Abstract
Background
Drivers are one of the trade unions that are most exposed to various health-related risks, especially metabolic diseases. The present study aimed to systematically assess the overall prevalence of metabolic syndrome and its determinants among drivers in the world.
Methods
All retrospective, cross-sectional, or prospective studies evaluating the prevalence and risk for metabolic syndrome and its main components among male professional drivers were eligible for the initial assessment. PRISMA guideline was used. Two blinded reviewers independently screened the titles and abstracts of the manuscripts followed by a deep assessment of the full texts for determining the inclusion appropriateness.
Results
In the final, 12 articles were eligible for the final analysis. Overall, 19,350 professional male drivers with a total average age of 43.06 years (ranged from 35.5 to 51.1 years) were included in the study. The prevalence of metabolic syndrome was estimated to be 32.8% (95%CI: 32.1% to 33.5%), and the major determinants of appearing this syndrome among professional drivers were advanced age, years of driving experience, higher body mass index, smoking, high cholesterol dietary regimen, high Framingham risk score, low regular exercising, history of diabetes mellitus, history of gout, and shift work pattern.
Conclusion
According to the 32.8% prevalence rate of metabolic syndrome among drivers, managerial measures are needed to prevent and control metabolic disturbances among professional drivers are recommended.
Keywords: Metabolic syndrome, Professional driver, Cardiovascular risk
Introduction
Metabolic syndrome or syndrome X is a set of metabolic and non-metabolic components including high fasting plasma glucose, increased blood triglyceride, hypertension, low HDL(high density lipoprotein) cholesterol and abdominal obesity [1, 2]. Metabolic syndrome increases the risk of diabetes, cardiovascular disease, dyslipidemia, stroke, osteoarthritis and some types of cancers leading higher likelihood of death [3–5].
The overall prevalence of metabolic syndrome in the population over the age of 20 in the United States, according to the definition of the World Health Organization, is about 25% and is also estimated to be 22 to 24% based on the criteria of Adult Treatment Panel III (ATP III) [6–8]. The prevalence of the metabolic syndrome as defined by the International Diabetes Federation (IDF) in the general American population is 39 ± 1.1% [9]. The prevalence of metabolic syndrome in seven major European countries is about 23% [10]. In Canada, about a quarter of the population aged 35–75 have metabolic syndrome, according to the World Health Organization criteria [11]. In South Asia, the prevalence of metabolic syndrome is estimated at 20–25% [12, 13].
There are some sedentary Jobs such as driving with high emotional demands and long working hours that considered safety critical jobs. Drivers are one of the trade unions that are most exposed to various health-related risks, especially metabolic diseases due to the nature of their job and unhealthy diet [14]. Studies have shown that job stress, inactivity, work shifts, and changing eating habits are among the major health risks for drivers, which can put them at greater risk for obesity and high blood pressure, which are known to be risk factors for metabolic syndrome [15, 16].
These disorders also affect the health status of people and increase the risk of road accidents, increase absenteeism and even cause temporary and permanent disabilities in drivers, and as a result, effect the driver’s health and safe driving which in turn impose a great economic burden on society [17].
Due to the working conditions of the drivers, they are more prone to such diseases, especially the components of metabolic syndrome and its complications. Studies among drivers have significantly linked metabolic disorders to obesity, and lipid profiles disturbances such as low HDL cholesterol, and high triglycerides; according to these studies, the risk of low HDL cholesterol in drivers with high shift work is twice as high as others [18, 19]. Most of the professional driver involved in the rotating shift works due to their requirements. Shift works also cause a mismatch between the body’s internal rhythm and the circadian rhythm, which in turn leads to symptoms such as sleep disorders and fatigue. The results of studies show that shift work can affect the cardiovascular and metabolic systems and cause weight gain, high blood pressure levels and increased incidence of metabolic syndrome [20, 21].
Given the prevalence of metabolic syndrome and the severe health and economic consequences of this event, epidemiological studies show an excess risk for cardiovascular diseases and musculoskeletal disorders in professional drivers [22]. The value of the metabolic syndrome as a predictor of cardiovascular risk has a great importance in drivers. In this statement, it seems the need to identify the cardiovascular risk associated with the metabolic syndrome in derivers. A large number of observational studies have been carried out to investigate the frequency, and there is a need to synthesize the results of these studies. Thus, our objective was to carry out a systematic review and meta-analysis to estimate the prevalence of the metabolic syndrome and its determinants such as obesity, diabetes, dyslipidemia and hypertension in professional drivers as one of the high-risk occupational groups.
