Abstract
Off-label use is frequently practiced in primary and revision arthroplasty, as there may be indications for the application of implants for purposes outside the one the manufacturers intended.
Under certain circumstances, patients may benefit from selective application of mix & match. This can refer to primary hip arthroplasty (if evidence suggests that the combination of devices from different manufacturers has superior results) and revision hip or knee arthroplasty (when the exchange of one component only is necessary and the invasiveness of surgery can be reduced).
Within the EFORT ‘Implant and Patient Safety Initiative’, evidence- and consensus-based recommendations have been developed for the safe application of off-label use and mix & match in primary as well as revision hip and knee arthroplasty.
Prior to the application of a medical device for hip or knee arthroplasty off-label and within a mix & match situation, surgeons should balance the risks and benefits to the patient, obtain informed consent, and document the decision process appropriately.
Nevertheless, it is crucial for surgeons to only combine implants that are compatible. Mismatch of components, where their sizes or connections do not fit, may have catastrophic effects and is a surgical mistake.
Surgeons must be fully aware of the features of the components that they use in off-label indications or during mix & match applications, must be appropriately trained and must audit their results.
Considering the frequent practice of off-label and mix & match as well as the potential medico-legal issues, further research is necessary to obtain more data about the appropriate indications and outcomes for those procedures.
Cite this article: EFORT Open Rev 2021;6:982-1005. DOI: 10.1302/2058-5241.6.210080
Keywords: hip arthroplasty, knee arthroplasty, mismatch, mix & match, off-label
Introduction
During this era, when orthopaedic surgeons are being increasingly regulated and litigated against, most will agree that there are occasions when surgeons have to tread carefully between what they think is best for a patient and what is deemed ‘correct’ by regulators and lawyers. For the majority of the time most surgeons will practice evidence-based medicine, but patients are unique and there are times when standard techniques maybe not the best option for a patient. Most surgeons have the capacity to adapt their practice when they think it is necessary and go ‘off-label’. EFORT consider these issues extremely important; they are all about patient safety which is why they commissioned this appraisal in order to evaluate all aspects of these practices and to produce guidance for the benefit of patients, surgeons, manufacturers and regulators.
In this article we will attempt to clarify and suggest recommendations around the issues of off-label, including discussing the mixing and matching of implants from different manufacturers in total joint arthroplasty (‘mix & match’) and commenting on ‘mismatch’. The commentary and conclusions we have made are based on an extensive literature review and consensus meetings. We have reached out to the specialist groups that represent the surgeons who we hope will eventually be guided by our conclusions, and have taken careful note of their opinions.
Definitions and significance
Any discussion about off-label procedures usually includes the subject of litigation, but even in the highest circles it seems that even liability has never been unequivocally defined. For the purposes of this article, we have attempted to define and explain the frequently used descriptions that are used in the context of this subject.
Off-label
Put simply, off-label means that the user of whatever the label has been placed on, is using it in a way that is not listed in the ‘indications for use’ (IFU) that are cited on the label. The United States (US) Food and Drug Administration (FDA) considers off-label use as a utilization of a medical device or drug outside the intended scope of indications or patient group for which they had granted approval.1 In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) offers the advice: ‘You should use medical devices as described by the manufacturer in the instructions. Should you use the device in any other way, it’s considered “off-label” use’.2 Originally, the term off-label was almost exclusively used with respect to pharmaceutical products. In this article, the term will only be used in the context of arthroplasty implants and not in the context of other hardware or procedures (i.e. synthetic implants, allografts, etc.).
Significance
The significance of the term off-label in joint replacement, including in routine surgical practice, is that there are occasions when on-label devices are not readily available or, if available, they do not adequately meet the requirements for a particular patient. Thus, the surgeon turns to a device that they think would fit the requirements, but if the indication for which the surgeons is going to use it for is not in the IFU, it will be said that it has been used off-label. With this decision comes the risk that the implant manufacturer will not take responsibility if the device fails and the responsibility could rest with the surgeon, which could result in major consequences.
Mix & match
According to different dictionaries, a definition of the idiom ‘mix & match’ is to put different things (such as pieces of clothing, furniture or food) together in different ways. In medicine the term is also used when something is made up of complementary elements taken from different sets or sources. Commonly, in contemporary precision medicine initiatives, mixing and matching drugs is an important part of pharmacology in the medical treatment of diseases, but mixing adversely acting drugs is a medication error. In the context of total joint arthroplasty (TJA) in orthopaedic surgery, mix & match describes the use of components from more than one manufacturer in completing the construct.3
Significance
Although off-label use as well as mix & match are frequently practiced in primary and revision arthroplasty, there is an increasing debate about potential medico-legal issues. Therefore, we ask the question: should surgeons, who feel they have no other alternative but to use off-label implants in high-risk patients or to mix and match when results of mixing and matching in a particular situation are equal or superior, be allowed to do so? In other words, should they change their practice simply to protect themselves from possible legal issues or should they continue a practice where their results or available evidence supports that mix & match might be best for their patients?
Certainly, there are agencies, including the medical insurance agencies, competent authorities and manufacturers who argue otherwise. They suggest that if the outcome of a procedure is poor, the surgeon will be blamed for going off-label and litigation might ensue. It has even been said that surgeons could be held responsible for designing a new device if they went off-label, and doubt has been cast over the status of their malpractice insurance. It is suggested that well documented, informed consent from the patient outlining the advantages and drawbacks of such a mix & match procedure would mitigate against litigation.
From Table 1 it is clear that mixing and matching of components in total joint replacement continues to be practiced.
Table 1.
Survey of the incidence of mix & match from contributing members to the International Society of Arthroplasty Registries (ISAR)
| Registry | Past | Present |
|---|---|---|
| AOANJRR (Australia) | Yes | Yes, but less than previously |
| DHR/DKR (Denmark) | Yes | Yes |
| EPRD (Germany) | Yes | 12% Hips |
| KP National Implant Registries (USA) | Yes | 2–4% hips, 1% shoulders |
| FAR (Finland) | Yes | Yes, but less than previously |
| LROI (Netherlands) | Yes | 8% |
| MARCQI (Michigan, USA) | Yes | 1.2% hips |
| NZOA (New Zealand) | Yes | Yes, but less than previously |
| NJR (England and Wales) | Yes (hips, shoulders, patellae) | Yes, but less than previously |
| NAR (Norway) | Yes | > 10 % |
| RIAP (Italy) | 13% hips | 15% hips |
| RIPO (Italy) | Yes | 4 % hips and some patellae |
| SHAR (Sweden) | Yes | Yes |
Source: Performed by Keith Tucker, January 2020.
Malcolm et al4 reported that 30% of total hip arthroplasty (THA) and 37% of total knee arthroplasty (TKA) procedures, using regular off-the-shelf implants, are performed in groups of patients outside those approved by the United States Food and Drug Administration for agreed indications. Due to increasing obesity and other comorbidities, they still expect future growth of these off-label procedures, emphasizing the need for continued medical device surveillance. Peters et al,5 reporting on mix & match, confirmed the practice as being contemporary in many countries, mainly involving THA, but, as demonstrated in Table 1, we found that it has also been reported in total shoulder replacement and in TKA operations where the patella from one manufacturer has been used with the tibial and femoral components of another.
