Abstract
Purpose
This study aimed to review and extract all publications containing concepts related to definitions of frailty and categorize them.
Methods
A total of six electronic databases (PubMed, Ovid web, Web of Science, Scopus, Embase, Cochrane Library, and ProQuest) were searched to identify studies that introduced a definition of frailty up to October 2018. No language restrictions were imposed.
Results
Totally, 104,370 papers were found in the initial search and finally 68 papers were included. Of these, 21 studies provided a conceptual definition and 50 original articles also 9 review articles provided a practical definition. Moreover, 12 papers had both definitions of frailty. Of them, 62 were published in English, 2 in Portuguese, 1 in Japanese, 2 in Korean, and 1 in German languages.
Conclusion
Many screening tools have been developed but neither of them can cover a wide range of parameters at the same time, nor do they have simplicity in the execution. It is important to note that although a more or less general consensus on one single definition might be expected, we believe that the elderly population is too heterogeneous to allow a tool to address it as a whole, and such a definition may even be impossible. Therefore, in the absence of a “Gold Standard” definition, it is suggested to seek accurate knowledge of the strengths and weaknesses of each definition and choose the most appropriate definition and the most effective evaluation tool according to the purpose of the research and the characteristics of the older population.
Keywords: Frailty, Aged, Systematic review
Introduction
The concept of frailty appeared in geriatric medical literature in the 1950s and 1960s for the first time, followed by a substantial body of contributions in the 1980s and 1990s [1]. In the US, the Federal Council on Aging (FCA) presented the term “frailty elderly” in 1978 to describe a specific group of elder individuals. The FCA defined frailty in older adults as subjects who usually, and not always, have an age > 75 and who need several health services for activities of daily living because of multi-morbidity [2]. Although after that time, more than 40 operational definitions of frailty were reported by researchers [1, 3], the introduction of the frailty phenotype by Fried and colleagues in 2001 is usually considered as the birth of frailty [4]. Afterwards, several studies by geriatricians and gerontologists were performed during the next decades. The number of scientific publications on frailty has exponentially increased during the past 15 years [1].
Although the term “frailty” is the core of geriatrics and gerontology, there is no clear consensus regarding the definition of this condition [4–7]. Perhaps this uncertainty is rooted in the intrinsic characteristics of frailty. Indeed, frailty is not an inevitable consequence of the aging process, neither is it a disease with a defined onset, and this is the reason why it has confusing heterogeneous manifestations [8]. Whereas multidimensionality and multi-morbidity are considered as the most important manifestations of frailty, its definitions should be validated in a wide variety of cultural contexts and addressed in economic, ethnic, and clinical settings in order to demonstrate the predictive validity of its adverse outcomes [9].
Subsequently, it is difficult to distinguish the frail elder people. Therefore, it is necessary to introduce a reliable and valid definition and also provide standard for the measurement of frailty concept in order to identify such high-risk members of the population and consequently to prevent the onset of this phenomenon and reduce or prevent progress to frailty through interventions [2].
On the other hand, depending on the definitions, settings, and ethnicity, a varied prevalence of frailty in older adults has been reported in studies; but the frequently-cited figure for frailty in community-dwelling adults aged 65 and older is on average 10.7% (range 4.0–59.1%) [4, 10]. Global frailty prevalence rates are variable too; low- to mid-income countries have higher rates of frailty compared to high-income countries. However, there is little information available about frailty rates in different ethnic groups [11–13]. Finally, health care professionals will face frail persons more and more frequently in the future due to an increasingly aging population [4]. From a research perspective, the level of frailty is as a good predictor or selection criterion for treatment or intervention. So awareness of frailty criteria is important for the early diagnosis and prevention or delay of the onset of the late-life disability and adverse outcomes [14].
What cited above expresses the importance and necessity of he present research which is conducted to study the concept and various definitions of frailty to assist geriatricians and gerontologists, particularly for those newcomers in this field to understand the features and differences of each definition and obtain a clearer and more comprehensive concept of frailty.
Objective
We aimed to conduct a systematic approach to present all published scientific documents containing concepts and definitions of frailty in older adults, and then categorizing these concepts to construct a more comprehensive concept for frailty.
Method
Protocol
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed to conduct the research target.
Search strategy and information sources
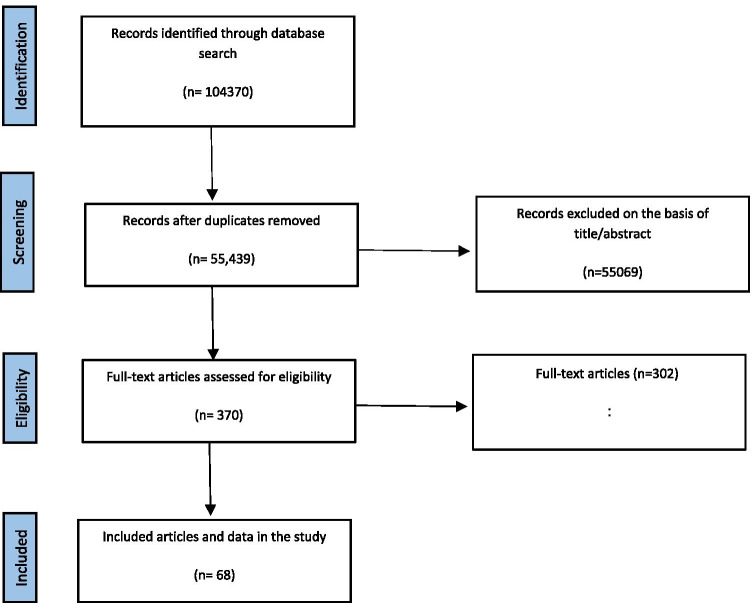
We performed a systematic search of the literature using six international databases: PubMed, Ovid web, Web of Science, Scopus, Embase, Cochrane Library, and ProQuest for documents published up to October 2018. The main searched keywords were “frailty” and “elderly”, their synonyms, related words, and Medical Subject Headings (MeSH) terms in PubMed. Reference lists of included papers, especially systematic review articles, were also manually searched in order to identify additional relevant articles. Furthermore, we considered conference proceedings. No language restrictions were imposed. The search strategy is presented in Table 1. The search flowchart using Preferred Reporting Items for Systematic Reviews and Meta-Analyses, PRISMA [15] method is demonstrated in Fig. 1.
Table 1.
Search strategies for different databases
|
PubMed “aged” [MeSH Terms] OR aged[Text Word])) OR Elder*) OR older adult*) OR old people)) AND “frailty” [MeSH Terms] OR frailty[Text Word])) OR asthenia) OR frail*) OR vulnerability) OR prefrail) OR pre frail) OR incapacity) OR fragil*) OR comorbidity) OR co-morbidity) OR co morbidity) AND ((defin*) OR guidline*) OR statement) OR determination) OR interpretation)) |
|
Scopus ((TITLE-ABS-KEY (aged) OR TITLE-ABS-KEY (elder*) OR TITLE-ABS-KEY (older AND adult*) OR TITLE-ABS-KEY (old AND people))) AND ((TITLE-ABS-KEY (defin*) OR TITLE-ABS-KEY (guidline*) OR TITLE-ABS-KEY (statement) OR TITLE-ABS-KEY (determination) OR TITLE-ABS-KEY (interpretation))) AND ((TITLE-ABS-KEY (frailty) OR TITLE-ABS-KEY (asthenia) OR TITLE-ABS-KEY (frail*) OR TITLE-ABS-KEY (vulnerability) OR TITLE-ABS-KEY (prefrail) OR TITLE-ABS-KEY (pre AND frail) OR TITLE-ABS-KEY (incapacity) OR TITLE-ABS-KEY (fragil*) OR TITLE-ABS-KEY (comorbidity) OR TITLE-ABS-KEY (co-morbidity) OR TITLE-ABS-KEY (co AND morbidity))) AND (LIMIT-TO (PUBYEAR, 2006)) |
|
Web of Science (frailty OR asthenia OR frail* OR vulnerability OR prefrail OR pre frail OR incapacity OR fragil* OR comorbidity OR co-morbidity OR co morbidity) AND (aged OR elder* OR older adult* OR old people) AND (defin* OR guidline* OR statement OR determination OR interpretation) |
|
Embase 'aged':ab,ti OR 'elder*':ab,ti OR 'older adult*':ab,ti OR 'old people':ab,ti AND 'frailty':ab,ti OR 'asthenia':ab,ti OR 'frail*':ab,ti OR 'vulnerability':ab,ti OR 'prefrail':ab,ti OR 'pre frail':ab,ti OR 'incapacity':ab,ti OR 'fragil*':ab,ti OR 'comorbidity':ab,ti OR 'co morbidity':ab,ti OR 'co-morbidity':ab,ti AND 'defin*':ab,ti OR 'guidline*':ab,ti OR 'statement':ab,ti OR 'determination':ab,ti OR 'interpretation':ab,ti |
|
Ovid (aged or elder* or older adult* or old people).mp. [mp = ti, ot, ab, tx, kw, ct] (frailty or asthenia or frail* or vulnerability or prefrail or pre frail or incapacity or fragil* or comorbidity or co-morbidity or co morbidity).mp. [mp = ti, ot, ab, tx, kw, ct] (defin* or guidline* or statement or determination or interpretation).mp. [mp = ti, ot, ab, tx, kw, ct] |
|
ProQuest ((aged OR elder* OR (older adult*) OR (old people)) AND (defin* OR guidline* OR statement OR determination OR interpretation)) AND ((incapacity OR fragil*) OR (comorbidity OR co-morbidity OR (co morbidity)) OR (frailty OR asthenia OR frail* OR vulnerability OR prefrail)) |
Fig. 1.
Study flowchart demonstrates the inclusion–exclusion process
Eligibility criteria
The eligibility criteria were as follows:
All articles which have presented a definition of frailty,
Review, observational and qualitative studies,
Addressing all the primary causes of frailty (secondary cases were not considered).
Letters to the editor, editorial, animal studies, and conference proceeding, were excluded. Moreover, all clinical trial studies used a definition of frailty that developed by other researchers and for this reason, they excluded from our study.
Study selection and data extraction
After removing duplicate studies, two researchers independently assessed the eligible studies according to the inclusion and exclusion standards via screening titles and abstracts. The full text of the study was subsequently reviewed to see if a study meets the selection criteria; if there was any doubt regarding eligibility disagreement was resolved by a discussion between the researchers. In case that they could not reach a consensus, a third independent researcher was consulted.