Materials and methods
Information sources
For performing the present systematic review and meta-analysis, the full guideline of the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” was followed [23]. After explaining the study’s main question and specific goals, all prospective and retrospective comparative cross-sectional studies that evaluated the prevalence and risk for metabolic syndrome and its main components among drivers were considered to be eligible for primary assessment. There are some definitions for metabolic syndrome, which the most widely used are the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) and the International Diabetes Federation (IDF). Diagnostic criteria of metabolic syndrome according to National Cholesterol Education Programs Adult Treatment Panel III have been based on any three of the following 5 features: 1. Increased waist circumference (≥ 102 cm in men ≥ 88 cm in women) which as defined as abdominal obesity 2. Triglyceride≥ 1.7 mmol/l or TG treatment 3. HDL-C (Men < 1.03 mmol/l or women < 1.29 mmol/l) or HDL-C treatment 4. Blood pressure: Systolic ≥ 130 mmHg or Diastolic ≥ 85 mmHg or hypertension treatment or previously diagnosed hypertension 5. Fasting blood glucose ≥ 5.6 mmol/l or treatment for elevated glucose or previously diagnosed Type 2 Diabetes. The IDF criteria include increased waist circumference Men ≥ 90 cm, Women ≥ 80 cm along with any 2 of other above-mentioned features.
[5, 24] In this regard, deep searching the manuscript databanks including PubMed, SCOPUS, Google Scholar, and Web of knowledge was planned from inception from 2000 to 2020. The following key words were uses: metabolic syndrome, insulin resistance syndrome, metabolic abnormalities, adult Treatment Panel III, syndrome X, drivers, professional drivers.
Selection process
All of the research which had mentioned the prevalence of metabolic syndrome in drivers was included in our study and the review papers, case presentations, letter to editors, and abstracts without full text access and female drivers as the population of the study and non-English written articles were all excluded. Also, in cases of lack of access to the full text of the articles, correspondence was made with the author in charge of the articles to obtain the full article, and in case of lack of access to the original article; it was removed from the study. The manuscript reviewing was done by the two blinded reviewers independently screened the titles and abstracts of the manuscripts followed by deeply assessment of the full texts for determining the inclusion appropriateness. The presence of any disagreement between them was judged and rechecked by the third reviewer as the final arbitrator. The details of eligibility and the reasons for excluding the papers were schematically shown in Fig. 1.
Fig. 1.
The flowchart of screening the eligible studies (Using PRISMA guideline)
Study risk of bias assessment
Before finalizing the meta-analysis, the risk of bias was evaluated blindly by the two authors using the Cochrane Q test risk of bias tool that the level of bias was qualitatively classified as at high, unclear or low risk of bias [25]. In this regard, the following domains are routinely assessed for determining the level of bias: how selection the participants (selection bias), and how managing confounders and missing data.
Synthesis methods
The fixed effects or random-effects (in case of significant heterogeneity across the data) models were used to obtained pooled prevalence of metabolic syndrome. All authors contributed in the translation. The heterogeneity between the studies was evaluated by determining I2 values. A sensitivity analysis was also performed, in which observational studies at critical risk of bias were excluded from the analysis (22 studies). Publication bias was also assessed by the funnel plot analysis. Reported values were two-tailed, and hypothesis testing results were considered statistically significant at p < 0.05. For statistical analysis, the Comprehensive Meta-Analysis Software (CMA, version 3.0) was employed.
Results
The flow diagram of the study selection process is presented in Fig. 1. In this context, 84 articles were initially collected by database searching. After removing 12 articles due to evidence of duplication, 72 records were primarily under-screened. Based on the titles and abstracts, 57 records were excluded and the remaining 15 citations were assessed for further eligibility. Of those, 3 were also excluded due to incompleteness of the data and contents. In the final, 12 articles were eligible for the final analysis [20, 26–36]. Table 1 describes the baseline characteristics of the studies included.
Table 1.