Mismatch
The term ‘mismatch’ generally refers to a situation where components in a construct do not match each other (such as for size or shape) and are altogether unsuitable for each other. In arthroplasty, it is a special subtype of mixing and matching, such as when the size or connections of components do not fit or match each other. A potential mismatch between morphological features of hip or knee bone anatomy and implant configuration is not addressed in this review.
Significance
The significance for the patient and the surgical team is that they have implanted into a patient a construct where the components do not fit or in some way are incompatible. This is very likely to result in early failure of the construct and an early revision operation. Mismatch is generally a mistake.
Methodological approach
Inauguration workshop
An inauguration workshop of the EFORT Implant and Patient Safety Initiative (IPSI) took place on 21 January 2020 with the participation of a steering group invited by the EFORT board. The steering group consisted of clinical experts, scientists, representatives from implant manufacturers, regulatory authorities and patient organizations. Also attending were representatives from European national societies and specialty societies, who were identified before the initiative commenced. During the workshop, the convenors (KT, LZ) introduced the scoping process and defined clinically relevant key questions about off-label use and mix & match with the participants within the workshop. It was agreed that the target audience for these recommendations will be primarily European orthopaedic surgeons.
After this initial meeting, the clinical key questions have been translated into epidemiological topics by the convenors, a methodologist (TL) and members of the writing group (KT, LZ, PKA, KPG, JL, JPK, RGHHN). These key topics formed the basis for the search and synthesis of evidence which was used to develop an iterative consensus process to be used by clinical experts. The clinical recommendations have therefore been based on all the available evidence and clinical expertise. The sequential development steps of the practical recommendation are described in more detail in the following chapters.
Evidence retrieval and synthesis
In order to identify the best available evidence for the clinical topics, a systematic literature search was performed. Based on the information provided from the inauguration workshop, the convenors and members of the writing group defined relevant terms for the systematic literature search, which was then performed by the methodologist. Two in-depth literature searches were performed:
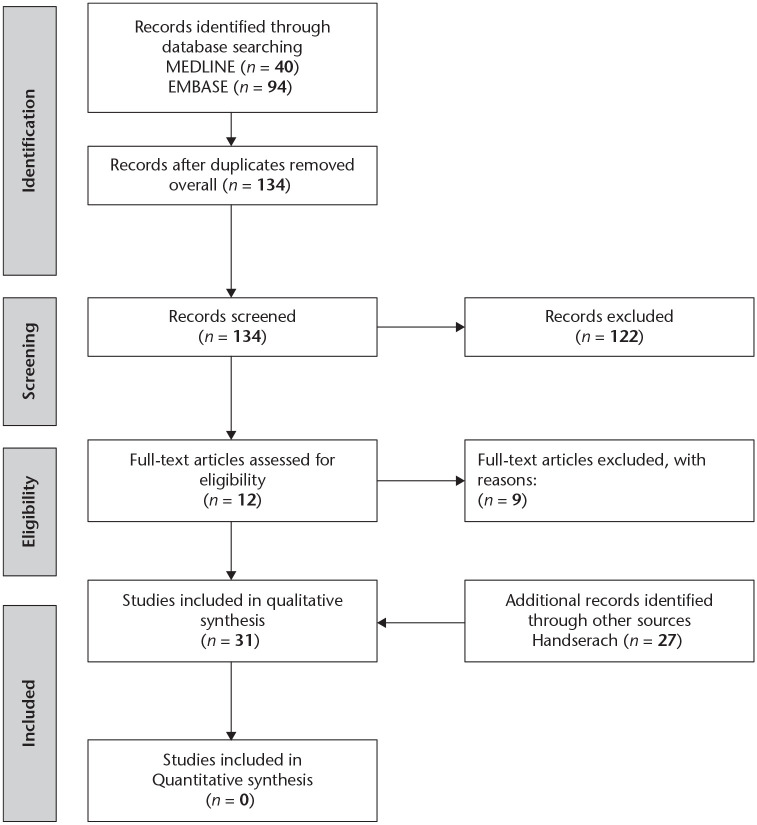
(1) to identify available evidence for off-label use of regular implants during THA/TKA (Fig. 1),
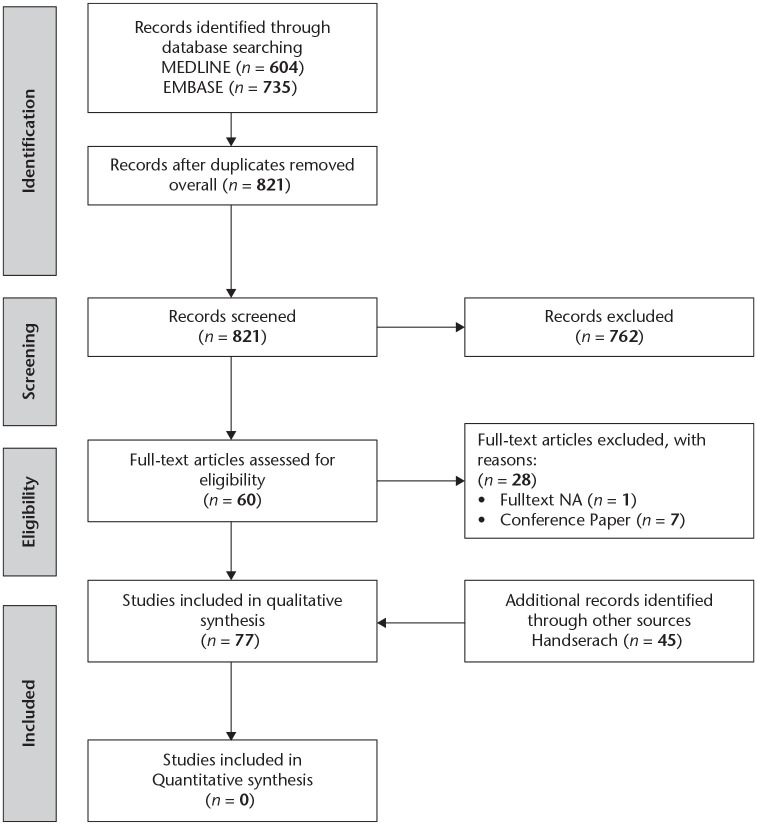
(2) to identify publications concerning the mixing of implants from different manufacturers for primary and revision THA/TKA (Fig. 2).
Fig. 1.
Flowchart of evidence retrieval about ‘off-label’ use.
Fig. 2.
Flowchart of evidence retrieval about ‘mix & match’.
Both literature searches were performed in EMBASE via Ovid and MEDLINE via PubMed. The titles and abstracts were screened independently in a double-blind manner by two reviewers (clinical experts) for eligibility. The search was completed by a hand search of abstracts additionally referring to the above topics. All eligible full texts were screened by at least two reviewers and allocated to the clinical topics.
Based on the results of the systematic literature searches, the convenors and writing group members drafted a first set of recommendations for the clinically relevant topics, which served as the basis for next steps in the consensus process. For each resulting recommendation, the available evidence was summarized.
Consultation of steering group, national and specialty societies
In order to receive additional input from clinical experts, the writing group distributed the preliminary set of recommendations and background information to the steering group as well as to EFORT National Member Societies and Specialty Societies (National Delegates and Presidents of Specialty Societies). They received a copy of the preliminary recommendations together with the summarized evidence and were asked for comments, specifically with regard to the relevance and completeness of the recommendations. Furthermore, the national society representatives were asked to compare ‘our’ guidelines with their own national guidelines to demonstrate any shortcomings or discrepancies.
