact on the choice of the treatment strategy. Also, although the German Society of Phlebology's recommendation for tumescent liposuction as an integrated part of treatment in lipoedema patients dates back to 2005, the high cost of treatment resulting from multiple liposuctions sessions without coverage from health insurance would have made this course of therapy inaccessible for many patients.
Second, the prospective part of the study had only 6 months of follow‐up regarding health‐related QoL, so it was not possible to make any conclusions regarding the long‐term effects of liposuction treatment.
Third, our choice of the FLQA‐lk instrument for measuring health‐related QoL in lipoedema patients might have also affected the study outcomes in some way. In this research, patients had a primary diagnosis of lipoedema and secondary lymphoedema. Both the initial questionnaire and the short form used in this study were initially designed and validated in patients with lymphatic diseases. 23 , 24 Lipoedema patients would benefit from a disease‐specific questionnaire, which has yet to be designed and validated.
Finally, although health‐related QoL based on pre‐post intervention score differences is traditionally used in research, several authors have suggested that this method is susceptible to bias due to changes in patients' response behaviour. 27 , 29 Application of instruments based on the patient benefit index methodology in future studies may provide a more direct disease‐specific insight and measurement of patient‐relevant treatment benefit.
5. CONCLUSIONS
The study results show that tumescent liposuction treatment for lipoedema under local and general anaesthesia significantly improves health‐related QoL and disease‐specific QoL. As most women undergoing liposuction required multiple treatment sessions, and a higher number of treatment sessions seemed to have a positive effect on general health status, this should be taken into consideration in treatment planning. More research is needed to find out the exact reasons for the correlation between the effect of treatment sessions and general health status, rather than other logical parameters such as BMI or mean volume of tissue removed per side.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Schlosshauer T, Heiss C, von Hollen A‐K, Spennato S, Rieger UM. Liposuction treatment improves disease‐specific quality of life in lipoedema patients. Int Wound J. 2021;18:923–931. 10.1111/iwj.13608
Contributor Information
Torsten Schlosshauer, Email: torsten.schlosshauer@web.de.
Ulrich M. Rieger, Email: ulrich.rieger@fdk.info.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Reich‐Schupke S, Schmeller W, Brauer WJ, et al. S1 guidelines: lipedema. J Dtsch Dermatol Ges. 2017;15(7):758‐767. [DOI] [PubMed] [Google Scholar]
- 2. Fife CE, Maus EA, Carter MJ. Lipedema: a frequently misdiagnosed and misunderstood fatty deposition syndrome. Adv Skin Wound Care. 2010;23(2):81‐92. [DOI] [PubMed] [Google Scholar]
- 3. Földi E, Földi M. Lipedema. In: Földi M, Földi E, Strössenreuther RHK, Kubik S, eds. Földi's Textbook of Lymphology for Physicians and Lymphedema Therapists. 2nd ed. Munich: Elsevier Urban & Fischer; 2006:417‐427. [Google Scholar]
- 4. Paolacci S, Precone V, Acquaviva F, et al. Genetics of lipedema: new perspectives on genetic research and molecular diagnoses. Eur Rev Med Pharmacol Sci. 2019;23(13):5581‐5594. [DOI] [PubMed] [Google Scholar]
- 5. DIMDI . ICD‐10‐GM Version 2020: Kapitel IV Endokrine, Ernährungs‐ und Stoffwechselkrankheiten (E00‐E90). https://wwwdimdide/static/de/klassifikationen/icd/icd‐10‐gm/kode‐suche/htmlgm2020/block‐e70‐e90htm. Accessed April 14, 2020.