A reference list of all the papers which met the quality criteria was reviewed to identify and select the relevant papers. In case of incomplete data or if the full-text was not available, the corresponding authors were contacted for additional information or full-text requests.
Finally, two researchers independently extracted the following data: author, publication year, the study region, title, the name of the journal, research type, frailty definition, type of frailty, the basis of frailty definition. All extracted data were stored in the Microsoft Excel file format.
Quality appraisal
The methodological quality of the eligible studies was assessed independently by two researchers using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) for cohort studies, Q–A Tool for review studies, Critical Appraisal Skills Program (CASP) for qualitative studies, Standards for Reporting Diagnostic accuracy studies (STARD), and STROBE checklist for cross-sectional studies. The probable discrepancy between them was resolved by consulting the third independent researcher.
Results
Study selection
Totally, 104,370 papers were found in the initial search among which 48,931 papers were excluded due to duplication. From 55,439 remained papers, 55,069 were deleted after reviewing the titles and abstracts, then 370 studies were reviewed as full-text, and finally, 68 published papers were included in our study. The process of study selection is summarized in Fig. 1.
Study characteristics
Of the 68 studies included in the review, 62 papers were published in English [2, 4, 5, 16–73], 2 in Portuguese [74, 75], 1 in Japanese [76], 2 in Korean [77], and 1 in German [78] languages. One of the operational definitions of frailty was first reported in Japanese and in this case, a systematic study that evaluated the validity of the instrument in this article was used instead [79]. Of total 68 papers, 21 provided a conceptual definition [2, 4, 5, 16–28, 30, 31, 69, 73] (Table 2), 50 original articles [5, 16, 23, 24, 27–32, 34–80] (Table 3), 9 review articles [22, 28, 29, 33, 69, 72, 73, 79, 80] (Table 4) provided a practical definition, and 12 research articles had both definitions of frailty.
Table 2.
Conceptual definitions
| First author | Publication year | Research type | Frailty definition | Quality assessment |
|---|---|---|---|---|
| Winograd C.H | 1988 | Cross-sectional | A state of being neither “too independent” nor “too impaired” that puts the person at risk for adverse health outcomes | 14/32 |
| Speechley and Tinetti | 1991 | Cross-sectional |
Classification into three groups: “frail” (possessed ≥ 4 frailty factors), “vigorous” (< 2 frailty factors), or “transition” (not meeting the criteria for frail or vigorous): Age > 80 – Depression – Use of sedatives – Near vision loss – Balance and gait abnormalities – Infrequent walking – Decreased strength in shoulder – Decreased strength in knee – Lower extremity disability (((To divide our elderly subjects into frail and vigorous groups based on clustering of demographic, physical, and psychological characteristics))) |
12/32 |
| Buchner D.M. and Wagner | 1992 | Review | Conceptual definition: frailty as a state of reduced physiologic reserve associated with increased susceptibility to disability | 9/10 |
| Walter M. Bortz | 1993 | Review | Conceptual definition: diminished energy flow (interaction) between the individual and their environment conceptual model: the physics of frailty (physical sciences) frailty is reversible through the reestablishment of optimal energy flow | 8/10 |
| Ory M.G | 1993 | Systematic review |
The components of physical frailty are: – Severely impaired strength mobility – Balance – Endurance |
9/10 |
| Rockwood K | 1994 | Review | A vulnerability state resulting from a precarious balance between the assets maintaining health and the deficits threatening it | 8/10 |
| Kaufman S.R | 1994 | Qualitative | The social construction of frailty (medical anthropology) frailty is a quality and a dynamic adaptational process on the part of elderly persons, families, and healthcare personnel | 21/30 |
| Brown I | 1995 | Review | Frailty is diminished ability to carry out important practical and social activities of daily living | 9/10 |
| Hamerman D | 1999 | Review | Complex and cumulative expression of altered homeostatic responses to multiple stresses resulting in metabolic imbalance | 9/10 |
| Bortz W.M | 2002 | Review | A state of muscular weakness and other secondary widely distributed losses in function and structure | 8/10 |
| Hanneke Schuurmans | 2004 | Cross-sectional | Frailty is a loss of resources in several domains of functioning, which leads to a declining reserve capacity for dealing with stressors | 17/32 |
| Gobbens R.J.J | 2009 | Diagnostic accuracy study |
Integral conceptual definition of frailty: frailty is a dynamic state affecting an individual who experiences losses in one or more domains of human functioning (physical, psychological, social), which is caused by the influence of a range of variables and which increases the risk of adverse outcomes. The actual state of a frail elderly person is a dynamic one. This state can be positioned on a continuum between non frail and frail |
27/34 |
| Robbert J. Gobbens | 2010 | Review | Frailty is a dynamic state affecting an individual who experiences losses in one or more domains of human functioning (physical, psychological, social) that are caused by the influence of a range of variables and which increases the risk of adverse outcomes | 9/10 |
| Susanne Gustafsson | 2012 | Qualitative |
• Being bodily weak and ill • Being negatively influenced by personal qualities • Lacking balance in everyday activities • Being dependent in everyday life • Not being considered important • Being hindered by physical milieu and defective community service • Having an inadequate social network |
25/30 |
| Maarten Boers | 2015 | Review | Linking the Frailty Concept to a New Definition of Health: health is the resilience or capacity to cope, and to maintain and restore one’s integrity, equilibrium, and sense of wellbeing in three domains: physical, mental, and social | 7/10 |
| Raphael D | 1995 | Diagnostic accuracy study | Frailty is a diminished ability to carry out important practical and social activities in daily living | 26/34 |
| Campbell and Buchner | 1997 | Review | A syndrome of multisystem reduction in reserve capacity as a result of which an older person’s function may be severely compromised by minor environmental stresses, giving rise to the condition of “unstable disability” | 9/10 |
| Strawbridge | 1998 | Cohort | A syndrome involving grouping of problems and losses of capacities in multiple domains, which make the individual vulnerable to environmental challenge | 23/34 |
| Dayhoff N.E | 1998 | Diagnostic accuracy study | Frailty is diminished functioning combined with diminished self-rated health | 27/34 |
| Linda Fried | 2001 | Diagnostic accuracy study | A biologic syndrome of decreased reserve and resistance to stressors, resulting from cumulative declines across multiple physiologic systems, causing vulnerability to adverse outcomes | 29/34 |
| Nourhashemi F | 2001 | Cross sectional | A combination of biological, physiological, social, and environmental changes that occur with advancing age and increase vulnerability to changes in the surroundings and to stress | 17/32 |
Table 3.
Operational definitions (original articles)
| First author | Publication year | Study region | Research type | Frailty definition | Type of frailty | Basis of frailty definition | Frailty assessment | Instrument | Frailty scale cut-off | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|
| Winograd C.H | 1991 | Hospital | Prospective cohort study | A state of being neither “too independent” nor “too impaired” that puts the person at risk for adverse health outcomes |
Suffering from terminal illness or severe dementia: – Impaired function – Common geriatric conditions i.e., falls, depression, confusion, incontinence, polypharmacy, etc. – Chronic and disabling illness – Social problems |
Winograd Screening Instrument | Classification into three groups: “independent” in all ADL (activities of daily living), “frail” meeting ≥ 1 of the following criteria and “severely impaired”, suffering from terminal illness or severe dementia | 21/34 | ||
| Jack M. Guralnik | 1994 | Community | Cross-sectional study | Encompasses slowness, weakness, and balance | Three domains focused on lower-extremity muscle performance: gait speed, time to rise from a chair without using arms five times, and ability to stand in tandem balance for 10 s | The short physical performance battery (SPPB) scale | Each is scored 1 to 4 and a total score ≤ 5 of 12 is required for a diagnosis of frailty | 17/32 | ||
| Strawbridge | 1998 | Community | Cohort |
Deficiencies in > 2 of the following domains: – Physical health (sudden loss of balance, weakness in arms, weakness in legs, and orthostatic dizziness) – Nutritional (loss of appetite and unexplained weight loss) – Cognitive (attention deficit, trouble finding words, and memory difficulties) – Sensory (visual and hearing problems) |
A syndrome involving grouping of problems and losses of capacities in multiple domains, which make the individual vulnerable to environmental challenge | Proposed an early frailty model based on deficiencies in four domains of functioning (physical, nutritive, cognitive, and sensory) | Strawbridge questionnaire | Deficiencies in ≥ 2 of the domains | 22/34 | |
| Dayhoff N.E | 1998 | Community | Cross-sectional | Scoring ≥ 21 on the World Health Organization Assessment of Functional Capacity combined with a self-report of perceived health | Frailty is diminished functioning combined with diminished selfrated health | ≥ 21 | 26/32 | |||
| Paw CMJMCA | 1999 | Community-dwelling | Cohort | Inactivity combined with weight loss | 30/34 | |||||
| Brown M | 2000 | Community | Cross-sectional study |
Physical performance test: – Strength – Range of motion – Balance – Gait – Coordination and speed of reaction – Sensation |
“Index of frailty” | Classifying elderly in three levels (not frail, mildly frail, moderately frail) | 21/32 | |||
| Linda Fried | 2001 | Community | Cohort | A biologic syndrome of decreased reserve and resistance to stressors, resulting from cumulative declines across multiple physiologic systems, causing vulnerability to adverse outcomes | As a clinical syndrome in which three or more of the following criteria were present: unintentional weight loss (10 lbs in past year), self-reported exhaustion, weakness (grip strength), slow walking speed, and low physical activity | Fried phenotype (FP) | 0–5, 3 levels (not frail, pre frail, frail), (≥ 3 frail) | 33/34 | ||
| Nourhashemi F | 2001 | Community | Cross sectional | Deficits in at least one IADL (instrumental activities of daily living) was used as a marker of frailty | A combination of biological, physiological, social, and environmental changes that occur with advancing age and increase vulnerability to changes in the surroundings and to stress | IADL | ≥ 1 | 17/32 | ||