A total of 26 steering group members, 70 national delegates and three specialty societies representatives were contacted and we received 40 responses (40%).
Consensus voting
Convenors and writing group members integrated the comments from the steering group and the national and specialty society representatives into the draft of preliminary recommendations. After confirming any possibility of potential plagiarism could not have occurred, updating references and correcting the English, the document was resent to all members of the steering group and the national and specialty society representatives to prepare consensus voting.
Prior to the annual EFORT congress, a final meeting of the steering group was organized on 23 June 2021 in Dresden. The convenors presented the results of the set of recommendations with the underlying evidence to all 30 panel members who could participate.
Due to the restrictions imposed by the COVID-19 pandemic only three steering group members attended the meeting in person whilst the other 27 panellists participated online. After explanation of the voting rules and voting process, consensus voting was performed. Due to the lack of a generally accepted definition of consensus in the development of recommendations, we adopted the stepwise approach as implemented during the previous consensus initiative on periprosthetic joint infections.6 The following levels of consensus have been established:
No consensus: less than 60% agreement in the voting panel
Weak consensus: 60% to 65% agreement
Consensus: 66% to 74% agreement
Strong consensus: 75% or more agreement
Unanimous: 100% agreement
During the voting process, all recommendations were displayed on a screen and the delegates were asked to vote in real time. Where necessary, the recommendations were rephrased and re-voted on. There were three possible responses to each recommendation: agree, disagree, or abstain. The voting results were communicated to the panellists electronically immediately after each vote was taken.
Distribution of the consensus document
Immediately after the consensus meeting, the voting results were added to the final recommendation document and the manuscript submitted for publication. When the recommendations are finally published, they will be sent to national societies as well as specialty societies who will be encouraged to distribute them to their members. In addition, the recommendations will be published on the EFORT and on individual member societies’ websites.
Recommendations
Off-label use of THA and TKA implants outside the scope of approved indications
Recommendation 1: There may be indications for the application of THA or TKA implants for purposes outside the one for which the manufacturer intended both in primary and revision arthroplasty (off-label use).
Results of consensus voting: 100% agreement, 0% disagreement, 0% abstention
Off-label use of implants and surgical instruments refers to their use outside those listed in the manufacturer’s ‘instruction for use’ or IFU. This section addresses the use of implants in conditions for which they were not originally intended (mix & match will be dealt with in a separate section).
Off-label use of instruments, and particularly implants, has been practiced for years. The original indications for THA as well as TKA were mainly aimed at the elderly and the infirm with crippling arthritis but with limited comorbidities. With the significant improvement in outcomes due to improved implant design, fixation techniques, surgical approaches, and postoperative rehabilitation total joint arthroplasty (TJA) is now offered to young and active patients as well as patients with different comorbidities and disease patterns.4 It is a seminal point that such procedures, once considered ‘off-label’, are nowadays routinely accepted.7
However, in spite of it being acceptable to offer TJA in the way that is now practiced, implant labelling has largely remained unchanged, typically reflecting historic indications and contraindications. Some manufacturers still only list in their IFU primary and secondary osteoarthritis in skeletally mature individuals as a result of non-inflammatory degenerative joint disease as the indication for use. They then go on to include disorders predisposing to infection and implant loosening (i.e. obesity, metabolic disorders, osteoporosis) besides non-compliance and inadequate fixation as contraindications.
Malcolm et al4 calculated a national off-label prevalence of 30.4% and 37.0% for THA and TKA, respectively in their United States Healthcare Cost and Utilization Project. They attributed the slight predilection for off-label practice in TKA compared to THA to higher rates of obesity (15.3% vs. 9.8%) and metabolic/bone disease (23.7% vs. 19.4%). It was also reported that with increased incidence of comorbidities the off-label rate rose annually for each procedure type during the investigated decade. Liu et al,8 in a single-institution study, evaluated the incidence and outcomes between patients with implants used on- and off-label. They found that, by current definition, of the 225 patients surveyed (92 hips and 133 knees), 154 patients (68.4%) had off-label implants. No differences in outcomes were reported in the off-label group.
There are reports, albeit few, where a surgeon has deliberately gone a bit more than just off-label. Marie-Hardy et al9 reported two cases (a unicompartmental knee arthroplasty and a TKA) where very abnormal patient anatomy meant that using an implant designed for the contralateral side provide the patient with a better fit.
It is germane to the argument, as pointed out by Nunley et al,10 that the indication of off-label implants for patients may depend on whether or not the indication has been approved in a specific country or by a particular health authority. This inconsistency can also apply to their use in different anatomical situations.11 Taylor et al12 commented in their article on the ‘off-label use in orthopaedic surgery’, that surgeons frequently use orthopaedic devices in an off-label manner. They added that it is the responsibility of the surgeon to be familiar with the product and to base its use on scientific and clinical rationale. Such practices are poorly publicized, and there remains a paucity of literature surrounding the off-label use of orthopaedic devices. These authors have supported the argument made by surgeons that they should be able to implant off-label within the scope of their medical practice if by doing so they optimize a patient’s outcome. They must, however, be fully cognisant of the recognized indications and any relevant research and clinical experience that is available. Zindrick13 pointed out that, whilst everyone expects an increasing number of innovations and technological improvements in orthopaedics, ethical and moral issues are raised whenever there is a suggestion that a device is being used in an off-label fashion. The commentary emphasized that the moral physician will always place a patient’s well-being and best interests above all else. It would appear that all these authors are asking for improved clarity throughout the whole issue of off-label.
Summary
Off-label use of instruments and implants has been common clinical practice in arthroplasty for many years, as current IFU restrictions are often based on historic indications and contraindications, but also should be justified by clinical data, to fulfil the regulatory requirements.
Surgeons must be familiar with the product, and it is their responsibility to base its use on scientific and clinical rationale.
Recommendation 2: Prior to the application of a medical device for hip or knee arthroplasty off-label, surgeons should balance the risks and benefits to the patient, obtain informed consent, and document the decision process appropriately.
Results of consensus voting: 100% agreement, 0% disagreement, 0% abstention
In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA)2 recommend that surgeons should use medical devices as described by the manufacturer in the IFU. If the device is used in any other way, the MHRA consider it to be used off-label. Their statement goes on to say that without the manufacturer’s approval, using a device off-label will mean that any risk will become the surgeon’s liability. Also in their advice, they state that the surgeon or their employer could become liable for civil claims for damages from injured patients or their families if the device should fail. The MHRA cites a list of reasons as to why they consider off-label use to be a risk which includes adverse reactions, inadequate sterilization, insufficient mechanical strength and/or structural integrity, insufficient durability besides misuse due to lack of adequate training for the device. However, they do go on to say, in their advice to surgeons, that in the rare situation where there is no medical device available for a procedure, the surgeon may decide:
to use an existing medical device normally designed for a different purpose;
to modify a medical device for a new purpose;
or to use a product for a medical purpose that is not CE (Conformité Européene – certificate) marked as a medical device.
However, they stress that surgeons must balance the risks and benefits to the patient, taking account of the MHRA recommendations,2 which include:
Carrying out a risk assessment and documenting it.