The details of studies included into meta-analysis
| Author, year | Country | Study type | Mets* criteria | sample size (n) | Mean ± SD age | Type of driver |
|---|---|---|---|---|---|---|
| Appiah et al., 2020 | Ghana | Cross- sectional | NCEP-ATP III | 100 | 41.0 ± 8.9 | Taxi |
| Cavagioni et al., 2008 | Brazil | Cross- sectional | Brazilian Guideline for Diagnosis and Treatment of the Metabolic Syndrome | 258 | 35.5 ± 10.1 | Truck |
| Chen et al., 2013 | Taiwan | Cross- sectional | NCEP-ATP III | 441 | 46.5 ± 9.4 | Truck, taxi, bus, trailer |
| Ebrahimi et al., 2015 | Iran | Cross- sectional | NCEP-ATP III, IDF | 1018 | 42.1 ± 10.6 | Truck, bus, minibus, taxi |
| Lemke et al., 2017 | United states | Cross- sectional | NCEP-ATP III | 262 | 46.6 ± 10.5 | Truck |
| Mohebbi et al., 2012 | Iran | Cross- sectional | IDF | 12,138 | 37.8 ± 10.1 | Truck, bus |
| Montazerifar et al., 2019 | Iran | Cross- sectional | Iranian National Committee of Obesity | 200 | 42.5 ± 10.0 | Taxi |
| Robbins et al., 2020 | United states | Cross- sectional | IDF | 817 | 45.5 ± 11.0 | Truck |
| Rodríguez et al., 2017 | Colombia | Cross- sectional | NCEP-ATPIII | 117 | 45.8 ± 10.5 | Truck, bus |
| Saberi et al., 2011 | Iran | Cross- sectional | NCEP-ATPIII | 429 | 36.6 ± 10.7 | Truck, bus |
| Shin et al., 2013 | Korea | Cross- sectional | NCEP-ATPIII | 443 | 45.7 ± 11.2 | Bus |
| Siu et al., 2012 | China | Cross- sectional | IDF | 3127 | 51.1 ± 7.7 | Truck, taxi, bus |
*Metabolic syndrome
Overall, 19,350 professional male drivers with a total average age of 43.06 ± 8.8 years (ranged 35.5 to 51.1 years were included in the study. Description of the studies included in the Meta-analysis is shown in Table 1. Also, various motor vehicles were considered in different studies including taxi, bus, minibus, and lorry, truck, and trailer however in some studies. These devices were not separated from each other and were considered together. Therefore, in the final analysis, we were not able to differentiate the data analysis by vehicle type. Most studies were performed in Asian countries, while we did not reveal a comprehensive study among European areas.
As summarized in Table 2, the prevalence of metabolic syndrome among professional drivers widely ranged 5% to 58% in Ghana (Appiah, 2020) and the United States (Lemke, 2017) respectively. In relation to total average of the 12 studies evaluated in the review, the pooled prevalence of metabolic syndrome among drivers was estimated to be 32.8% (95%CI: 32.1% to 33.5%). With respect to the prevalence of each component of metabolic syndrome, the overall prevalence of obesity was 51.6% (95%CI: 50.9% to 52.4%), the prevalence of hypertension was 45.1% (95%CI: 44.4% to 45.9%), the prevalence of diabetes mellitus was 17.5% (95%CI: 16.9% to 18.0%) and the overall prevalence of dyslipidemia was 48.7% (95%CI: 48.0% to 49.4%) (Figs. 2, 3, 4, 5 and 6). The heterogeneity across the studies in all measurements was significantly relevant with the I2 values ranged 96.6% to 98.7%. Also, the significant publication of bias was revealed in all published studies according to the funnel plot drawn with the p values ranged from 0.631 to 0.999.
Table 2.
The pooled prevalence of metabolic syndrome and its determinants
| Author, year | Prevalence of MetS* | Obesity | Hypertension | Diabetes mellitus | Dyslipidemia |
|---|---|---|---|---|---|
| Appiah, 2020 | 5.0% | 13.0% | 63.0% | 12.0% | 40.0% |
| Cavagioni, 2008 | 24.0% | 36.0% | 59.0% | 7.0% | 35.0% |
| Chen, 2013 | 43.1% | 22.5% | 58.9% | 20.1% | 47.6% |
| Ebrahimi, 2015 | 26.1% | 25.2% | 12.7% | 13.3% | 56.3% |
| Lemke, 2017 | 58.0% | 79.0% | 28.0% | 17.0% | 50.0% |
| Mohebbi, 2012 | 32.4% | 51.9% | 44.6% | 17.5% | 45.5% |
| Montazerifar, 2019 | 20.0% | 64.4% | 28.8% | 35.6% | 81.4% |
| Robbins, 2020 | 52.4% | 77.0% | 21.2% | 11.9% | 67.6% |
| Rodríguez, 2017 | 49.5% | 51.7% | 13.8% | 5.3% | 64.6% |
| Saberi, 2011 | 35.9% | 68.3% | 72.0% | 83.9% | 46.6% |
| Shin, 2013 | 49.9% | 53.3% | 53.3% | 28.6% | 44.6% |
| Siu, 2012 | 25.2% | 52.7% | 53.5% | 9.2% | 54.3% |
*Metabolic syndrome
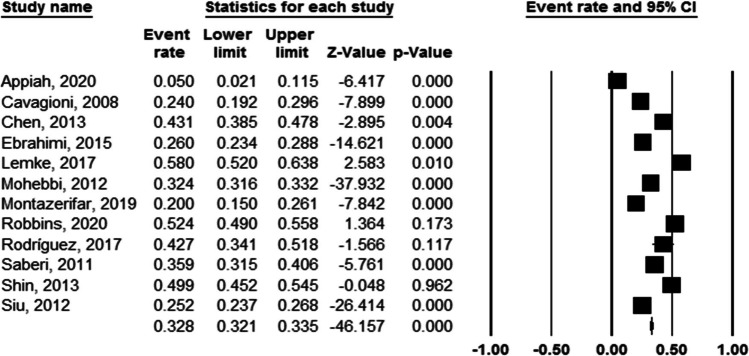
Fig. 2.