- 6. Warren Peled A, Kappos EA. Lipedema: diagnostic and management challenges. Int J Womens Health. 2016;8:389‐395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wiedner M, Aghajanzadeh D, Richter DF. Differential diagnoses and treatment of lipedema. Plastic Aesthet Res. 2020;7:10. [Google Scholar]
- 8. Buck DW, Herbst KL. Lipedema: a relatively common disease with extremely common misconceptions. Plast Reconstr Surg Glob Open. 2016;4(9):e1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Herbst KL. Rare adipose disorders (RADs) masquerading as obesity. Acta Pharmacol Sin. 2012;33(2):155‐172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alwardat N, Di Renzo L, Alwardat M, et al. The effect of lipedema on health‐related quality of life and psychological status: a narrative review of the literature. Eat Weight Disord. 2020;25(4):851‐856. 10.1007/s40519-019-00703-x. [DOI] [PubMed] [Google Scholar]
- 11. Dudek JE, Białaszek W, Ostaszewski P, Smidt T. Depression and appearance‐related distress in functioning with lipedema. Psychol Health Med. 2018;23(7):846‐853. [DOI] [PubMed] [Google Scholar]
- 12. Stutz JJ, Krahl D. Water jet‐assisted liposuction for patients with lipoedema: histologic and immunohistologic analysis of the aspirates of 30 lipoedema patients. Aesthetic Plast Surg. 2009;33(2):153‐162. [DOI] [PubMed] [Google Scholar]
- 13. Wollina U. Lipedema—an update. Dermatol Ther. 2019;32(2):e12805. [DOI] [PubMed] [Google Scholar]
- 14. Schmeller W, Meier‐Vollrath I. Tumescent liposuction: a new and successful therapy for lipedema. J Cutan Med Surg. 2006;10(1):7‐10. [DOI] [PubMed] [Google Scholar]
- 15. Rapprich S, Dingler A, Podda M. Liposuction is an effective treatment for lipedema—results of a study with 25 patients. J Dtsch Dermatol Ges. 2011;9(1):33‐40. [DOI] [PubMed] [Google Scholar]
- 16. Dadras M, Mallinger PJ, Corterier CC, Theodosiadi S, Ghods M. Liposuction in the treatment of Lipedema: a longitudinal study. Arch Plast Surg. 2017;44(4):324‐331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schmeller W, Hueppe M, Meier‐Vollrath I. Tumescent liposuction in lipoedema yields good long‐term results. Br J Dermatol. 2012;166(1):161‐168. [DOI] [PubMed] [Google Scholar]
- 18. Halk AB, Damstra RJ. First Dutch guidelines on lipedema using the international classification of functioning, disability and health. Phlebology. 2017;32(3):152‐159. [DOI] [PubMed] [Google Scholar]
- 19. Peprah K, MacDougall D. Liposuction for the Treatment of Lipedema: A Review of Clinical Effectiveness and Guidelines. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health; 2019. [PubMed] [Google Scholar]
- 20. Papadopulos NA, Kolassa MJ, Henrich G, et al. Quality of life following aesthetic liposuction: a prospective outcome study. J Plast Reconstr Aesthet Surg. 2019;72(8):1363‐1372. [DOI] [PubMed] [Google Scholar]
- 21. Beschluss des Gemeinsamen Bundesausschusses über eine Richtlinie über Maßnahmen zur Qualitätssicherung nach § 136 Absatz 1 Satz 1 Nummer 2 des Fünften Buches Sozialgesetzbuch (SGB V) bei Verfahren der Liposuktion bei Lipödem im Stadium III (QS‐RL Liposuktion): Erstfassung: BAnz AT 06.12.2019 B4 ; 2019. https://www.g-ba.de/downloads/39-261-3963/2019-09-19_QS-Massnahmen_Liposuktion-Lipoedem-III_BAnz.pdf. Accessed April 14, 2020.
- 22. Baumgartner A, Hueppe M, Schmeller W. Long‐term benefit of liposuction in patients with lipoedema: a follow‐up study after an average of 4 and 8 years. Br J Dermatol. 2016;174(5):1061‐1067. [DOI] [PubMed] [Google Scholar]
- 23. Augustin M, Bross F, Földi E, Vanscheidt W, Zschocke I. Development, validation and clinical use of the FLQA‐I, a disease‐specific quality of life questionnaire for patients with lymphedema. Vasa. 2005;34(1):31‐35. [DOI] [PubMed] [Google Scholar]
- 24. Augustin M, Conde Montero E, Hagenström K, Herberger K, Blome C. Validation of a short‐form of the Freiburg Life Quality Assessment for lymphoedema (FLQA‐LS) instrument. Br J Dermatol. 2018;179(6):1329‐1333. [DOI] [PubMed] [Google Scholar]
- 25. Dudek JE, Białaszek W, Ostaszewski P. Quality of life in women with lipoedema: a contextual behavioral approach. Qual Life Res. 2016;25(2):401‐408. [DOI] [PubMed] [Google Scholar]
- 26. Romeijn JRM, de Rooij MJM, Janssen L, Martens H. Exploration of patient characteristics and quality of life in patients with lipoedema using a survey. Dermatol Ther (Heidelb). 2018;8(2):303‐311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Blome C, Augustin M, Heyer K, et al. Evaluation of patient‐relevant outcomes of lymphedema and lipedema treatment: development and validation of a new benefit tool. Eur J Vasc Endovasc Surg. 2014;47(1):100‐107. [DOI] [PubMed] [Google Scholar]
- 28. Cobos L, Herbst K, Ussery C. Liposuction for Lipedema (Persistent Fat) in the US Improves Quality of Life. J Endocr Soc. 2019;3(Supplement_1): MON‐116. [Google Scholar]
- 29. Augustin M, Radtke MA, Zschocke I, et al. The patient benefit index: a novel approach in patient‐defined outcomes measurement for skin diseases. Arch Dermatol Res. 2009;301(8):561‐571. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