Considering the ethical and legal implications.
Implementing suitable precautions to minimize the risk.
Reviewing the risk assessment at suitable periods.
Getting approval from the MHRA for exceptional use of non-complying devices (if necessary).
Informing the patient during the consent procedure and documenting off-label use.
What is also said is that off-label use is legal as long as it is in accordance with the medical standard of care; care that is reflective of the type of care that a reasonable physician would provide under similar circumstances. Practically, this care translates to the use of the device in a way that serves patient needs in an equivalent or better manner than other currently available options.12
The point is also made that if the off-label use is not a common feature of practice, or empirical evidence does not exist supporting its use in a particular setting, the surgeon may have difficulty in providing the necessary evidence. Given this case law, it would be in the best interest of the surgeon to disclose off-label use to all patients and to ensure that, wherever possible, any off-label use is performed in accordance with common practice and the available scientific evidence. This will involve counselling patients appropriately regarding risks, benefits, and alternatives to any proposed treatment with appropriate records being documented and the physician’s records including a note about any off-label usage. The records should include any information regarding the relevant off-label usage.12–14 It is readily acknowledged that today’s patient may well expect to become a partner with the physician and to participate in the treatment decision making. This participation will include making personal decisions based on the full disclosure of risks, benefits, and alternatives besides the physician’s personal experience with various treatments.
Whilst a new device may not be off-label as it has a CE mark, it might just as well be for a particular surgeon who has not previously used it. Not infrequently, patients are biased towards new but unproven devices, believing that in medicine new must equate with better.12 Indeed, any dialogue with a patient that touches on a new device should embrace caution. Anand et al15 failed to show that there was any benefit to patients from the introduction of new prostheses, details of which had been recorded in the Australian registry during the previous five-year study period. They identified new implants with worse outcomes than the ones which were well established.
It is agreed that physicians, after a full and frank discussion with the patient, will usually recommend the treatment they think is the best for a particular patient. They will try not to introduce any personal bias but a patient’s choice is nearly always influenced by the recommendation made by the physician whom they trust and respect.13 For a standard procedure the consent process is relatively straightforward, but where there are off-label implants or techniques involved, the discussion may be more challenging; it will be incumbent on the surgeon to be sure as possible that informed consent has been achieved. The surgeon will have to question whether the patient fully understands the lack of existing medical information regarding outcomes and long-term effects of any off-label procedure. Surgeons must be very clear in their minds that they have imparted their guidance to the patient thoroughly, accurately and honestly so as to allow the patient to come to logical decision about what will be in their best interest.13,16
Summary
In situations where there is no IFU-approved implant available, surgeons must balance the risks and benefits to the patient before considering an off-label procedure.
Prior to the operation the patient should be informed about the advantages and disadvantages of off-label use, in order to allow proper shared decision making. It is, however, recognized that during an operation, when the patient is anaesthetized, the final decision making will have to be left to the surgeon who will be cognisant of the patients’ preoperative thoughts and views.
Appropriate documentation of decision making and off-label use is mandatory. It is important that the indication for undertaking a procedure involving off-label devices should be fully justified and documented.
The documentation should include a benefit-risk assessment, which could be performed according to published guidelines of the European Commission’s independent Scientific Committee on Health, Environmental and Emerging Risks (SCHEER).
Primary THA and TKA
Recommendation 3: In obese patients, primary and revision arthroplasty is associated with increased peri and postoperative risks. Off-label use of implants must be considered carefully by surgeons and patients.
Results of consensus voting: 100% agreement, 0% disagreement, 0% abstention
According to the manufacturers, the IFUs many of their THRs and TKRs are either contraindicated or at least not recommended in obese patients. A fact that is not widely appreciated. Craik et al17 reviewed the most commonly used primary THA and TKA components in the National Joint Registry (NJR) and requested their IFUs from the manufacturers with regard to recommendations for component use in obesity. Of 25 components reviewed:
Five recommended against implant use in obese patients or even listed obesity as a contraindication.
Four reported morbid or pathological obesity as a contraindication.
Of the remaining implants, all advised caution or patient counselling with regard to the risks of implant use in heavy, overweight or obese patients.
Based on this information and the analysis of all patients with a body mass index (BMI) of more than 30 kg/m2 in the NJR database, a total of 10,745 patients (16%) received implants against manufacturer recommendations.
It is well recognized and well recorded that obesity is influencing the rate of peri- and postoperative complications in THA and TKA arthroplasty. There are several meta-analyses, including those by Kunutsor et al18 and reviews by Liu et al,19–21 Ponnusamy et al,22 Boyce et al,23 Chaudhry et al,24 and Sun and Li.25 They all reported that obesity results in increased rates of infections and revisions secondary to deep infection besides an increase in overall complications. Especially patients with morbid obesity (BMI > 40 kg/m2), and those with super-obesity (BMI > 50 kg/m2) seem to have substantially higher risks of all-cause and septic revision.22,24 Barrett et al26 reported an increased rate of thromboembolic events in obese TKA and THA patients whilst Liu et al19 observed a higher frequency of dislocation in THA in obese patients.
At the Second International Consensus Meeting on Musculoskeletal Infection27 a clear association between obesity and PJI was agreed upon. The authors of the output considered that obesity is a modifiable risk factor and recommended that arthroplasty should be delayed until body weight has been reduced. It was agreed that obesity is considered a relative contraindication while super-obesity (BMI ⩾ 50 kg/m2) serves as an absolute contraindication.28
Nevertheless, despite the overall increased complication rate in obese THA and TKA patients, patient-relevant outcome improvements (PROMS) are often comparable to those for non-obese patients.19,21 What this means is that although obese patients rarely achieve the high outcome scores that many non-obese reach in terms of function, as they usually start a lower level preoperatively, their overall gain is often comparable to that of non-obese patients.23
Should arthroplasty be withheld in obese patients?
As improvement of functional outcomes and satisfaction are little different in obese patients, it can be argued that it is unfair to withhold arthroplasty. Considering the high and even increasing number of obese patients worldwide, it is very important that everyone involved acknowledges the potential risks of elevated body weight. It will always have to be part of the discussion during the shared decision-making process with a patient, including advice about weight loss. However, it is noted that any approach to reducing weight is controversial28 and weight loss may not always result in adequate risk reduction.27,29
Which implants should a surgeon use in obese patients?
If a surgeon’s standard implant is contraindicated or not recommended in obese patients, the surgeon has to choose the most appropriate implant for the patient. This can either be the use of this standard implant off-label or to use another implant. It has to be acknowledged, however, that for surgeons using an implant which they rarely use, just because it is not contraindicated in an obese patient, it will also have attendant risks. Withholding commonly used implants with good results in registries to obese patients, in favour of implants which are less commonly used, may result in even higher revision risk in obese patients. It could also skew registry data.
It is important that surgeons are cognisant of any contraindications to use in the IFU and their legal responsibilities, whilst coming to a decision about the implant they use. The reasons for their final decision must be well documented.