Forest plots of pooled prevalence of metabolic syndrome. (Heterogeneity I2 value = 96.6%, p < 0.001, significant publication bias (p = 0.769). The pooled prevalence of metabolic syndrome: 32.8% (95%CI: 32.1% to 33.5%)
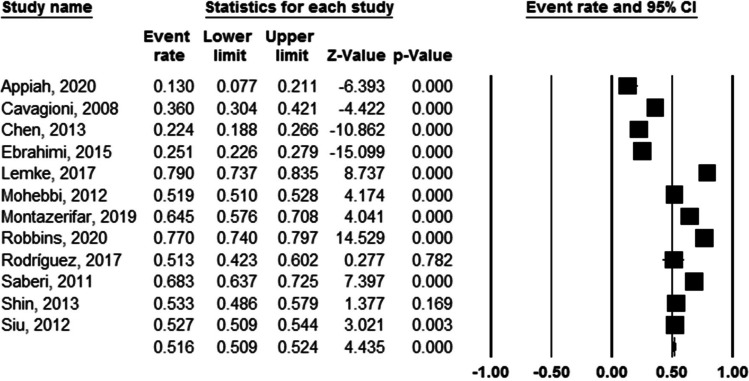
Fig. 3.
Forest plots of pooled prevalence of obesity. (Heterogeneity I2 value = 97.2%, p < 0.001, significant publication bias (p = 0.852). The pooled prevalence of obesity: 51.6% (95%CI: 50.9% to 52.4%)
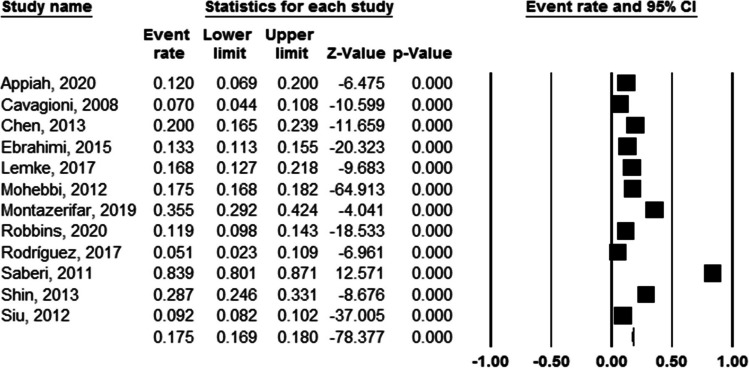
Fig. 4.
Forest plots of pooled prevalence of hypertension. (Heterogeneity I2 value = 98.7%, p < 0.001, significant publication bias (p = 0.998). The pooled prevalence of hypertension was 45.1% (95%CI: 44.4% to 45.9%)
Fig. 5.
Forest plots of pooled prevalence of diabetes mellitus. (Heterogeneity I2 value = 97.5%, p < 0.001, significant publication bias (p = 0.876). The prevalence of diabetes mellitus was 17.5% (95%CI: 16.9% to 18.0%)
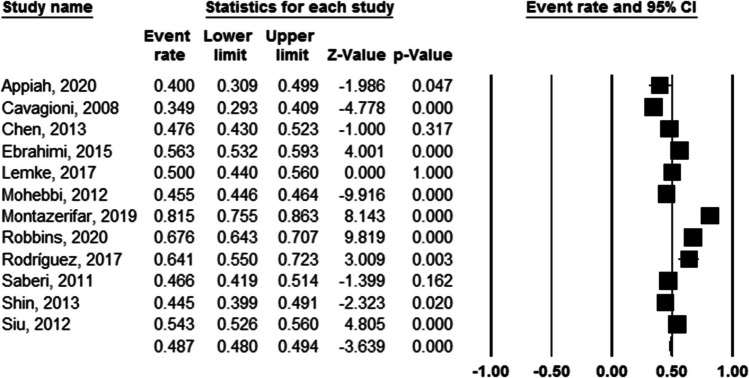
Fig. 6.