| Debra Saliba | 2001 | Community | Cohort | Self-reported screening tools based on the deficit model | 13 Questions that examine age, health status, physical activities, ADL, and IADL (13-item function-based scoring system that considers age, self-rated health, limitation in physical function, and functional disabilities) | Vulnerable elderly survey-13 (VES-13) | ≥ 3 | 29/34 | ||
| Mitnitski A.B | 2002 | Community-dwelling and institution | Cohort | Made a list of 20 deficits (signs, impairments, symptoms or disabilities) observed after a structured clinical examination based upon comprehensive geriatric assessment (CGA) | Frailty index | Continuous scale: 0–1 | 30/34 | |||
| Mitnitski | 2001 | Community | Cohort | Frailty index include symptoms (e.g., changes in sleep, memory complaints, low mood), signs (e.g., tremor, decreased peripheral pulses), abnormal laboratory values (e.g., urea, creatinine, calcium), disease classifications (e.g., diabetes mellitus, Parkinson’s disease), and disabilities (e.g., dependence in bathing or dressing) | A frailty index was defined as the proportion of accumulated deficits (symptoms, signs, functional impairments, and laboratory abnormalities) | Frailty index (92 items) (FI-CSHA) | Continuous scale = 0–1 | 28/34 | ||
| Schuurmans H | 2004 | Community, Hospital, Nursing home | Cross-sectional |
– Mobility – Physical fitness – Vision – Hearing – Nourishment – Morbidity – Cognition (perception) – Psychosocial (depression, anxiety, loneliness) |
The term frailty should not only refer to physical vulnerabilities, but also in psychosocial imbalances | A loss of resources in several functional domains that leads to reduced reserve capacity to deal with stress | Consists of 15 questions regarding the IADL, ADL, physical functions, cognition, mood, vision, hearing, and polypharmacy. (four domains: physical, cognitive, social, and psychological) | Groningen frailty indicator (GFI) | (Frail, not frail), range: 0–15, ≥ 4 frail | 25/32 |
| Studenski S | 2004 | Community | Diagnostic accuracy study |
(CGIC-PF). The CGIC-PF includes 6 intrinsic domains (38 items): – Mobility – Balance – Strength – Endurance – Nutrition – Neuromotor performance |
Clinical global impression of change in physical frailty instrument (CGIC-PF) | Dichotomous scale: (frail–not frail) | 31/34 | |||
| Jones D.M | 2004 | Community-dwelling | Diagnostic accuracy study |
The index results from the count of impairments in: – Cognitive status – Mood – Communication – Mobility – Balance – Bowel function – Bladder function – Nutrition – Activities of daily living (ADL) – Social status, plus the comorbidity count of active diagnoses |
Developed a frailty index (FI) based on a standard comprehensive geriatric assessment (CGA) | Frailty index (FI/CGA) | 0–20, Three levels of frailty were mild (FI-CGA 0–7), moderate (FI-CGA 7–13), and severe (FI-CGA > 13) | 30/34 | ||
| Kenneth Rockwood | 2005 | Community, Hospital | Cohort | Measured frailty with the CSHA clinical frailty scale, a 7-point scale based upon a frailty index of 70 items | Based on a comprehensive geriatric assessment (CGA), with scores ranging from “very fit” to “severely frail” | In this scale, a significant degree of emphasis is placed on the inability to perform ordinary activities in the home, or for personal care as well as the symptom burden. Although scoring is based purely on clinician judgment, the predictive abilities are similar to those seen with other frailty assessments | Is based on patients’ health information, which can be completed over a short time and without any special equipment | Clinical frailty scale | Ordinal scale: 1–77 levels (from robust to complete dependence) | 26/34 |
| Overcash J.A | 2005 | A retrospective chart review of patients at the H. Lee Moffitt Cancer Center | Diagnostic accuracy study | The CGA will be defined as a multidimensional assessment consisting of functional, emotional and cognitive components | aCGA (15 items) | 25/34 | ||||
| Puts M.T.E | 2005 | Community | Cohort |
Nine frailty markers: – Body weight – Peak expiratory flow – Cognition – Vision – Hearing – Incontinence – Sense of mastery – Depressive symptoms – Physical activity |
≥ 3 frail | 32/34 | ||||
| Darryl B. Rolfson | 2006 | Edmonton, Alberta, Canada | Diagnostic accuracy study | 10 Domains: cognition, balance and mobility, mood, functional independence, medication use, social support, nutrition, health attitudes, continence, burden of medical illness and quality of life (all standard historical items in geriatric assessment) | Edmonton frail scale (EFS) | Ordinal scale: 1–17 5 levels (not frail, apparently vulnerable, mild, moderate and sever frailty) | 30/34 | |||
| Kristine E. Ensrud | 2008 | Community | Cohort | Three components: lower limb strength, unintentional body weight loss, and exhaustion | Cohort | (1) Weight loss (irrespective of intent to lose weight) of 5% or more between the third and fourth examinations (mean [SD] years between examinations, 2.0 [0.3]); (2) the subject’s inability to rise from a chair five times without using her arms; and (3) reduced energy level, as identified by an answer of “no” to the question “Do you feel full of energy?” on the geriatric depression scale/categorizes the physical status as robust, prefrail, and frail | SOF frailty criteria |
Three levels (not frail, pre frail, frail) ≥ 2 frail |
24/34 | |
| Gobbens R.J.J | 2009 | Based on the literature search and consultation of 17 experts during the expert meetings | Qualitative | Nutrition, mobility, physical activity, strength, endurance, balance, cognition, sensory functions, mood, coping, social relations and social support | (Frail, not frail) | 8/10 | ||||
| Thomas N. Robinson | 2009 | Community | Cohort | Eight ‘markers’ of frailty (age, cognition, recent weight loss, BMI < 25, serum albumin, falls, depression, hematocrit) | Cognition was assessed using the mini-cog test (combined three items recall with a clock draw test with proven validity for assessing cognitive function). Mini-cog scores range from 5 (normal cognition) to 0 (impaired cognition)//chronic under-nutrition by the presence of weight loss of 10 lbs in past 6 months//number of falls in the 6 months before | 30/34 | ||||
| Roman Romero-Ortuno | 2010 | Community | Diagnostic accuracy study | Exhaustion/weight loss/weakness/slowness/low activity | The frailty definition used in this study is related (but not equivalent) to the one by Fried | SHARE frailty instrument | Three levels (not frail, pre frail, frail) | 28/34 | ||
| Robbert J.J. Gobbens | 2010 | Community | Diagnostic accuracy study | The TFI is based on an integral conceptual model of frailty, based on “a working framework in development” | Self-report ED screening tools based on the deficit model | Physical domain [unexplained weight loss, difficulty in walking, strength in hands, and physical tiredness, physical health, balance, vision problems, and hearing problems (range 0–8)]/psychological [cognition, depressive symptoms, anxiety, and coping (range 0–4)]/social [living alone, social relations, and social support (range 0–3)]//the maximum score is 15 and represents the highest level of frailty | Tilburg frailty indicator (TFI) | (Frail, not frail) range: 0–15, ≥ 5 frail | 28/34 | |
| Lee D.H | 2010 | Health Sciences Centre (cardiac surgery patient) | Cohort | Frailty was defined as any impairment in activities of daily living (Katz index), ambulation, or a documented history of dementia | Consider even one impairment in any of these measures as evidence of frailty | 24/34 | ||||
| Josep Garre-Olmo | 2013 | Community | Cohort | Social frailty | (1) Living alone, (2) lack of a person to help with ADL, (3) infrequent contact with family (less than once a week), (4) infrequent contact with friends or neighbors (less than once a week), (5) absence of a confidant, (6) lack of support for daily living during the past 3 months | ≥ 3 | 28/34 | |||
| Francisco José García-García | 2014 | Community | Cohort | The FTS includes 7 dimensions (12 items): energy balance and nutrition, activity, nervous system, vascular system, weakness, endurance, and slowness. These domains become operational through 12 items | The first is the “frailty trait,” which is similar to the biological trait that is reached over time. The second is the “frailty load,” which is the change in the level of frailty trait due to a specific factor (e.g., disease, hospitalization) | The frailty trait scale (FTS) | 0–5; 3 Levels (not frail, pre frail, frail) | 27/34 | ||
| Matteo Cesari | 2014 | Community | Cross-sectional | Self-reported screening tools based on the phenotype model | This questionnaire consists of two steps. The first step is designed to discriminate between disabled and nondisabled seniors by asking whether they could walk 400 m and could climb a flight of stairs. The second step attempts to identify older adults with frailty by asking them three questions regarding body weight loss, exhaustion, and physical activity | The ‘Frail Nondisabled’ (FiND) questionnaire | (Frail- not frail) | 23/32 | ||
| Tze Pin Ng (T.P. Ng) | 2014 | Community | Cohort | 13 Factors: age ≥ 75, no formal education, heart failure, Asthma/COPD, stroke, depression, hearing impairment, visual impairment, nutritional risk score ≥ 3, low hemoglobin, WBC (× 10(9)/L) ≥ 6.5, FEV1/FVC < 0.7, eGFR < 60 (mL/min/1.73 m2) | Cumulative deficit model or the multidimensional model | Frailty risk index (FRI) | 1 or 2 pre frail, ≥ 3 frail | 29/34 | ||
| Judah Goldstein | 2015 | Community, Geriatric Clinic | Diagnostic accuracy study | A questionnaire based on a CGA that can be completed by care partners (CP-FI-CGA) | 62 Items | (CP-FI-CGA): care partners frailty index comprehensive geriatric assessment | Dichotomous scale: (frail–not frail) | 29/34 | ||
| Makizako | 2015 | Community | Prospective cohort study |
Self-reported questionnaire including five domains (1) going out less frequently (2) Rarely visiting friends (3) Feeling unhelpful to friends or family (4) Living alone (5) Not talking to someone every day |
24/34 | |||||
| Minoru Yamada | 2015 | Community | A prospective cohort study | Self-reported screening tools based on the phenotype model |
Five items: nutrition/shrinking, physical function, physical activity, forgetfulness, and emotions/exhaustion Answer: 0 or 1 |
Frailty screening index | Range: 0–5/ 3 levels (0 robust, 1 to 2 pre frail, ≥ 3 frail) | 28/34 | ||
| Eklund Kajsa | 2016 | Emergency Department | Diagnostic accuracy study |
Frailty was measured by Fried’s classical frailty indicators, with the addition of visual and cognitive impairment Because of their high impact on disability |
The FRESH-screening includes five short questions | Indicators included: weakness, fatigue, weight loss, low physical activity, poor balance, low gait speed, visual impairment, and cognitive impairment | FRESH-screening | ≥ 3 frail | 28/34 | |
| Dewi Vernerey | 2016 | Community | Cohort | Dimension global health status, dimension PSYCHOLOGICAL—depression, dimension Cognitive, Dimension ENVIRONMENTAL, Dimension SOCIO-CULTURAL, Dimension SEXUAL, Dimension BURDEN OF HELP, Dimension NUTRITIONAL, Dimension MOBILITY, Section for EXAMINER (1Q) | 19 Items describing 9 dimensions | Frailty GIR evaluation (FRAGIRE) | Continuous scale: 0–100. There is no cut-off point. Higher scores equate to greater frailty | 29/34 | ||