Revision arthroplasty
Corresponding to the age-related increase that has been seen worldwide in the rates of primary THA and TKA rates, is a corresponding increase in the number of revisions arthroplasties being undertaken and further growth has to be expected. Considering the fact that revision patients show a similar trend towards rising BMI as primary patients, it is of concern that, again, many implant manufacturers include obesity as a relative or even absolute contraindication in their revision implant IFU.30
As with primary TJA, all complications including infection in revision arthroplasty are reported as being higher in obese patients. A large national database31 analysing both 18,866 THA and THA revisions and systematic reviews of reasons for failure after hip revision32 and knee revision30 demonstrated that obese patients – and especially those with morbid obesity – have higher complication and re-revision rates than non-obese patients.
While the reported main problem in these large cohorts is again periprosthetic infection, potential mechanical failure is rarely mentioned in this advancing field. However, reports do exist, especially in modular hip revisions stems, that elevated mechanical load on the components can lead to fracture of the taper connection. Other causes of mechanical failure (i.e. high offset, short proximal component, lack of adequate medial bone supporting the junction area) seem to be more common in the obese patient.33–36 Whilst one option to avoid taper connection fractures is to use a monobloc or non-modular implant, there is always a conflict when obesity is listed as a contraindication in the IFU.
Thus, considering the increased risk of complications in obese patients who have to undergo revision surgery, it is important that they are advised about potential off-label use in order to avoid litigation.30
Summary
Considering the increasing prevalence of obesity and a rising number of patients with primary as well as revision THA and TKA, there are several points which need to be urgently addressed:
Firstly, denying TJA in obese patients, where conservative treatment has failed and weight loss is not a viable option is, in most people’s view, inhumane.
The suggestion that the surgeon takes responsibility for implanting a device ‘off-label’ and is maybe legally responsible for potentially resulting problems is unreasonable and should be put aside.
The current product information and IFU of manufacturers should be re-appraised in the light of contemporary practice and, where appropriate, revised.
Surgeons should be familiar with the IFU.
Shared decision making is of even more importance in these complex patients.
Implant manufacturers are strongly encouraged to base their warnings and contraindications about obesity on biomechanical data and to clearly describe these restrictions in the IFU.
Mix & match in primary hip arthroplasty
Recommendation 4: Due to product liability it is commonly accepted in primary THA to use all components from one manufacturer. If evidence suggests, however, that the combination of devices from different manufacturers has superior results, patients may benefit from selective and documented application of mixing and matching.
Results of consensus voting: 96.15% agreement, 3.85% disagreement, 0% abstention
For many years, throughout the world, a good number of surgeons have made a positive decision to use components from more than one manufacturer, in the formation of a joint replacement, both in the primary and revision setting. The practice is widely documented as mix & match. The practice mainly involves hips but has also involved total shoulder and knee arthroplasty.
The construct that is created has the manufacturers mixed and the sizes matched, but is this practice safe and what is the evidence both from a bioengineering and a clinical perspective? It has been hypothesized that in THA the combination of different implants from different manufacturers can lead to adverse effects.37–40
A typical example of mix & match would be combining an acetabular cup and liner from one company with a stem and head from another. The majority of recorded instances has involved polythene (of varying types) being mixed with ceramic or metal heads. In this section an attempt is made to address these issues.
Bio-engineering commentary
Acetabular bearing wear and friction depend on the combined materials and sizes. The head and socket diameters are slightly different, and from this difference the bearing clearance is defined. In particular with hard-on-hard bearings the clearance is an important parameter to promote mixed lubrication or fluid-film lubrication, ensuring low wear and friction.41 By combining components from different manufactures, the mode of lubrication might be altered, potentially leading to increased wear or pinching of the bearing. With hard-on-soft bearings the influence of the clearance is not as strong, as these bearing are generally not as sensitive regarding the mode of lubrication and furthermore the size of the polyethylene liner is requested by standardization (ISO 7206-2) to be slightly larger than the nominal bearing size. Consequently, pinching of the bearing is not expected even if a head and a polyethylene liner from different manufactures are combined.
There is probably more concern with regard to tapers. Femoral heads are connected to the stem by a taper connection. The male taper or trunnion is the proximal part of the stem that is engineered to fit perfectly into the female taper on the underside of the femoral head (ball). This arrangement secures the head onto the stem. It is important to realize that modular tapers are not standardized and that they vary in terms of dimension and surface properties albeit they (i.e. the 12/14 taper) may be labelled the same.42,43
As they can vary from manufacturer to manufacturer, it is agreed that combining a stem and head from different manufacturers should not be undertaken. Good evidence behind this advice came from Mueller et al,43 who performed torque-off tests using hip stems and metal femoral heads from different implant manufacturers. They showed that while some mix & match combinations from two different manufacturers failed to indicate a potential problem when compared with the off-the-shelf combination, the overall results suggested that mixing components may affect the strength of the taper connection. They suggested that this could lead to increased weakness and a reduction in the stability of the construct.
From systematic reviews four modularity-related taper failure modes have been identified:
Tribocorrosion-associated adverse local tissue reactions (ALTR)
Dissociation of a taper junction
Stem fracture
Mismatch of a femoral head taper attached to a stem with a different trunnion size44,45
Angular mismatch at the taper junction has been shown to lead to increased micromotion above certain thresholds.46 This may cause severe fretting and corrosion with loss of material from the bore of the head as well as from the trunnion)47–49 leading to dissociation of the coupling. Particle release can also induce adverse biologic reactions.50
In THAs with ceramic heads, a mismatch can result in a fracture of the femoral head component.48,51,52
Other studies have reported different results. Cook et al53 analysed the geometry of taper interfaces from different manufacturers in order to establish whether the taper clearance angles were outside the normal range for other taper interfaces. Also reviewed were the rates of material loss from the bearings and taper. They ranked the stem damage to determine whether the levels of loss were above that seen for other similar joints. The material loss analysis demonstrated that the rates or levels of loss from the bearings, taper and trunnion were no different to levels published for manufacturer matched joints and in many cases were lower. They also demonstrated that the taper clearance angles for the mixed manufacturer joints were within the range of other studies and manufacturer matched clearances. Thus, when compared to same manufacturer pairings, using components from different manufacturers failed to show increased material loss. These findings are in line with a recent investigation of retrieved hips with large-diameter cobalt-chromium heads, where those paired with stems from different manufacturers (mix & match) did not show higher corrosion scores than those paired with stems from the same manufacturer.54
In summarizing the data, it is very evident that at the taper junction there are significant variations in shape, metallurgy, roughness, inclination, and angle.43,55 Taking this evidence into account would lead us to recommend that surgeons should avoid mixing stem–head combinations which are not authorized by manufacturers. The risks include trunnionosis and, in the case of an unpaired ceramic head, ceramic head fracture.