Forest plots of pooled prevalence of dyslipidemia. (Heterogeneity I2 value = 96.9%, p < 0.001, significant publication bias (p = 0.631). The pooled prevalence of dyslipidemia was 48.7% (95%CI: 48.0% to 49.4%)
With regard to the main indicators for metabolic syndrome among drivers, the major determinants of appearing this syndrome among professional drivers were advanced age, years of driving experience, higher body mass index, smoking, high cholesterol dietary regimen, high Framingham risk score (Framingham score is a gender-specific algorithm used to estimate the 10-year cardiovascular risk of an individual and is consisted of age, smoking status, total cholesterol, HDL cholesterol and systolic blood pressure) [37], low regular exercising, history of diabetes mellitus, history of gout, and Shift work pattern (Table 3).
Table 3.
Main determinants of metabolic syndrome among professional drivers
| Author, year | Main determinants of metabolic syndrome |
|---|---|
| Appiah, 2020 | Smoking, time for supper |
| Cavagioni, 2008 | High cholesterol habit, high Framingham risk score, body mass index |
| Chen, 2013 | Age, history of diabetes mellitus, history of gout, betel nut chewing, Albuminuria |
| Ebrahimi, 2015 | – |
| Lemke, 2017 | Driving experience, work day sleep quality |
| Mohebbi, 2012 | Weekly driving duration, driving experiences, smoking, age, body mass index |
| Montazerifar, 2019 | Driving experiences, age, physical activity |
| Robbins, 2020 | – |
| Rodríguez, 2017 | Age, body mass index, weekly exercise |
| Saberi, 2011 | – |
| Shin, 2013 | Shift pattern, age, driving experiences |
| Siu, 2012 | – |
Assessment of publication and systematic bias showed that almost all studies were considered as low risk or with unclear biases and thus the obtained results could be considered valid and none of the citations was determined to have a high risk of bias (Table 4).
Table 4.
The Assessment of the risk of bias
| Authors | Patient selection | Index test | Outcomes measuring | Flow and timing |
|---|---|---|---|---|
| Appiah, 2020 | + | ? | ? | + |
| Cavagioni, 2008 | ? | ? | ? | + |
| Chen, 2013 | ? | + | + | + |
| Ebrahimi, 2015 | + | + | + | + |
| Lemke, 2017 | ? | + | + | + |
| Mohebbi, 2012 | + | + | + | ? |
| Montazerifar, 2019 | ? | ? | ? | + |
| Robbins, 2020 | ? | ? | ? | + |
| Rodríguez, 2017 | + | + | + | + |
| Saberi, 2011 | + | ? | ? | + |
| Shin, 2013 | + | + | + | + |
| Siu, 2012 | + | + | ? | ? |
Discussion
Overall, about one-third of drivers suffered from the metabolic syndrome that seems to be considerably high. Similar to our study, a metanalysis which was completed in 2016, revealed that the prevalence of metabolic syndrome was 34% [38]. The observed global prevalence of metabolic syndrome was reported 20–25% [39]. Our meta-analysis revealed 32.8% prevalence rate of metabolic syndrome among professional drivers regardless of driving system. In fact, categorizing of type of vehicles was not possible because most studies pointed to the term of professional driving. Overall, about one-third of drivers suffered from the metabolic syndrome that seems to be considerably high. The highest prevalence of metabolic syndrome was reported among definitive components of this syndrome, the most prevalent profile was obesity in 51.6%, followed by dyslipidemia in 48.7%, hypertension in 45.1%, and diabetes mellitus in 17.5%.
Long and irregular working hours and shift works which are the nature of drivers’ work lead to sleep deprivation and disruption of circadian rhythm are the important factors leading to overweight and specially abdominal obesity [40]. sedentary lifestyles, unhealthy diet, smoking and high blood pressure predispose professional drivers to cardiovascular disease [41].
Comparing data across the different countries shows a significant difference in the rate of metabolic syndrome and especially in its components. Regarding the prevalence rate of metabolic syndrome, the highest rates were found in the developed and industrialized countries especially the United States Lemke (58.0%), while the lowest prevalence rate could be found in African nations Appiah (5.0%) [33, 35]. In this regard, a higher rate of obesity (ranged 77 to 79%) is clearly shown in Western countries as compared to Eastern areas leading higher prevalence rate of metabolic syndrome among the former areas. Moreover, due to heavy vehicle activities due to high levels of economic activity and sedentary lifestyle accompanied with western diet in industrialized countries has increased prevalence of metabolic syndrome [42]. Furthermore, western diet increases body adipose tissue so increases prevalence of metabolic syndrome [43].