| John N. Morris | 2016 | Home care agencies | Diagnostic accuracy study | The concept of frailty, a relative state of weakness reflecting multiple functional and health domains, continues to receive attention within the geriatrics field | Multidimensional approaches to measuring frailty have included cognition, mood and social components | 29 Items, across 6 categories of function, movement, cognition and communication, social life, nutrition, and clinical symptoms | InterRAI home care frailty scale | (0–29), ≥ 19 Frail | 25/34 | |
| Emiel O. Hoogendijk | 2017 | Community | Diagnostic accuracy study | Frailty index (FI) as a measure of deficit accumulation, that is, a measure of the cumulative burden of, for example, symptoms, diseases, conditions, and disability | 32 Health deficits from the physical, mental and cognitive domain were used to construct the LASA–FI | Longitudinal aging study Amsterdam frailty index (LASA-FI) | (Frail, not frail), ≥ 0.25 frail | 29/34 | ||
| Nigel Teo BSocSci | 2017 | Community | Cohort | Based on multiple facets of general or social resources, and social behaviors and activities |
Seven-item social frailty index: (1) Living alone (2) No education (3) Absence of a confidant (4) Infrequent contact (5) Infrequent social activities (6) Financial difficulty (7) Socioeconomic deprivation |
Social frailty index | 0: nil SF, 1: low, 2–7: high | 26/34 | ||
| Melissa K. Andrew | 2010 | Community | Cohort |
Social vulnerability index (1) Communication to engage in wider community (2) Living situation (3) Social support (4) Socially oriented activities of daily living (5) Leisure activities (6) Ryff scale (7) How do you feel about your life (8) Socioeconomic status |
40 Items, self-report variables relating to potential social deficits | Social vulnerability index (SVI)-D | 0–40, Index scores were split into tertiles of high, intermediate, and low social vulnerability | 27/34 | ||
| Speechley and Tinetti | 1991 | Community | Cross sectional |
– Age > 80 – Depression – Use of sedatives – Near vision loss – Balance and gait abnormalities – Infrequent walking – Decreased strength in shoulder – Decreased strength in knee – Lower extremity disability |
Classification into three groups: “frail” (possessed ≥ 4 frailty factors), vigorous (< 2 frailty factors), or “transition” (not meeting the criteria for frail or vigorous) | 12/32 | ||||
| Ma L | 2016 | Community | Cohort | 68 Parameters were drawn from six variables: demographic characteristics, physical health, physical function, living behavior, social function, mental health, and cognitive function | 69 Item frailty index | 0–1, ≥ 0.25 Frail | 24/34 | |||
| Freiheit | 2010 | Hospital | Cohort | Brief frailty index including physical, cognitive, and psychosocial criteria in older patients with CAD undergoing coronary angiography | Five items, three domains | Brief frailty index | Frail, not frail, ≥ 3 frail | 28/34 | ||
| Michel Raıche | 2008 | Community | Cross-sectional | Seven question, age, male, health problem with limited activity, to need someone to help you, health problems that require you to stay at home, can you count on someone close to you, regularly use a cane, a walker of a wheelchair to move about | PARISMA-7 | Range: 0–7, (frail, not frail) ≥ 3 frail | 28/32 | |||
| Ravaglia | 2008 | Community | Cohort | Nine easy-to-collect predictors may identify aged people at increased risk of adverse health outcomes associated with frailty | Using data from a population-based cohort, a frailty score was developed including nine independent predictors of mortality: age ≥ 80 years, male gender, low physical activity, comorbidity, sensory deficits, calf circumference < 31 cm, IADL dependence, gait and performance test score ≤ 24, and pessimism about one’s health | Prognostic frailty score | 0–9, Without cut-off | 29/34 | ||
| Joseph | 2014 | Hospital | Cohort | The 15 variable trauma specific frailty index is an independent predictor of unfavorable discharge disposition in geriatric trauma patients | 5 Domains (15 variables): comorbidities, daily activities, health attitude, function, nutrition | Trauma specific frailty index (TSFI) |
(Frail, not frail) > 0.27 Frail |
31/34 | ||
| Scarcella | 2005 | Community | Cohort | Mental–physical area, socio-economical and functional area | 3 Domains and 32 items | Geriatric functional evaluation (GFE) | Three levels (severely impaired, moderately impaired, totally independent) | 28/34 | ||
| Hebert R | 1996 | Community | Diagnostic accuracy study | The items focus on the physical (four items), social (one item) and cognitive (one item) domains of functioning | Sherbrooke postal questionnaire (SPQ) | Range: 0–6, ≥ 2 frail | 29/34 | |||
| Moraes E.N | 2016 | Community | Diagnostic accuracy study | The IVCF-20 is a questionnaire that covers multidimensional aspects of the older adult’s health condition and has 20 questions divided into eight sections | IVCF-20 can be considered a CGA methodology performed by professionals who are non-specialists in geriatrics and gerontology, and can be applied by middle-level professionals previously trained | Age (one Q), health self-perception (one Q), functional disabilities ( four Q), cognition (three Q), mood (two Q), mobility (six Q), communication (Q), and multiple comorbidities (one Q) | Indice de Vulnerabilidade Clinico-Functional (IVCF-20) Portuguese | 0–40, 3 Levels (robust, potentially frail, frail) | 28/24 | |
| Nunes D.P | 2015 | Community | Cross-sectional | Frailty phenotype | Five items in one domain (physical): weight loss, decreased strength, decreased walking speed, low physical activity, self-reported fatigue | Modelo Fried adaptadi Portuguese | 0–5, 3 Levels (not frail, pre-frail, frail), ≥ 3 frail | 26/32 | ||
| Shinkai S | 2010 | Community | Diagnostic accuracy study | Self-reported assessment of frailty syndrome in older adults | 15 Items, 2 domains (physical, psychological) | Kaigo-Yobo Check-list Japanese | (Frail, not frail), range: 0–15, > 4 frail | 25/34 | ||
| Hwang H.S | 2010 | Long-term care institutions for older adults | Diagnostic accuracy study |
Eight items in two domains (physical, psychological) The Korean frailty index 8-item questionnaire was established by a panel of experts from the Korean Geriatrics Society |
Korean frailty index Korean | Three levels (robust, pre frail, frail) | 26/34 | |||
| Dapp N | 2012 | Community | Cohort | In contrast to the literature, the focus is equally on risks and resources. The questions relate more to facts (intensity of doing things) than to subjective assessments. The questionnaire was developed in the LUCAS project | 12 Items in physical domain | LUCAS German | 0–6, 3 Levels (healthy, pre frail, frail) | 33/34 |
Table 4.
Operational definitions (review articles)
| First author | Publication year | Study region | Research type | Frailty definition | Type of frailty | Basis of frailty definition | Frailty assessment | Instrument | Frailty scale cut-off | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|
| Lachs M.S | 1990 | Community | Review | A simple approach that can be used by clinicians to screen the functional status of older patients in community practice. The focus is on carefully selected tests of vision, hearing, upper and lower limb function, urinary incontinence, mental status, instrumental and basic activities of daily living, environmental hazards, and social support systems | The FSS combines seven core domains of functioning: disability, mobility, cognitive function, visual function, hearing function, urinary continence and social support. For each domain the score was equal to 0 when the function was preserved and it was equal to 1 when the function was lost | The frailty staging system (FSS) | .The study developed a score that considered a grading of impairment stratifying subjects into three classes of frailty (0 or 1 = class 1, 2 or 3 = class 2 and 4 through 7 = class 3) | 6/10 | ||
| Raphael D | 1995 | Community | Review | Developed an instrument to measure frailty, based on the definition of the diminished ability to carry out the important practical (21 items) and social activities (9 items) of daily living | Frailty is a diminished ability to carry out important practical and social activities in daily living | 8/10 | ||||
| Campbell and Buchner | 1997 | Community | Review | Frailty can be diagnosed clinically by measuring four key capacities required for successful interaction with the environment: musculoskeletal function, aerobic capacity, cognitive and integrative neurological function and nutritional state | A syndrome of multisystem reduction in reserve capacity as a result of which an older person’s function may be severely compromised by minor environmental stresses, giving rise to the condition of “unstable disability” |
Deficits in the four key components of frailty: – Musculoskeletal function (grip strength and chair stand) – Aerobic capacity (sub-maximal treadmill and 6 min walk) – Cognitive/integrative neurological (Mini-Mental State Examination and Static balance test) – Nutritional (body mass index and arm muscle area) |
Campbell and Buchner | 7/10 | ||
| Abellan van Kan | 2008 | Community | Systematic review | A combination of aging, disease, and other factors that make some people vulnerable | Cumulative deficit model or the multidimensional model (self-reported screening tools based on the phenotype model) |
Suggested to develop a FRAIL scale, a case finding tool, that should comprise the following five domains: – Fatigue – Resistance (the ability to climb stairs) – Ambulation (ability to walk certain number of meters) – Number of illnesses – Loss of weight (> 5%) |
FRAIL scale | 0–5, 3 Levels (0 = robust, 1–2 = pre-frail, ≥ 3 = frail) | 9/10 | |
| Buchner D.M | 1992 | Community | Review |
Deficits in three major components of frailty: – Neurological control – Mechanical performance – Energy metabolism |
9/10 | |||||
| Rockwood K | 1994 | Community | Review |
Deficits in five major components of frailty: – Functional dependence – Restricted mobility – Poor self-rated health – Limited social resources – Increased use of healthcare services |
8/10 | |||||
| Bergman H | 2004 | Community | Review |
The core components of frailty are: – Weight loss/under nutrition – Weakness – Endurance – Physical activity – Slowness – Cognitive decline – Depressive symptoms |
Extended the frailty phenotype definition using a life course approach, which incorporates biological, social, clinical, psychological, and environmental determinants | 6/10 | ||||
| Ory M.G | 1993 | Community | Review |
The components of physical frailty are: – Severely impaired strength – Mobility – Balance – Endurance |
8/10 | |||||
| Sewo Sampaio | 2016 | Community | Systematic review | Self-reported screening tools based on the deficit model | 25 Simple yes/no questions that are designed to examine the IADL, physical domain, nutritional domain, eating domain, socialization domain, memory domain, and mood domain | Kihon checklist (KCL) Korean | Range: 0–25, frail, not frail (a higher score indicates worse functioning) | 8/10 |
In order to better understand these definitions, we have categorized them according to evaluation criteria into four sub-categories (physical, cognitive and psychological dimensions, nutritional, and social), which are summarized in Table 5.