Clinical commentary
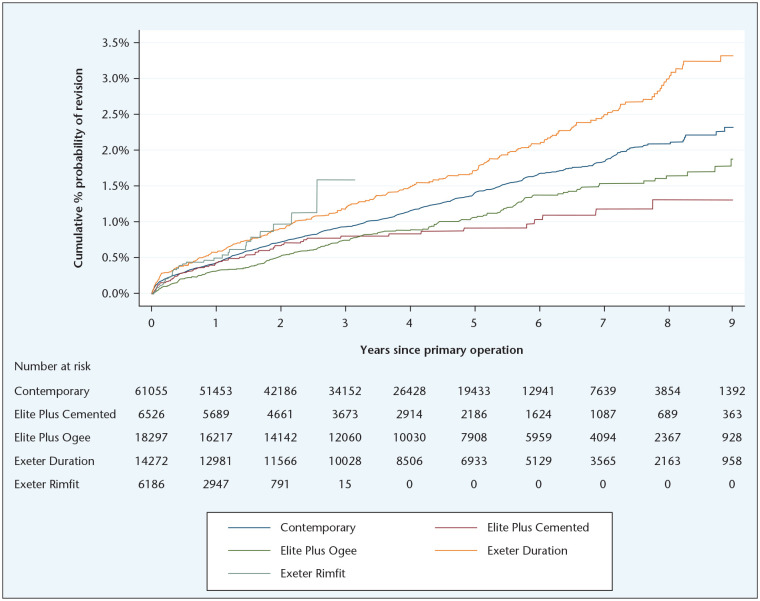
It is extremely relevant to this discussion that some authors have shown that in some circumstances mix & match can result in lower revision rates in hip replacement than from non-mixed THAs.5,56,57 In fact, mix & match THA has been practiced on a large scale (Fig. 3). Typically, in THA, the practice involves the use of cups and liners from one manufacturer with stems and heads from another. More recently, combining the stem from one manufacturer with a dual mobility cup from another has become commonplace in patients with a high risk of instability.58
Fig. 3.
Graphs to show the probability of revision when an Exeter V40 femoral component is used with different brands of acetabular components both the Elite acetabular cups, which are made by a company other than the company which manufactured the Exeter V40 stem, show lower revision rates than non-mixed combinations.
Source: The illustration is by courtesy of the National Joint Registry, reproduced with kind permission.
Tucker et al57 reported data from the National Joint Registry of England and Wales (NJR) describing the incidence of mix & match in THA. They produced data showing that, in the NJR, mix & match had been recorded for virtually all combinations of implants used in THA, and in a few cases how more than two manufacturers’ implants had been used in a single construct. They divided the constructs into ‘hard-on-soft’ and ‘hard-on-hard’. The former included metal or ceramic heads on polythene and the latter ‘metal-on-metal’ or ‘ceramic-on-ceramic’. The best performing construct in the NJR at the time of publishing was a cemented Exeter Stem and the Charnley Elite cup that are produced by different manufacturers. The breakdown when the data was sampled is below in Table 2.
Table 2.
Breakdown of the bearing combinations in the National Joint Registry (NJR) from 2003–2013
| Matched | Mix & match | ||
|---|---|---|---|
| Hard-on-soft | Monobloc or modular stem metal head on monobloc poly cup modular cup with poly liner | 519,993 | 79,672 approx. (13.3%) |
| Ceramic head on poly cup | 27,909 | 7,894 approx. (22.0%) | |
| Hard-on-hard | Ceramic-on-ceramic | 83,295 | 3,861 approx. (4.4%) |
| Metal-on-metal (include. standard head size & resurfacing) | 29,206 | 4,138 approx. (12.4%) | |
| Approximate totals (some data were not ‘clean’ enough to use) | 660,403 87.4% |
95,565
(12.6 %) |
|
Source: Courtesy of Keith Tucker.
Other important outcomes detailed in the article
The results of mixing and matching large and regular sized metal heads and acetabular components in a construct appeared to be no worse than the results from most of the control group where no mix & match had occurred. In fact, if the results from the ASR© are extracted the results in the mix & match group were better than in the control group. It was emphasized that all the results from metal-on-metal were dismal.
The results of mixing and matching ceramic constructs failed to show any meaningful difference from the control group (it should be understood that the vast majority were manufactured by the same company).
The results of mixing and matching metal heads on a metal stem in a construct with a high-density polyethylene cup showed the mix & match results to be inferior to the controls, although the numbers were small.
Other national registries have published similar findings. Peters et al5 reported from the LROI (Netherlands) that during an eight-year period between 2007 and 2014 mix & match had occurred in 11% of primary THAs. They reported that the revision rates in the mix & match group were similar to the non-mix & match cohort. Taylor et al56 in their analysis of New Zealand Joint Registry data (99,732 arthroplasties performed between 1999 and 2015), reported that in 24.6% of hip procedures mix & match was recorded in the registry. Their survival analysis showed that the 17-year results for matched components and unmatched were within 95% confidence intervals of each other at all time points. Interestingly, there was a small, statistically significant improvement in Oxford Hip Scores for the unmatched group compared with the matched group. They concluded that it is safe to use unmatched implants for THA as the outcomes in the groups they evaluated compared favourably with those of matched implants in the medium to long term. In addition to these observations from arthroplasty registries, Trebše et al59 reported that mixing components from different manufacturers did not lead to worse survival rates if the head and stem were provided from the same manufacturer.
Finally, a pertinent fact is that manufacturers are prepared to sell one component of a joint replacement in large numbers to a specific hospital without questioning why the purchaser has not included the rest of the construct in the purchase. Manufacturers are obviously aware of mix & match and it could be argued that they would have a moral responsibility to advise a surgeon against the practice if they had evidence that it was dangerous.
Summary
It would seem that there are pros and cons to mixing and matching components from more than one manufacturer in a THA.
The evidence suggests that reliable results in mix & match are only likely to be achieved when it is limited to combining cups and inserts from one manufacturer with stems and heads from another.
Ceramics and metals from different manufacturers should never be mixed as materials coming from different fabricators may differ in their mixture.
Careful thoughts based on available long-term results should be applied to any situation where mixing and matching head and stem is being considered.
If a THA failed and it was one where the manufacturer of the acetabular component(s) was different from the one who manufactured the femoral components it is very unlikely that mix & match was responsible for the failure.
If a manufacturer only produces an acetabular component, using a femoral system from another is not unreasonable (e.g. dual mobility constructs, constrained liners).
Informed consent is important.
Mixing and matching in revision surgery
Recommendation 5: When, in revision THA and TKA, only one component needs revising, mix & match should be allowed. Taking the patient’s risk-benefit balance, the available evidence and the current state of the art into account, surgeons should be allowed to avoid replacing a component purely to avoid mix & match.
Results of consensus voting: 100% agreement, 0% disagreement, 0% abstention
Somewhat surprisingly, in view of the importance that the regulators and manufacturers have attached to the dangers of mixing and matching in primary operations, the practice of mix & match in the revision setting seems never to have been challenged. The following clinical situations, where this practice has been undertaken, include:
when an exact replacement of the failed prosthesis is not immediately available or no longer manufactured (legacy implants).
when a different design or surface finishing of an implant is required such as a long-stem prosthesis or a high porosity cup or cage or complex reconstruction and either the manufacturer does not make such a device or it would not be immediately available.
after consideration of the patient’s fitness to withstand the extended surgery required to remove a well-fixed implant.
In these often-challenging cases the following examples of strategies have been shown to be effective, often using mix & match 60.