However, we faced high heterogeneities across the studies in estimating the prevalence of metabolic syndrome and its metabolic determinants. The reason for this variation is first applying different diagnostic criteria for defining a metabolic syndrome and also for its defining criteria that it is recommended that instead of using internationally defined criteria, each community should use its own standardized criteria for metabolic syndrome according to the metabolic conditions of that community. In fact, many of the normalized defining indicators of this disease, such as anthropometric indicators, are very different between communities. On the other hand, the measurement of these indicators has been completely different in different studies, sometimes based on a single query from patients, sometimes based on the existence of clinical evidence and sometimes by different people and instruments with different measurement accuracy. Such significant differences can lead to heterogeneity between the results of the studies. Also, due to the change in the prevalence of each of the defining indicators of the disease during the last decade due to the arrangements of the health organizations of the countries, it is obvious that the level of control of these indicators in different studies that have been published in different years is completely different.
Metabolic syndrome is an important medical issue specially in specific occupational groups such as drivers due to the increasing sedentary lifestyle and unhealthy diet. Therefore, the importance of medical assessment through a well-defined screening program seems necessary for driver safety.
The major strength of the study is that we have tried to provide a comprehensive review on the frequency of metabolic syndrome and its components among professional drivers.
Limitations
However, our study has some limitations. Summarizing and concluding the frequency of metabolic syndrome in professional drivers with different demographic and socio-economic characteristics is complicated. Also, all of the studies didn’t use the same definition for metabolic syndrome. Different lab kits and fasting status of studies participants’ could be considered as biases of the studies. Different measurement instruments for height and weight also can be a source of bias between the studies.
Conclusion
Overall, what can be deduced from the review of studies is the high prevalence of metabolic syndrome and its components. The major determinants related to this syndrome were advanced age, working history, body mass index, smoking, cholesterol dietary regimen, Framingham risk score, low regular exercising, history of diabetes mellitus, history of gout, and shift work pattern. This issue should be managed by strategic planning to diagnose and control of this syndrome through periodic health assessment to promote the health of professional drivers. Although the results could not be generalized to general population, findings will help promotion of health status and attention of health authorities towards health issues of commercial drivers as a safety sensitive job that can influence communities’ health by prevention of their man-made traffic accidents.
Data availability
The data that support the results are presented in this study.
Author’s contribution
NI, MS were responsible for analysis, visualization, writing of the manuscript; AN made substantial contributions to data acquisition; NI, AN participated in the data interpretation and made substantial revisions in the first draft; MS, AN contributed to the reception and the design of the work. All authors read and approved the final manuscript.
Declaration
Ethical approval
Since it is systematic review, consent to participate does not apply.
Consent for publication
All authors have reviewed the final version of the manuscript and agree with the publication of the article in this journal.
Competing interests
No potential conflicts of interest or funding source were related to this study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nazanin Izadi, Email: nazanin.izadi@gmail.com.
Arezu Najafi, Email: najafeeaz@gmail.com.
Maryam Saraei, Email: saraie_m@yahoo.com.
References
- 1.Lohsoonthorn V, Lertmaharit S, Williams MA. Prevalence of metabolic syndrome among professional and office workers in Bangkok, Thailand. J Med Assoc Thail. 2007;90(9):1908. [PubMed] [Google Scholar]
- 2.McNeill AM, Katz R, Girman CJ, Rosamond WD, Wagenknecht LE, Barzilay JI, et al. Metabolic syndrome and cardiovascular disease in older people: the cardiovascular health study. J Am Geriatr Soc. 2006;54(9):1317–1324. doi: 10.1111/j.1532-5415.2006.00862.x. [DOI] [PubMed] [Google Scholar]