Table 5.
Frailty definitions domains
| Frailty instrument | Physical | Nutrition | Psychological/cognitive | Social | ||
|---|---|---|---|---|---|---|
| The frailty staging system (FSS) | + | + | + | |||
| Winograd screening instrument | + | + | + | |||
| SPPB | + | |||||
| Raphael | + | + | ||||
| Campbell and Buchner | + | + | + | |||
| Strawbridge questionnaire | + | + | + | |||
| Dayhoff | + | |||||
| Paw CMJMCA | + | |||||
| Index of frailty | + | |||||
| Frailty phenotype | + | |||||
| IADL | + | |||||
| VES-13 | + | |||||
| Frailty index (92 items) | + | + | + | |||
| GFI | + | + | + | |||
| CGIC-PF | + | + | ||||
| CGA-FI | + | + | + | + | ||
| aCGA | + | + | ||||
| Clinical frailty scale (CFS) | + | + | ||||
| Puts MTE | + | + | ||||
| Edmonton frail scale (EFS) | + | + | + | + | ||
| SOF | + | |||||
| Gobbens | + | + | + | + | ||
| Thomas N. Robinson | + | + | + | |||
| SHARE | + | |||||
| Tilburg frailty indicator (TFI) | + | + | + | |||
| Lee DH | + | + | ||||
| FRAIL | + | |||||
| Social frailty | + | |||||
| Frailty trait scale (FTS) | + | + | ||||
| Frail nondisabled (FiND) | + | |||||
| Frailty risk index (FRI) | + | + | + | |||
| CP-FI-CGA | + | + | + | + | ||
| Frailty screening index | + | + | ||||
| InterRAI home care frailty scale | + | + | + | + | ||
| Kihon checklist | + | + | + | + | ||
| Short screening instrument (FRESH-screening) | + | + | ||||
| Social frailty | + | |||||
| Social frailty index | + | |||||
| Social vulnerability index | + | |||||
| FRAGIRE | + | + | + | + | ||
| Buchner | + | |||||
| Rockwood | + | + | ||||
| Bergman | + | + | + | + | ||
| Speechley and Tinett | + | + | ||||
| Ory MG | + | |||||
| Sherbrooke Postal questionnaire (SPQ) | + | + | + | |||
| IVCF-20 | + | + | ||||
| Kaigo-Yobo check-list | + | + | ||||
| Korean frailty index | + | + | ||||
| Brief frailty index | + | + | ||||
| PRISMA | + | |||||
| Prognostic frailty score | + | + | ||||
| Trauma specific frailty index (TSFI) | + | |||||
| Geriatric functional evaluation (GFE) | + | + | + | |||
| Modelo Fried adaptadi | + | |||||
| LUCAS | + |
Discussion
This study was carried out to conduct a systematic review of studies reporting a conceptual and operational definitions of “Frailty”. Although the development of the frailty theory was documented in the literature and the frailty concept was almost universally accepted [81], the researchers have not come up with a universally agreed upon unique definition, conceptual model, or operational definition of frailty [2].
Conceptual definitions
Numerous conceptual definitions of frailty have been proposed and numerous researcher have addressed the issue of frailty from a different aspect. In 1994, an article defined frailty and briefly described it as an “evolving concept” and this concept persists to some extent until today [69]. Conceptual definitions are provided in Table 2. Winograd C.H. et al. (1988) defined frailty as ‘a condition that is neither “very independent” nor “very impaired” and that puts a person at the risk of several health consequences [17]. It should be noted that most conceptual definitions focus mainly on the physical problems that affect the older people [2]. Only very few definitions have focused on other aspects of the subjects’ functioning areas such as psychological ones [2]. There was only one definition that addressed other areas of vulnerability (i.e. a combination of biological, physiological, social, and environmental changes) [27].
Three conceptual definitions clearly refer to negative outcomes. In Campbell and Buchner's definition, the negative consequence is “unstable disability.” Winograd and Fried also described the relationship between frailty and adverse outcomes but did not provide an explanation of what these adverse outcomes are in their conceptual definitions [2].
Functional definition
The operational definition, also known as the empirical definition, is in fact a concept that is expressed as the number of observable criteria [82]. As acknowledged at the beginning of the article, there are several definitions of frailty, which makes it difficult to reach a consistent and accepted definition, and researchers also have difficulty comparing statistical results. Practical definitions are given in Table 3.
Definitions focusing on the physical dimensions of frailty
To date, various approaches have been proposed regarding frailty. One of these approaches is to address frailty by focusing on the physical dimension. One of the most widely used definitions in this field was first proposed in 2001 by Fried et al., who introduced frailty as a syndrome called “frailty phenotype” [83]. This syndrome is defined by five indicators in which the elderly subjects who have had three or more criteria are defined as frail subjects. These criteria include: (1) unintentional weight loss of more than or equal to 4.5 kg in the last year or weight loss equal or more than 5% of body weight during the mentioned period, (2) weakness, reduced handgrip strength, (3) reduced endurance and energy, (4) reduced walking speed, and (5) reduced level of physical activity (5).
In fact, the phenotype of frailty is still valid although only one of dimensions of frailty has been addressed, it is commonly used in research and clinical practice [84]. Because Fried considered only the physical dimension as a criterion, some literatures also refer to this definition as “physical frailty.” In recent years, a number of assessment tools have been developed based on this approach that evaluate only the physical dimension [32, 39–41, 54, 57, 85].
The most commonly used tools for frailty screening are physical function, walking speed, and muscle strength. Despite the validity of the “frailty phenotype”, some believe that it has problems in implementation. Kristine E. Ensrud, for example, stated in a paper that the “frailty phenotype” is inapplicable in clinical settings and that the three components, handgrip strength, walking speed, and physical activity, require sufficient knowledge on the distribution of measurement in a given population [41].
Other tools have been introduced that measure physical dimension of frailty, including the osteoporosis fracture (SOF) index, which is much easier to measure clinically and uses only three components to evaluate [41], short physical performance battery (SPPB), or other short performance tests such as timed-up-and-go and handgrip strength test [32, 86]. Moreover “Frail tool” uses five questions to assess frailty and unlike the two previous scales, frail frailty phenotype and SOF, which require face-to-face assessment, FRAIL can be easily used by telephone and can be self-administered. This tool is very economic and can be frequently used in various populations [41, 80, 87].
The Survey of Health, Aging and Retirement in Europe (SHARE-FI) tool defines frailty close to the definition of the frailty phenotype, but it is not exactly the same. This definition eradicates one of the limitations of the “frailty phenotype”, which is its only applicability to the population aged 65 and over, whereas frailty is more related to biological than chronological age. The SHARE-FI tool is applicable to people ≥ 50 years. However, this tool is not suitable for measuring frailty in elderly care centers and hospitals settings as it does not target this population [54].
As we mentioned, there are several factors affecting the development of frailty, and poor nutrition status is one of these factors. An inappropriate diet is associated with an increased risk of chronic diseases, decreased antioxidant functions, impaired immune responses, increased risk of bone fractures, sarcopenia, and frailty. A systematic review study confirmed that the importance of quantitative (such as energy intake) and qualitative (such as nutrient quality) nutritional factors in the development of frailty syndrome [88]. The “Edmonton Frail Scale” (EFS), “Frailty Index”, and “Strawbridge Questionnaire” address the nutritional factors in detecting of frailty [31, 37, 53].
In general, it seems that frailty should be considered as a continuous gradient of impaired functioning of several biological systems, which we consider as a “frailty trait” attribute, and is affected by other factors such as environment, lifestyle, genetics, and comorbidity. Since it addresses only one dimension, Fried's definition is unable to accurately represent this continuous change [42]. On the other hand, this definition has been criticized for limiting the criteria and not paying attention to important domains such as cognitive deficits [84].
Despite the limitations of Fried’s definition, it can be applicable in primary health care services for the elderly without the need for a preliminary clinical evaluation. Therefore, it is possible to use it at population levels to classify the population into three groups (robust and healthy, pre-frail and frail) [81]. We believe that tools developed based on Fried’s model address only one dimension of the health of the older adults, and each in fact have some strengths and weaknesses.
There is a fear that if the definitions of frailty focus exclusively on physical criteria, attention to the subjects as a whole will be jeopardized. These conditions can also potentially lead to disruption of care and consequently reduce the quality of care provided for frail individuals [89].
Definitions considering frailty as a syndrome
There is a strong evidence that other criteria should be considered as part of the frailty syndrome, as these criteria may be influenced by the same biological processes that lead to the manifestation of physical frailty. Cognitive impairment, mood disorders, sensory impairment, social status and support, chronic illnesses, and disability have been considered by many researchers as part of frailty syndrome, and by considering these criteria the ability to predict physical vulnerability and as a result, poor clinical outcomes increase [86]. An alternative model that was proposed by Rockwood et al. in 2005 was “Frailty Index” [46]. The frailty index (FI) was first introduced with 92 items. This index was developed based on the comprehensive geriatric assessment (CGA) to assess the frailty and cover the physical, cognitive, psychological, nutritional, and social domains [37, 46]. The CGA is widely used and accepted as an important approach to assess the care that the senior people need. The CGA is a multidimensional team approach to assess medical, functional, psychosocial, and environmental needs of older adults [57]. The FI was developed followed by the criticisms of the physical frailty models. The “Frailty Index” includes health disorders in the physical, mental, and cognitive domains that are influenced by social and environmental factors, and does not address just physical ones. This index fully considers the concept of multidimensional frailty [56, 90].