Application of a taper adapter for exchange of ceramic heads
In a case of acetabular revision surgery, where the stem is well fixed and the taper undamaged, the surgeon has the option of using a taper adapter or a re-sleeving device so they can use a new femoral head that pairs with the revision acetabular component they have used. The importance of this option cannot be over stressed. It will reduce operating time, reduce blood loss and preserve bone stock. It does have to be noted that while a new metal ball can be applied to a well-fixed stem without gross taper damage, ceramic manufacturers have concerns over placing a ceramic head on a used trunnion, due to the danger of ceramic fracture. These adaptors, which are usually made of titanium alloy, are designed to be placed over the trunnion of the retained stem. They allow for neck length adjustment and they negate the risks of ceramic fracture when ceramic heads are applied to a ‘used’ trunnion. By definition they are examples of mix & match if they are manufactured by another company.61
Some manufacturers also provide special ceramic heads for THA revision surgery, where the titanium sleeve is integrated into the ceramic head62 and several studies have demonstrated good results when this technology is used.63–68
All those combinations can be used when the taper of the head/adapter is the same as the taper of the in situ stem and if the maximum manufacturer-approved stem extension is not exceeded. This has to be verified intraoperatively.
When these devices are off-label, where possible, surgeons should explain the rationale behind their use and record the patient’s informed consent.
Cementing a polyethylene liner into a well-fixed acetabular component
If removing the well-fixed metal back component of a modular acetabular component is thought to be contraindicated, cementing a new liner into the shell is an accepted procedure.69,70 This option is particularly applicable when either a replica of the original liner is not available (either off-the-shelf or custom made) or when the locking mechanism is damaged.71 The shell size has to be adequate to accept a liner with a > 2 mm cement mantle around it and the operative technique does have to include scoring the inside of the metal shell in a spider web configuration to a depth of 1 mm to promote reliable bonding.72
Bensen et al 73 have shown sufficient mechanical stability of cemented liners in an in vitro investigation, and several clinical studies report good intermediate to long-term results, although the dislocation rate has been reported to be as high as 17%.62,71,74 It has been suggested that the use of constrained liners may be an alternative to provide better stability.75,76 However, it is likely that the liner dissociation rate would be increased due to the decreased impingement-free arc of motion, resulting in higher stress at the cement–implant interface.
When cementing a conventional or constrained liner into the shell, the technique must be definitely regarded as off-label. Not only is it off-label, if the manufacturer of the new (cemented) liner is different from the manufacturer of the shell it should be regarded as mix & match. The surgeon must be cognisant of the technical recommendations (i.e. cement mantle thickness, appropriate scoring). Thus, appropriate patient counselling will be essential.
Cementing dual mobility liners into well fixed acetabular components
In view of the high frequency of dislocations when polyethylene liners are cemented into well fixed metal back components during acetabular revision, a recently recommended alternative is cementing dual mobility cups into the retained liner (‘double-socket’ technique). Both primary and revision THA tripolar cups have been shown to have low dislocation rates and they can be readily cemented into well fixed shells as an off-label technique. Biomechanical investigations have confirmed reliable fixation of the constructs, when they are exposed to significantly higher maximum lever arm moments than those used to test all-polyethylene components.77,78 Again, a prerequisite for success is a minimum cement mantle thickness of 2–3 mm and spider roughening of the metal shell surface. Encouraging short- to medium-term results have been reported using this technique.79–84 Long-term results are awaited, but the technique seems to be useful in cases with high risk of instability and it allows a more limited exposure and surgical trauma during revision. Nevertheless, as an off-label procedure, patients must be informed appropriately.
Waiving exchange of a well seated patellar component in aseptic TKA revision
If the femoro-tibial components of a previously implanted tri-compartmental TKA have to be replaced by a new implant, with different design or from a different manufacturer, and the patella is well integrated without evidence of polyethylene wear, it might be detrimental for the bone stock to revise it just to match the new revision device. Shield et al85 have presented a large series of aseptic revisions where femoral and/or tibial components were exchanged and the patella was not. The clinical results at medium-term follow-up were good, and no reoperations on any patella or risk of failure were observed.
Other applications
Dual mobility acetabular components on conventional stems have been reported as producing encouraging results after excision of the femoral head in revisions of surface replacements, where the acetabular component is being retained.86,87 Long-term reports are not yet available and it could be that there will be a potential wear problem as a consequence of incompatible clearance.88
In selected circumstances, particularly when more than one risk factor is present, (such as instability, allergy to metals, ceramic breakage) off-label use of modular ceramic dual mobility liners has been incorporated into the THA.89
In order to treat large acetabular defects in hip revision, several authors recommend the use of a modular reconstruction construct incorporating anti-protrusio cages and metal augments. If components from different manufacturers are used or two off-the-shelf components from one manufacturer are combined (without being formally approved for use together) the procedure is performed off-label.15,90
Occasionally it may be deemed necessary to reshape peripheral areas of a polyethylene bearing in a TKA for impingement as described by Shah et al.91 They described how they reshaped the posterior aspect of a large size constrained liner to fit into the corresponding femoral box of a retained femoral component, during a revision for recurrent posterior knee dislocation after TKA.
Considering the fact that THA and TKA revision surgery can be very complex, every effort should be made to reduce the morbidity of the procedure. This is particularly important in these patients who are often elderly and suffering from other comorbidities. The use of reliable technical or implant modifications that make an operation quicker and less traumatic should be supported.
Summary
At present the evidence for the use of these off-label procedures is still limited but it is clear that they can often reduce invasiveness and thereby be advantageous for patients.
Used appropriately, mixing and matching of components in the revision situation has no detrimental effect on implant survival and outcome.
Whenever possible, informed consent should be obtained.
Mismatch
Recommendation 6: It is crucial for surgeons to only combine implants that are compatible. Mismatch of components, where their sizes or connections do not fit, may have catastrophic effects. It is essential that appropriate measures should be put in place to avoid component mismatch.
Results of consensus voting: 100% agreement, 0% disagreement, 0% abstention
Mixing and matching components from more than one manufacturer is an active decision made by a surgeon and it can only be undertaken safely when all the components are matched for size, material and connection. They should fit together properly. Mismatch is different, and it is a surgical mistake. It is where a construct is put together where sizes or connections do not fit or match each other due to geometrical differences. A mismatch is a non-compatible combination of implant components. Its creation is regarded in the UK as a ‘never event’.
Examples include:
a femoral head with a different diameter to the internal diameter of the acetabular component with which it has been articulated (i.e. combining a 28 mm head with a 32 mm acetabular liner)
a femoral head with a different taper to the trunnion on the stem (i.e. combining a 12/14 head taper with a 11/13 stem taper)
femoro-tibial component size mismatch in TKA (i.e. the combination of a very large femoral condyle with a very small tibia base plate)
wrong sidedness such as combining a left TKA femoral component with a right tibia base plate
In a confidential survey among members of one national Orthopaedic Society, Stokes and Rutherford92 reported that 23% of surgeons had implanted mismatched components within the previous five years, occurring mainly in THA, but also TKA and other TJAs. In about half of the patients further surgery was necessary to correct the mistake. Howard93 stated that more than the expected number of hip head-liner mismatches and knee wrong-sided mismatches have been found in the NJR in the past, and besides incomplete or absent intraoperative check, unclear labelling of implants may have been a major reason. Wrong implant selection (incorrect size, wrong side or where parts of the prosthesis used are incompatible with each other) is sometimes recognized by the surgeon and operating theatre team and can be addressed during the procedure. If the mistake is recognized at a later date, a revision operation may be required. This might be after serious side effects or other problems have already affected the patient. Generally, the advice is to revise as soon as the mismatch has been unequivocally identified.
In view of the serious consequences of mismatch, several initiatives have been developed to reduce the risk of incompatible component selection. Odgaard et al94 piloted an online, real-time compatibility check in the operating theatre based on checking of the barcodes on the implant packages, before the packets were opened and expected that this process could significantly reduce the number of incompatibility events for hip and knee arthroplasty procedures.