- 3.Cameron AJ, Magliano DJ, Zimmet PZ, Welborn T, Shaw JE. The metabolic syndrome in Australia: prevalence using four definitions. Diabetes Res Clin Pract. 2007;77(3):471–478. doi: 10.1016/j.diabres.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Harzallah F, Alberti H, Ben Khalifa F. The metabolic syndrome in an Arab population: a first look at the new international diabetes federation criteria. Diabet Med 2006;23(4):441–4. [DOI] [PubMed]
- 5.Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med. 2006;23(5):469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 6.Park Y-W, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the third National Health and nutrition examination survey, 1988-1994. Arch Intern Med. 2003;163(4):427–436. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ford ES, Giles WH. A comparison of the prevalence of the metabolic syndrome using two proposed definitions. Diabetes Care. 2003;26(3):575–581. doi: 10.2337/diacare.26.3.575. [DOI] [PubMed] [Google Scholar]
- 8.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and nutrition examination survey. Jama. 2002;287(3):356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 9.Davila EP, Florez H, Fleming LE, Lee DJ, Goodman E, LeBlanc WG, et al. Prevalence of the metabolic syndrome among US workers. Diabetes Care. 2010;33(11):2390–2395. doi: 10.2337/dc10-0681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anand SS, Yusuf S, Jacobs R, Davis AD, Yi Q, Gerstein H, et al. Risk factors, atherosclerosis, and cardiovascular disease among aboriginal people in Canada: the study of health assessment and risk evaluation in aboriginal peoples (SHARE-AP) Lancet. 2001;358(9288):1147–1153. doi: 10.1016/S0140-6736(01)06255-9. [DOI] [PubMed] [Google Scholar]
- 11.Anand SS, Yi Q, Gerstein H, Lonn E, Jacobs R, Vuksan V, et al. Relationship of metabolic syndrome and fibrinolytic dysfunction to cardiovascular disease. Circulation. 2003;108(4):420–425. doi: 10.1161/01.CIR.0000080884.27358.49. [DOI] [PubMed] [Google Scholar]
- 12.Nestel P, Lyu R, Low LP, Sheu WH-H, Nitiyanant W, Saito I, et al. Metabolic syndrome: recent prevalence in East and Southeast Asian populations. Asia Pac J Clin Nutr. 2007;16(2). [PubMed]
- 13.Eapen D, Kalra GL, Merchant N, Arora A, Khan BV. Metabolic syndrome and cardiovascular disease in south Asians. Vasc Health Risk Manag. 2009;5:731. doi: 10.2147/vhrm.s5172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma SK, Ghimire A, Radhakrishnan J, Thapa L, Shrestha NR, Paudel N, et al. Prevalence of hypertension, obesity, diabetes, and metabolic syndrome in Nepal. Int J Hypertens. 2011;2011. [DOI] [PMC free article] [PubMed]
- 15.Nasri H, Moazenzadeh M. Coronary artery disease risk factors in drivers versus people in other occupations. Arya Atheroscler. 2010;2(2).
- 16.Ragland DR, Winkleby MA, Schwalbe J, Holman BL, Morse L, Syme SL, et al. Prevalence of hypertension in bus drivers. Int J Epidemiol. 1987;16(2):208–214. doi: 10.1093/ije/16.2.208. [DOI] [PubMed] [Google Scholar]
- 17.Talbott EO, Gibson LB, Burks A, Engberg R, McHugh KP. Evidence for a dose-response relationship between occupational noise and blood pressure. Arch Environ Health Int J. 1999;54(2):71–78. doi: 10.1080/00039899909602239. [DOI] [PubMed] [Google Scholar]
- 18.Izadi N, Malek M, Aminian O, Saraei M. Medical risk factors of diabetes mellitus among professional drivers. J Diabetes Metab Dis. 2013;12(1):23. doi: 10.1186/2251-6581-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karlsson BH, Knutsson AK, Lindahl BO, Alfredsson LS. Metabolic disturbances in male workers with rotating three-shift work. Results of the WOLF study. Int Arch Occup Environ Health. 2003;76(6):424–430. doi: 10.1007/s00420-003-0440-y. [DOI] [PubMed] [Google Scholar]
- 20.Mohebbi I, Shateri K, Seyedmohammadzad M. The relationship between working schedule patterns and the markers of the metabolic syndrome: comparison of shift workers with day workers. Int J Occup Med Environ Health. 2012;25(4):383–391. doi: 10.2478/s13382-012-0051-5. [DOI] [PubMed] [Google Scholar]
- 21.Ha M, Park J. Shiftwork and metabolic risk factors of cardiovascular disease. J Occup Health. 2005;47(2):89–95. doi: 10.1539/joh.47.89. [DOI] [PubMed] [Google Scholar]
- 22.Ronchese F, Bovenzi M. Occupational risks and health disorders in transport drivers. Giornale italiano di medicina del lavoro ed ergonomia. 2012;34(3):352–359. [PubMed] [Google Scholar]
- 23.Liberati A, Altman D, Tetzlaff J, Mulrow C. Gøtzsche PC, Ioannidis, JPA, … Moher, D. The PRISMA statement for reporting systematic reviews and metaanalyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. [DOI] [PubMed]
- 24.Alberti KGM, Zimmet P, Shaw J. The metabolic syndrome—a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 25.Higgins J, Altman D, Sterne J. Assessing risk of bias in included studies. Cochrane handbook for systematic reviews of interventions. Cochrane Book Ser. 2008:187–241.