Some researchers believe that cognitive evaluation is necessary to diagnose frailty because cognitive decline increases the predictive value of other adverse health indicators. Nowadays, there is a consensus that frailty is a multi-dimensional concept [90]. Ensuing the introduction of “the frailty index”, other practical definitions were developed that addressed not only the physical but also other dimensions, such as the Edmonton frail scale and the Groningen frailty indicator [30, 53]. In the above definitions, including Raphael D’s and Nourhashemi F’s definitions, and also according to the clinical global impression of change in physical frailty (CGIC-PF frailty) index, ‘disability’ is also considered in their assessment of frailty, whereas Gobbens believes that the existence of disability will dismiss all these assessment tools as useless [44]; as a definition is successful only if it fulfils all necessary criteria, hence removing ‘comorbidity’ and ‘disability’ from the definition [2]. Gobbens states that frailty assessment requires a tool that does not include disability but one which covers several areas of human functioning (physical, mental, and social) [44]. Considering the World Health Organization's definition of health [44], this researcher has defined frailty as a dynamic state; that is, a frail person is a person who was injured in one or more areas of performance (physical, mental, social) and was affected by a wide range of risk factors, which in turn increase the risk of adverse consequences [44]. In 2010, the Tilburg frailty indicator (TFI) was developed by the same researcher, which assesses frailty with 15 questions in three areas, including physical, psychological, and social domains [44]. There are other tools and definitions which have addressed all or parts of the frailty domains, but none provides a standard definition of frailty.
Definitions focusing on the social dimension
Social factors play an important role in moderating frailty’s adverse outcomes, and social factors appear to affect health outcomes at many levels, including biological, health behaviors (including diet, exercise, and smoking), availability of social support, and access to qualified health care [91]. Despite the development of the concept of frailty and the emergence of various definitions, the least researches and studies has been carried out in the field of social frailty. However, some researchers have focused specifically on the social field and have examined the importance of this field and its role in health and have proposed definitions focusing on the social dimension. Some studies offer a narrow definition of social frailty as “having a lack of social participation and social support”. However, other researchers have used various aspects of social frailty to define this concept [71]. A multifaceted concept that was proposed by Bunt et al. is the continuous risk for the loss of public and social resources, problem in self-management behaviors, activities, and capabilities that are necessary to meet basic social needs [92]. Moreover, the results of a limited number of studies in this area show a shortage of social resources to meet the basic social needs as well as a lack of social activities, behaviors and problem in self-management capabilities that should be considered as the components of social frailty [92]. Makizako defined “social frailty” by just five criteria: (1) leaving home less than the previous year, (2) meeting friends less than before, (3) self-feeling of unusefulness for friends and family, (4) living alone, and (5) not having daily conversations with others—and this definition has a significant relationship with the occurrence of disability [58]. In a study in 2017, Nigel Teo BSocSci also introduced the “Social Frailty Index” with seven items that included “living alone, lack of education, not having a trusted and reliable person, limited contact, limited social activities, financial problems and socio-economic deprivation”. Other studies have shown that the social frailty index without and with physical frailty could predict the burden of care in the older population [71].
A study in 2008 evaluated the views of twelve health professionals on two broad definitions of frailty. Six main ideas emerged from the conversations: (1) definitions of frailty are complementary, (2) there is no potential for prevention, (3) defining frailty is a very complex task, (4) What is the concept of frailty? (5) The multidimensional definition is complete, and (6) frailty is a condition that can last a lifetime. Most experts believe that the definitions are complementary because frailty arises as a result of the interaction of biological, psychological, and social factors throughout life (the perception of health professionals of two definitions of frailty in elderly people) [93].
It is clear that any definition of frailty should meet the criterion of “practicality”. Practicality means that it should be modifiable by interventions or could be preventable. In addition, the definition of frailty should be able to serve as a developing tool for measuring and assessing frailty. Finally, a successful definition also should be “clinically reasonable.” This refers to the acceptance of the frailty definition by those who use it in clinics [29, 94, 95].
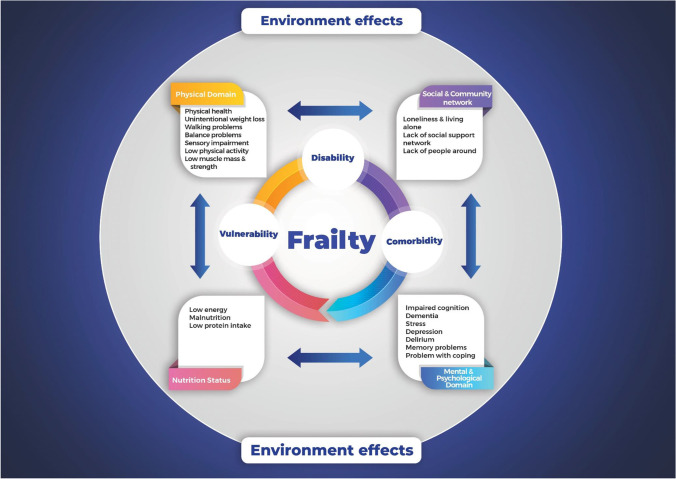
It seems that frailty includes not only the physical health, but also comprised other components such as social, psychological and biological aspects. Emerging problems in several dimensions of health maybe lead to comorbidity, disability, and vulnerability. In fact, the most vulnerable group in geriatric refers to older people, who have comorbidity or are disabled. The concept of disability, comorbidity and frailty, while differing with each other have a unique clinical management. There are strong associations between these three concepts and each one is a predictor of another ones. These concepts significantly correlated and often predict each other. Since frailty is considered as the core of aging syndrome, comorbidity and disability undoubtedly lead to frailty through “health deficits”. On the other hand, environmental factors have roles in developing these health conditions. Disability and comorbidity strongly are affected by environmental factors [93, 96, 97] (Fig. 2).
Fig. 2.
Framework conceptual of frailty
Strengths and limitations of the study
A comprehensive evaluation of and presenting conceptual and practical definitions together without considering the limitations of language is one of the strengths of this research, which leads to a broad understanding of frailty. One of the weaknesses of this study was that most of the studies were observational studies. Regarding the limitations of the research, it was not possible to estimate the pooled sensitivity and specificity of tools due to the lack of a gold standard definition. Moreover, we could not address the relationships and interactions between sarcopenia and frailty in older adults.
Conclusion
Screening and assessing frailty in older adults by using the different tools can be an important intervention approach to reduce the negative effects of this phenomenon on personal health and social services. A large number of researchers agree that a common international definition is essential for the development of screening, monitoring, and reduction of frailty’s adverse outcomes in the elderly. Despite the lack of consensus on the definition of frailty, we believe understanding of frailty is not only important from the geriatric medicine opinion, but also is relevant to all medical specialties, as they frequently encounter elderly frail people in daily practices. Therefore training of the health providers for diagnosis and management of frailty is essential.
We also believe that it is impossible to have a consensus over one single definition of frailty and such an expectation is a naïve one. Since the older people are too heterogeneous population to allow one tool to address all types of frailty conditions, and such a definition may even be impossible. We believe that a definition of frailty should have several criteria to refer different domains of health status. This multidimensional approach could be dynamic, predict negative consequences in the target group, and have simplicity in implementation as well as being practical. On the other hand, lack of a “Gold Standard” definition is another problem for future studies in frailty concepts. For this reason, we could not report the pooled sensitivity and specificity of the tools that addressed frailty. Even if we consider consequences such as mortality, disability, hospitalization, and living in a nursing home admission as the main criteria, we will still reach to different precision that are impossible to combine. Therefore, in the absence of a “Gold Standard” definition, it is suggested to choose the most appropriate definition and the most effective evaluation tool will be dependent to the purpose of the research and the characteristics of the elderly population. Future studies may be able to determine to which scopes of these frailty definitions are more associated with cellular and molecular characteristics of cell senescence and the aging process. Recently, some studies in the field of epigenetics have been able to provide a genetic definition of the aging process. Perhaps these definitions can help us determine the sensitivity and specificity of these definitions of frailty.
Declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cesari M, Calvani R, Marzetti E. Frailty in older persons. Clin Geriatr Med. 2017;33(3):293–303. doi: 10.1016/j.cger.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Toward a conceptual definition of frail community dwelling older people. Nurs Outlook. 2010;58(2):76–86. doi: 10.1016/j.outlook.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 3.Theou O, Walston J, Rockwood K. Operationalizing frailty using the frailty phenotype and deficit accumulation approaches. Frailty Aging. 2015;41:66–73. doi: 10.1159/000381164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gustafsson S, Edberg A-K, Dahlin-Ivanoff S. Swedish health care professionals’ view of frailty in older persons. J Appl Gerontol. 2012;31(5):622–640. [Google Scholar]
- 5.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A. 2001;56(3):M146–M157. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 6.Hogan DB. Models, definitions, and criteria for frailty. In: Conn's handbook of models for human aging. Amsterdam: Elsevier; 2018. pp. 35–44.
