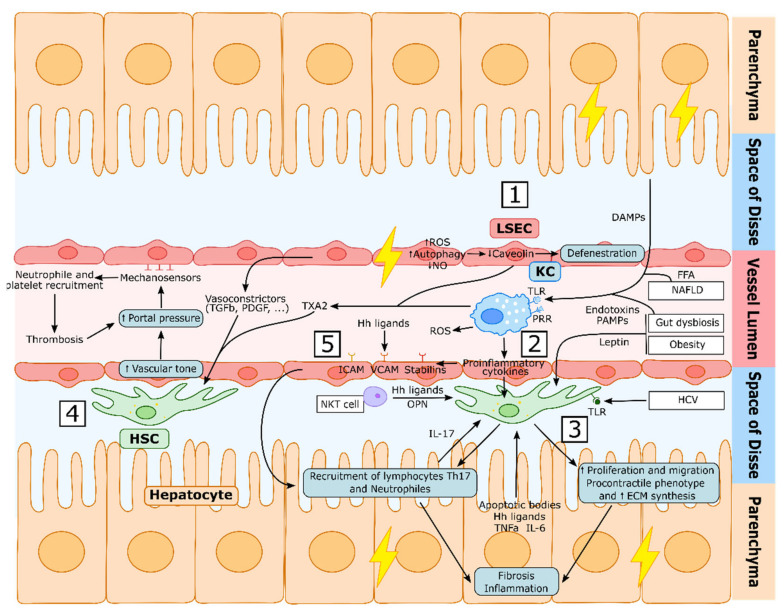
Figure 3.
Liver Sinusoid dysfunction during chronic liver disease. (1) During chronic liver injury, LSEC become dysfunctional, impairing the autophagy process, increasing the generation of reactive oxygen species (ROS), decreasing nitric oxide (NO) intrahepatic levels and synthetizing increased vasoconstrictors, which induces the activation of HSCs. Hepatic damage further induces LSECs defenestration through the degradation of caveolin-1. (2) Kupffer cells (KCs) are activated by damage-associated molecular patterns (DAMPs), pathogen-associated molecular patterns (PAMPs), free-fatty acids (FFA) and endotoxins via their toll-like receptors (TLR) and pattern recognition receptors (PRR). This induces the secretion of reactive oxygen species (ROS) and proinflammatory cytokines that, together with other proinflammatory molecules secreted by other cell types, activate HSCs (3) which will acquire a proliferative, migrating, procontractile and proinflammatory phenotype that will induce liver fibrosis and inflammation. This procontractile phenotype increases vascular tone (4), which further increases portal pressure, activating LSECs mechanosensors that induce the recruitment of neutrophiles and platelets, the accumulation of which produces thrombi that will further increase portal pressure. LSECs are also activated by hepatocyte-derived hedgehog (Hh) ligands and other proinflammatory mediators (5) secreted during the inflammatory and injury process, which—via adhesion molecules such as ICAM, VCAM and Stabilins—will recruit leukocytes to the liver tissue, further promoting fibrosis and inflammation.