- 26.Siu S, Wong K, Lee K, Lo Y, Wong C, Chan A, et al. Prevalence of undiagnosed diabetes mellitus and cardiovascular risk factors in Hong Kong professional drivers. Diabetes Res Clin Pract. 2012;96(1):60–67. doi: 10.1016/j.diabres.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Shin SY, Lee CG, Song HS, Kim SH, Lee HS, Jung MS, et al. Cardiovascular disease risk of bus drivers in a city of Korea. Ann Occup Environ Med. 2013;25(1):34. doi: 10.1186/2052-4374-25-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saberi HR, Moravveji AR, Fakharian E, Dehdashti AR. Prevalence of metabolic syndrome in bus and truck drivers in Kashan, Iran. Diabetol Metab Syndr. 2011;3(1):8. doi: 10.1186/1758-5996-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodríguez-Miranda CD, Jojoa-Ríos JD, Orozco-Acosta LF, Nieto-Cárdenas OA. Síndrome metabólico en conductores de servicio público en Armenia, Colombia. Rev Salud Pública. 2017;19:499–505. doi: 10.15446/rsap.v19n4.69758. [DOI] [PubMed] [Google Scholar]
- 30.Robbins RB, Thiese MS, Ott U, Wood EM, Effiong A, Murtaugh M, et al. Metabolic syndrome in commercial truck drivers: prevalence, associated factors, and comparison with the general population. J Occup Environ Med. 2020;62(7):453–459. doi: 10.1097/JOM.0000000000001863. [DOI] [PubMed] [Google Scholar]
- 31.Montazerifar F, Karajibani M, Pirmoradi B, Torki Z, Moradpour M, Dashipour A. Prevalence of metabolic syndrome in professional drivers. Zahedan J Res Med Sci. 2019;21(3).
- 32.Chen S-C, Chang J-M, Lin M-Y, Hou M-L, Tsai J-C, Hwang S-J, et al. Association of metabolic syndrome and albuminuria with cardiovascular risk in occupational drivers. Int J Mol Sci. 2013;14(11):21997–22010. doi: 10.3390/ijms141121997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lemke MK, Apostolopoulos Y, Hege A, Wideman L, Sönmez S. Work organization, sleep and metabolic syndrome among long-haul truck drivers. Occup Med. 2017;67(4):274–281. doi: 10.1093/occmed/kqx029. [DOI] [PubMed] [Google Scholar]
- 34.Ebrahimi MH, Delvarianzadeh M, Saadat S. Prevalence of metabolic syndrome among Iranian occupational drivers. Diabetes Metab Syndr Clin Res Rev. 2016;10(1):S46–S51. doi: 10.1016/j.dsx.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Appiah CA, Afriyie EO, Hayford FEA, Frimpong E. Prevalence and lifestyle-associated risk factors of metabolic syndrome among commercial motor vehicle drivers in a metropolitan city in Ghana. Pan Afr Med J. 2020;36. [DOI] [PMC free article] [PubMed]
- 36.Cavagioni LC, Bensenor IM, Halpern A, Pierin AM. Metabolic syndrome in professional truck drivers who work on highway BR-116 within the area of São Paulo City-Régis Bittencourt. Arq Bras Endocrinol Metab. 2008;52(6):1015–1023. doi: 10.1590/S0004-27302008000600013. [DOI] [PubMed] [Google Scholar]
- 37.Jahangiry L, Farhangi MA, Rezaei F. Framingham risk score for estimation of 10-years of cardiovascular diseases risk in patients with metabolic syndrome. J Health Popul Nutr. 2017;36(1):1–6. doi: 10.1186/s41043-017-0114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soltaninejad M, Yarmohammadi H, Madrese E, Khaleghi S, Poursadeqiyan M, Aminizadeh M, et al. The prevalence of metabolic syndrome in drivers: A meta-analysis and systematic review. Work. 2020(Preprint):1–7. [DOI] [PubMed]
- 39.Alizade Z, Azadbakht L. Review of epidemiology of metabolic syndrome in Iran. Iran J Diabetes Metab. 2017;15(3):143–157. [Google Scholar]
- 40.Sun M, Feng W, Wang F, Li P, Li Z, Li M, et al. Meta-analysis on shift work and risks of specific obesity types. Obes Rev. 2018;19(1):28–40. doi: 10.1111/obr.12621. [DOI] [PubMed] [Google Scholar]
- 41.Casmir EA, Amam CM, Obianuju BO, Tim PG, David AW, Oyewole AK, et al. Prevalence of cardiometabolic risk factors among professional male long–distance bus drivers in Lagos, south–West Nigeria: a cross–sectional study. Cardiovasc J Afr. 2018;29(2):106. doi: 10.5830/CVJA-2018-006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20(2):1–8. doi: 10.1007/s11906-018-0812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heinonen I, Rinne P, Ruohonen S, Ruohonen S, Ahotupa M, Savontaus E. The effects of equal caloric high fat and western diet on metabolic syndrome, oxidative stress and vascular endothelial function in mice. Acta Physiol. 2014;211(3):515–527. doi: 10.1111/apha.12253. [DOI] [PubMed] [Google Scholar]