- 7.Rockwood K. Frailty and its definition: a worthy challenge. J Am Geriatr Soc. 2005;53(6):1069. doi: 10.1111/j.1532-5415.2005.53312.x. [DOI] [PubMed] [Google Scholar]
- 8.Junius-Walker U, Onder G, Soleymani D, Wiese B, Albaina O, Bernabei R, et al. The essence of frailty: a systematic review and qualitative synthesis on frailty concepts and definitions. Eur J Intern Med. 2018;56:3–10. doi: 10.1016/j.ejim.2018.04.023. [DOI] [PubMed] [Google Scholar]
- 9.Rodríguez-Mañas L, Féart C, Mann G, Viña J, Chatterji S, Chodzko-Zajko W, et al. Searching for an operational definition of frailty: a Delphi method based consensus statement. The frailty operative definition-consensus conference project. J Gerontol A. 2013;68(1):62–67. doi: 10.1093/gerona/gls119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Topinková E. Aging, disability and frailty. Ann Nutr Metab. 2008;52(Suppl. 1):6–11. doi: 10.1159/000115340. [DOI] [PubMed] [Google Scholar]
- 11.Anand T, Haddadin Z, Tang AL, Saljuqi ATK, Hamidi MK, Ditillo M, et al. Association of racial, ethnic disparities, and frailty in geriatric trauma patients. J Am Coll Surg. 2019;229(4):S119. [Google Scholar]
- 12.Majid Z, Welch C, Davies J, Jackson T. Global frailty: the role of ethnicity, migration and socioeconomic factors. Maturitas. 2020;139:33–41. doi: 10.1016/j.maturitas.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pradhananga S, Regmi K, Razzaq N, Ettefaghian A, Dey AB, Hewson D. Ethnic differences in the prevalence of frailty in the United Kingdom assessed using the electronic Frailty Index. Aging Med. 2019;2(3):168–173. doi: 10.1002/agm2.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iriarte E, Araya A-X. Frailty criteria among older people living in the community: an update. Rev Med Chile. 2016;144(11):1440–1447. doi: 10.4067/S0034-98872016001100010. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Speechley M, Tinetti M. Falls and injuries in frail and vigorous community elderly persons. J Am Geriatr Soc. 1991;39(1):46–52. doi: 10.1111/j.1532-5415.1991.tb05905.x. [DOI] [PubMed] [Google Scholar]
- 17.Winograd CH, Gerety MB, Brown E, Kolodny V. Targeting the hospitalized elderly for geriatric consultation. J Am Geriatr Soc. 1988;36(12):1113–1119. doi: 10.1111/j.1532-5415.1988.tb04398.x. [DOI] [PubMed] [Google Scholar]
- 18.Bortz WM., II The physics of frailty. J Am Geriatr Soc. 1993;41(9):1004–1008. [PubMed] [Google Scholar]
- 19.Boers M, Jentoft AJC. A new concept of health can improve the definition of frailty. Calcif Tissue Int. 2015;97(5):429–431. doi: 10.1007/s00223-015-0038-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bortz WM. A conceptual framework of frailty: a review. J Gerontol A. 2002;57(5):M283–M288. doi: 10.1093/gerona/57.5.m283. [DOI] [PubMed] [Google Scholar]
- 21.Brown I, Renwick R, Raphael D. Frailty: constructing a common meaning, definition, and conceptual framework. Int J Rehabil Res. 1995;18(2):93–102. [PubMed] [Google Scholar]
- 22.Campbell AJ, Buchner DM. Unstable disability and the fluctuations of frailty. Age Ageing. 1997;26(4):315–318. doi: 10.1093/ageing/26.4.315. [DOI] [PubMed] [Google Scholar]
- 23.Dayhoff NE, Suhrheinrich J, Wigglesworth J, Topp R, Moore S. Balance and muscle strength as predictors of frailty among older adults. J Gerontol Nurs. 1998;24(7):18–27. doi: 10.3928/0098-9134-19980701-06. [DOI] [PubMed] [Google Scholar]
- 24.Gobbens R, Luijkx K, Wijnen-Sponselee MT, Schols J. Towards an integral conceptual model of frailty. J Nutr Health Aging. 2010;14(3):175–181. doi: 10.1007/s12603-010-0045-6. [DOI] [PubMed] [Google Scholar]
- 25.Hamerman D. Toward an understanding of frailty. Ann Intern Med. 1999;130(11):945–950. doi: 10.7326/0003-4819-130-11-199906010-00022. [DOI] [PubMed] [Google Scholar]
- 26.Kaufman SR. The social construction of frailty: an anthropological perspective. J Aging Stud. 1994;8(1):45–58. [Google Scholar]
- 27.Nourhashemi F, Andrieu S, Gillette-Guyonnet S, Vellas B, Albarede JL, Grandjean H. Instrumental activities of daily living as a potential marker of frailty: a study of 7364 community-dwelling elderly women (the EPIDOS study) J Gerontol A. 2001;56(7):M448–M453. doi: 10.1093/gerona/56.7.m448. [DOI] [PubMed] [Google Scholar]
- 28.Ory MG, Schechtman KB, Miller JP, Hadley EC, Fiatarone MA, Province MA, et al. Frailty and injuries in later life: the FICSIT trials. J Am Geriatr Soc. 1993;41(3):283–296. doi: 10.1111/j.1532-5415.1993.tb06707.x. [DOI] [PubMed] [Google Scholar]
- 29.Raphael D, Cava M, Brown I, Renwick R, Heathcote K, Weir N, et al. Frailty: a public health perspective. Can J Public Health = Rev can de sante publique. 1995;86(4):224–227. [PubMed] [Google Scholar]
- 30.Schuurmans H, Steverink N, Lindenberg S, Frieswijk N, Slaets JP. Old or frail: what tells us more? J Gerontol A. 2004;59(9):M962–M965. doi: 10.1093/gerona/59.9.m962. [DOI] [PubMed] [Google Scholar]
- 31.Strawbridge WJ, Shema SJ, Balfour JL, Higby HR, Kaplan GA. Antecedents of frailty over three decades in an older cohort. J Gerontol B. 1998;53(1):S9–S16. doi: 10.1093/geronb/53b.1.s9. [DOI] [PubMed] [Google Scholar]
- 32.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 33.Lachs MS, Feinstein AR, Cooney LM, Jr, Drickamer MA, Marottoli RA, Pannill FC, et al. A simple procedure for general screening for functional disability in elderly patients. Ann Intern Med. 1990;112(9):699–706. doi: 10.7326/0003-4819-112-9-699. [DOI] [PubMed] [Google Scholar]
- 34.Winograd CH, Gerety MB, Chung M, Goldstein MK, Dominguez F, Jr, Vallone R. Screening for frailty: criteria and predictors of outcomes. J Am Geriatr Soc. 1991;39(8):778–784. doi: 10.1111/j.1532-5415.1991.tb02700.x. [DOI] [PubMed] [Google Scholar]
- 35.Brown M, Sinacore DR, Binder EF, Kohrt WM. Physical and performance measures for the identification of mild to moderate frailty. J Gerontol A. 2000;55(6):M350–M355. doi: 10.1093/gerona/55.6.m350. [DOI] [PubMed] [Google Scholar]
- 36.Mitnitski AB, Graham JE, Mogilner AJ, Rockwood K. Frailty, fitness and late-life mortality in relation to chronological and biological age. BMC Geriatr. 2002;2(1):1–8. doi: 10.1186/1471-2318-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J. 2001;1:323–336. doi: 10.1100/tsw.2001.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paw MJCA, Dekker JM, Feskens EJ, Schouten EG, Kromhout D. How to select a frail elderly population? A comparison of three working definitions. J Clin Epidemiol. 1999;52(11):1015–1021. doi: 10.1016/s0895-4356(99)00077-3. [DOI] [PubMed] [Google Scholar]
- 39.Saliba D, Elliott M, Rubenstein LZ, Solomon DH, Young RT, Kamberg CJ, et al. The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc. 2001;49(12):1691–1699. doi: 10.1046/j.1532-5415.2001.49281.x. [DOI] [PubMed] [Google Scholar]
- 40.Cesari M, Demougeot L, Boccalon H, Guyonnet S, Van Kan GA, Vellas B, et al. A self-reported screening tool for detecting community-dwelling older persons with frailty syndrome in the absence of mobility disability: the FiND questionnaire. PLoS ONE. 2014;9(7):e101745. doi: 10.1371/journal.pone.0101745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Cawthon PM, Stone KL, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med. 2008;168(4):382–389. doi: 10.1001/archinternmed.2007.113. [DOI] [PubMed] [Google Scholar]
- 42.García-García FJ, Carcaillon L, Fernandez-Tresguerres J, Alfaro A, Larrion JL, Castillo C, et al. A new operational definition of frailty: the Frailty Trait Scale. J Am Med Dir Assoc. 2014;15(5):371.e7–e13. doi: 10.1016/j.jamda.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 43.Garre-Olmo J, Calvó-Perxas L, López-Pousa S, de Gracia BM, Vilalta-Franch J. Prevalence of frailty phenotypes and risk of mortality in a community-dwelling elderly cohort. Age Ageing. 2013;42(1):46–51. doi: 10.1093/ageing/afs047. [DOI] [PubMed] [Google Scholar]
- 44.Gobbens RJ, van Assen MA, Luijkx KG, Wijnen-Sponselee MT, Schols JM. The Tilburg frailty indicator: psychometric properties. J Am Med Dir Assoc. 2010;11(5):344–355. doi: 10.1016/j.jamda.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 45.Goldstein J, Hubbard RE, Moorhouse P, Andrew MK, Mitnitski A, Rockwood K. The validation of a care partner-derived frailty index based upon comprehensive geriatric assessment (CP-FI-CGA) in emergency medical services and geriatric ambulatory care. Age Ageing. 2015;44(2):327–330. doi: 10.1093/ageing/afu161. [DOI] [PubMed] [Google Scholar]
- 46.Jones DM, Song X, Rockwood K. Operationalizing a frailty index from a standardized comprehensive geriatric assessment. J Am Geriatr Soc. 2004;52(11):1929–1933. doi: 10.1111/j.1532-5415.2004.52521.x. [DOI] [PubMed] [Google Scholar]
- 47.Lee DH, Buth KJ, Martin B-J, Yip AM, Hirsch GM. Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation. 2010;121(8):973. doi: 10.1161/CIRCULATIONAHA.108.841437. [DOI] [PubMed] [Google Scholar]
- 48.Ng TP, Feng L, Nyunt MSZ, Larbi A, Yap KB. Frailty in older persons: multisystem risk factors and the Frailty Risk Index (FRI) J Am Med Dir Assoc. 2014;15(9):635–642. doi: 10.1016/j.jamda.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 49.Overcash JA, Beckstead J, Extermann M, Cobb S. The abbreviated comprehensive geriatric assessment (aCGA): a retrospective analysis. Crit Rev Oncol/Hematol. 2005;54(2):129–136. doi: 10.1016/j.critrevonc.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 50.Puts M, Lips P, Deeg D. Static and dynamic measures of frailty predicted decline in performance-based and self-reported physical functioning. J Clin Epidemiol. 2005;58(11):1188–1198. doi: 10.1016/j.jclinepi.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 51.Robinson TN, Eiseman B, Wallace JI, Church SD, McFann KK, Pfister SM, et al. Redefining geriatric preoperative assessment using frailty, disability and co-morbidity. Ann Surg. 2009;250(3):449–455. doi: 10.1097/SLA.0b013e3181b45598. [DOI] [PubMed] [Google Scholar]
- 52.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J. 2005;173(5):489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton Frail Scale. Age Ageing. 2006;35(5):526–529. doi: 10.1093/ageing/afl041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Romero-Ortuno R, Walsh CD, Lawlor BA, Kenny RA. A frailty instrument for primary care: findings from the Survey of Health, Ageing and Retirement in Europe (SHARE) BMC Geriatr. 2010;10(1):57. doi: 10.1186/1471-2318-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Studenski S, Hayes RP, Leibowitz RQ, Bode R, Lavery L, Walston J, et al. Clinical global impression of change in physical frailty: development of a measure based on clinical judgment. J Am Geriatr Soc. 2004;52(9):1560–1566. doi: 10.1111/j.1532-5415.2004.52423.x. [DOI] [PubMed] [Google Scholar]
- 56.Hoogendijk EO, Theou O, Rockwood K, Onwuteaka-Philipsen BD, Deeg DJ, Huisman M. Development and validation of a frailty index in the Longitudinal Aging Study Amsterdam. Aging Clin Exp Res. 2017;29(5):927–933. doi: 10.1007/s40520-016-0689-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kajsa E, Katarina W, Sten L, Synneve I-D. Screening for frailty among older emergency department visitors: validation of the new FRESH-screening instrument. BMC Emerg Med. 2016;16(1):1–7. doi: 10.1186/s12873-016-0087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Makizako H, Shimada H, Tsutsumimoto K, Lee S, Doi T, Nakakubo S, et al. Social frailty in community-dwelling older adults as a risk factor for disability. J Am Med Dir Assoc. 2015;16(11):1003.e7–e11. doi: 10.1016/j.jamda.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 59.Morris JN, Howard EP, Steel KR. Development of the interRAI home care frailty scale. BMC Geriatr. 2016;16(1):188. doi: 10.1186/s12877-016-0364-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vernerey D, Anota A, Vandel P, Paget-Bailly S, Dion M, Bailly V, et al. Development and validation of the FRAGIRE tool for assessment an older person’s risk for frailty. BMC Geriatr. 2016;16(1):187. doi: 10.1186/s12877-016-0360-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yamada M, Arai H. Predictive value of frailty scores for healthy life expectancy in community-dwelling older Japanese adults. J Am Med Dir Assoc. 2015;16(11):1002.e7–e11. doi: 10.1016/j.jamda.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 62.Andrew MK, Rockwood K. Social vulnerability predicts cognitive decline in a prospective cohort of older Canadians. Alzheimer's Dement. 2010;6(4):319–25.e1. doi: 10.1016/j.jalz.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 63.Freiheit EA, Hogan DB, Eliasziw M, Meekes MF, Ghali WA, Partlo LA, et al. Development of a frailty index for patients with coronary artery disease. J Am Geriatr Soc. 2010;58(8):1526–1531. doi: 10.1111/j.1532-5415.2010.02961.x. [DOI] [PubMed] [Google Scholar]
- 64.Hábert R, Bravo G, Korner-Bitensky N, Voyer L. Predictive validity of a postal questionnaire for screening community-dwelling elderly individuals at risk of functional decline. Age Ageing. 1996;25(2):159–167. doi: 10.1093/ageing/25.2.159. [DOI] [PubMed] [Google Scholar]
- 65.Joseph B, Pandit V, Zangbar B, Kulvatunyou N, Tang A, O'Keeffe T, et al. Validating trauma-specific frailty index for geriatric trauma patients: a prospective analysis. J Am Coll Surg. 2014;219(1):10–7.e1. doi: 10.1016/j.jamcollsurg.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 66.Ma L, Zhang L, Tang Z, Sun F, Diao L, Wang J, et al. Use of the frailty index in evaluating the prognosis of older people in Beijing: a cohort study with an 8-year follow-up. Arch Gerontol Geriatr. 2016;64:172–177. doi: 10.1016/j.archger.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 67.Raîche M, Hébert R, Dubois M-F. PRISMA-7: a case-finding tool to identify older adults with moderate to severe disabilities. Arch Gerontol Geriatr. 2008;47(1):9–18. doi: 10.1016/j.archger.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 68.Ravaglia G, Forti P, Lucicesare A, Pisacane N, Rietti E, Patterson C. Development of an easy prognostic score for frailty outcomes in the aged. Age Ageing. 2008;37(2):161–166. doi: 10.1093/ageing/afm195. [DOI] [PubMed] [Google Scholar]
- 69.Rockwood K, Fox RA, Stolee P, Robertson D, Beattie BL. Frailty in elderly people: an evolving concept. Can Med Assoc J. 1994;150(4):489. [PMC free article] [PubMed] [Google Scholar]
- 70.Scarcella P, Liotta G, Marazzi M, Carbini R, Palombi L. Analysis of survival in a sample of elderly patients from Ragusa, Italy on the basis of a primary care level multidimensional evaluation. Arch Gerontol Geriatr. 2005;40(2):147–156. doi: 10.1016/j.archger.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 71.Teo N, Gao Q, Nyunt MSZ, Wee SL, Ng T-P. Social frailty and functional disability: findings from the Singapore Longitudinal Ageing Studies. J Am Med Dir Assoc. 2017;18(7):637.e13–e19. doi: 10.1016/j.jamda.2017.04.015. [DOI] [PubMed] [Google Scholar]
- 72.Bergman H, Beland F, Karunananthan S, Hummel S, Hogan D, Wolfson C. Developing a working framework for understanding frailty Howard Bergman, MD. Gérontol soc. 2004;109:15–29. [Google Scholar]
- 73.Buchner DM, Wagner EH. Preventing frail health. Clin Geriatr Med. 1992;8(1):1–18. [PubMed] [Google Scholar]
- 74.de Moraes EN, do Carmo JA, de Moraes FL, Azevedo RS, Machado CJ, Montilla DER. Clinical-Functional Vulnerability Index-20 (IVCF-20): rapid recognition of frail older adults. Rev saúde pública. 2016;50:81. doi: 10.1590/S1518-8787.2016050006963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nunes DP, de Oilveira Duarte YA, Santos JLF, Lebrão ML. Screening for frailty in older adults using a self-reported instrument. Rev saude publica. 2015;49:2. doi: 10.1590/S0034-8910.2015049005516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shinkai S, Watanabe N, Yoshida H, Fujiwara Y, Amano H, Lee S, et al. Research on screening for frailty: development of “the Kaigo-Yobo Checklist”. [Nihon koshu eisei zasshi] Jpn J Public Health. 2010;57(5):345. [PubMed] [Google Scholar]
- 77.Hwang HS, Kwon IS, Park BJ, Cho B, Yoon JL, Won CW. The validity and reliability of Korean frailty index. J Korean Geriatr Soc. 2010;14(4):191–202. [Google Scholar]
- 78.Dapp U, Anders J, Golgert S, Renteln-Kruse WV, Minder C. The LUCAS-I marker set for a classification of elderly people as fit, pre-frail and frail. First results on validity from the Longitudinal Urban Cohort Aging Study (LUCAS), Hamburg. J Gerontol Geriatr. 2012;45:262–270. doi: 10.1007/s00391-012-0311-9. [DOI] [PubMed] [Google Scholar]
- 79.Sewo Sampaio PY, Sampaio RAC, Yamada M, Arai H. Systematic review of the Kihon Checklist: is it a reliable assessment of frailty? Geriatr Gerontol Int. 2016;16(8):893–902. doi: 10.1111/ggi.12833. [DOI] [PubMed] [Google Scholar]
- 80.Van Kan GA, Rolland Y, Bergman H, Morley J, Kritchevsky S, Vellas B. The IANA Task Force on frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008;12(1):29–37. doi: 10.1007/BF02982161. [DOI] [PubMed] [Google Scholar]
- 81.Cesari M, Gambassi G, Abellan van Kan G, Vellas B. The frailty phenotype and the frailty index: different instruments for different purposes. Age Ageing. 2014;43(1):10–12. doi: 10.1093/ageing/aft160. [DOI] [PubMed] [Google Scholar]
- 82.Yvonne Kaethler M, Molnar FJ, Susan L. Defining the concept of frailty: a survey of multi-disciplinary health professionals. Geriatr Today. 2003;6:26–31. [Google Scholar]
- 83.Xue Q-L. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011;27(1):1–15. doi: 10.1016/j.cger.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. 2018;47(2):193–200. doi: 10.1093/ageing/afx162. [DOI] [PubMed] [Google Scholar]
- 85.van Kan GA, Rolland YM, Morley JE, Vellas B. Frailty: toward a clinical definition. J Am Med Dir Assoc. 2008;9(2):71–72. doi: 10.1016/j.jamda.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 86.Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthan S, et al. Frailty: an emerging research and clinical paradigm—issues and controversies. J Gerontol A. 2007;62(7):731–737. doi: 10.1093/gerona/62.7.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Morley JE, Malmstrom T, Miller D. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi: 10.1007/s12603-012-0084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lorenzo-López L, Maseda A, de Labra C, Regueiro-Folgueira L, Rodríguez-Villamil JL, Millán-Calenti JC. Nutritional determinants of frailty in older adults: a systematic review. BMC Geriatr. 2017;17(1):108. doi: 10.1186/s12877-017-0496-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Villacampa-Fernandez P, Navarro-Pardo E, Tarin JJ, Cano A. Frailty and multimorbidity: two related yet different concepts. Maturitas. 2017;95:31–35. doi: 10.1016/j.maturitas.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 90.Kulminski AM, Ukraintseva SV, Kulminskaya IV, Arbeev KG, Land K, Yashin AI. Cumulative deficits better characterize susceptibility to death in elderly people than phenotypic frailty: lessons from the Cardiovascular Health Study. J Am Geriatr Soc. 2008;56(5):898–903. doi: 10.1111/j.1532-5415.2008.01656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Berrut G, Andrieu S, De Carvalho IA, Baeyens J, Bergman H, Cassim B, et al. Promoting access to innovation for frail old persons. J Nutr Health Aging. 2013;17(8):688–693. doi: 10.1007/s12603-013-0039-2. [DOI] [PubMed] [Google Scholar]
- 92.Bunt S, Steverink N, Olthof J, van der Schans C, Hobbelen J. Social frailty in older adults: a scoping review. Eur J Ageing. 2017;14(3):323–334. doi: 10.1007/s10433-017-0414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Teixeira IND. The perception of health professionals of two definitions of frailty in elderly people. Cienc saude colet. 2008;13(4):1181–1188. doi: 10.1590/s1413-81232008000400014. [DOI] [PubMed] [Google Scholar]
- 94.Markle-Reid M, Browne G. Conceptualizations of frailty in relation to older adults. J Adv Nurs. 2003;44(1):58–68. doi: 10.1046/j.1365-2648.2003.02767.x. [DOI] [PubMed] [Google Scholar]
- 95.Rockwood K. What would make a definition of frailty successful? Age Ageing. 2005;34(5):432–434. doi: 10.1093/ageing/afi146. [DOI] [PubMed] [Google Scholar]
- 96.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A. 2004;59(3):M255–M263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 97.Espinoza SE, Quiben M, Hazuda HP. Distinguishing comorbidity, disability, and frailty. Curr Geriatr Rep. 2018;7(4):201–209. doi: 10.1007/s13670-018-0254-0. [DOI] [PMC free article] [PubMed] [Google Scholar]