In countries with established arthroplasty registries such as the National Joint Registry (NJR), wrong implant selection is picked up as a ‘never event’, immediately the data from the operation are uploaded. The writing on the screen turns red and a warning question is posed. The Healthcare Safety Investigation Branch (HSIB)95 and National Guideline Centre (UK)96 have also proposed measures to prevent these never events in relation to wrong implant selection. Ast et al97 found that through the use of a software verification system they could reduce selection errors that occur in the operating room (OR). They found that mismatch errors occurred in approximately 0.74% of the procedures they monitored, but these were all identified and rectified before implantation. It has been widely publicized that when such advanced procedures and systems are not available, the golden rule in the OR is to follow a comprehensive check list. First before starting surgery, then through double checking the implant boxes and the labels by the surgeon and by the nurse during surgery (before implantation) and then again just after and before the wound is closed.
Font size of the details on the box which contains the implant has been discussed and recommendations have been made.95
Head-liner mismatch in THA
Head-liner mismatch has been reported in hip resurfacing arthroplasty98–100 as well as conventional THA.37,101–103 In all cases the head size of the femoral component was different from the corresponding inner diameter of the acetabular cup. Although we could not find additional reports of head-cup mismatch, this complication may occur more frequently. The problem may present as recurrent dislocation or gross wear.
In terms of material mismatch the most striking examples have been mismatches involving ceramics. If ceramic heads are combined with inserts of incompatible ceramic (usually made by a different manufacturer), catastrophic failure may occur.40,104 Pairing metal heads with ceramic inlays is nowadays regarded as a never event.105
Reassuringly, the combination of alumina ceramic heads with delta ceramic liners from the same manufacturer has been widely and safely used.106,107
Taper mismatch in THA
Koper et al108 reported on a 12/14 stem taper that was combined with a 14/16 head taper causing dramatic metal wear, an increased release of metal ions and pseudotumor formation. They have not been alone in describing extremely worrying effects of taper mismatch. Hohman et al48 found metallosis and excessive wear of the stem taper after a head with a C-taper and a stem with a V40 taper were paired.
These clinical cases have been supported by finite element analysis (FEA) of mismatched taper connections in the laboratory. Using FEA, Ashkanfar et al109 reported on how a significant taper mismatch resulted in markedly increased wear and negative clinical outcomes which they combined with retrieval studies. Similar findings were reported by Fallahnezhad et al,110 who showed in an FEA of simulated fretting wear, that it increased with increased taper mismatch.
It has been shown 52 that with mismatched components the mean fracture strength of the ceramic heads was reduced to about 50% of the recommended FDA strength.
Femoro-tibial component mismatch in TKA
Most TKA systems allow a certain degree of femoro-tibial component size mismatch. Heylen et al111 have investigated whether and how the size of mismatch influences the clinical outcome in a clinical study. They could not find a statistically significant difference in patient-relevant outcomes between patients with no mismatch and patients with tibial component larger than femoral component or femoral component one size as well as two sizes larger than the tibial component. They even described that, compared to men, women tend to have more component size mismatch. Berend et al112 reported even lower revision rates with mismatched components compared to size-matched components. Nevertheless, there is a conflicting report from the Australian registry,113 where TKA revision rates were significantly higher when the femoral size was greater than the tibia, compared to both equal size as well as to tibial size greater than femoral size. The authors discussed edge loading of polyethylene and increased tibial component stress as potential explanations for their findings.
The challenge with component size mismatch in TKA is that most TKA manufacturers allow such a mismatch to a certain degree (i.e. by two component sizes), which would lead to compatible conditions. Nevertheless, if the size difference of the mismatched components is outside the range as specified by the manufacturer, a non-compatible combination is created.
Summary:
Mismatch may lead to adverse clinical events which are avoidable.
Acknowledging the existence of the problem and introducing robust checking protocols will mitigate against its occurrence.
It is suggested that clear and improved labelling of implants by the manufacturers may further reduce the risk of incorrect pairing of TJA components.
General recommendations
Recommendation 7: As always, surgeons must be fully aware of the features of the components that they use off-label, must be appropriately trained and must audit their results.
Results of consensus voting: 100% agreement, 0% disagreement, 0% abstention
Wherever possible, surgeons must be fully cognisant of the salient features, the accepted uses and the required surgical technique for the use an off-label device. They should be aware of any off-label and on-label use of the product and the scientific basis behind its design. Surgeons should only use an off-label device after they have failed to find an on-label one that would be a suitable implant.
It is expected that the surgeon will be able to show that the decision to go off-label would be expected to lead to a better clinical outcome than would have been the case following the use of an on-label device. These important points will need to be included in the preoperative counselling of the patient.12
Because there is little or no follow-up data on the performance of off-label devices, careful and ongoing follow-up is essential, both to ensure a satisfactory outcome for the patient and the knowledge base of the surgeon. Surgeons should be prepared to share their experience with others.
Recommendation 8: As mix & match is an off-label procedure, the reasons should be explained to the patient and informed consent obtained.
Results of consensus voting: 96.43% agreement, 0% disagreement, 3.57% abstention
It is standard practice to fully counsel patients with regard to all aspects of their operation but if it is the intention of the surgeon to use off-label implants or to mix & match implants, for ethical, moral and medico-legal reasons, fully detailed consent is even more important. The patient deserves a detailed breakdown of the surgeon’s own experience with the off-label implants and/or mixing and matching. It is important for the surgeon to evaluate and record the patient’s reaction to the surgical pathway and accompanying explanations that they have covered during their discussion. In case of concern either by the patient or the surgeon, the opportunity of a second opinion should be offered.
Ethical and moral issues are raised whenever a drug or device is used in an unapproved manner. Physicians using devices in an off-label fashion must be aware of these issues and how they affect their patients. Reviewing an ethical checklist before embarking on the use of a device or drug in an off-label fashion can alert the physician to potential ethical and moral conflicts. The ethical physician always will place his or her patient's well-being and best interests above all else. Using this pledge as the cornerstone of all their clinical decision making, the virtuous physician is able to offer the most innovative and new procedures without compromising his or her ethical or moral obligations to their patients.13
Recommendation 9: If the application of off-label and mix & match follows recommendations 1–8 for the clinical benefit of the patient, surgeons should not be considered as ‘implant manufacturers’.
Results of consensus voting: 89.29% agreement, 3.57% disagreement, 7.14% abstention
Off-label application
One type of off-label use is the application of an implant in a situation which is not approved by the manufacturer. According to the MHRA,2 this will be at surgeon’s own risk and they or their employers ‘. . .could become liable for civil claims for damages from injured patients or their families if something goes wrong with the device’.2 Many IFUs list ‘relative’ or even ‘absolute’ contraindications (i.e. soft tissue insufficiency or compromised bone stock creating a risk of instability or fixation failure, allergy to implant materials, renal insufficiency, neoplasms, obesity). If the patient suffers from such a condition, the application of an implant is off-label and might bear the risk of legal implications in case of failure. Obesity is probably the most important example, as the incidence of arthritic patients with obesity is raising worldwide and may pose an irresolvable dilemma to the surgeon. If severe pain persists in spite of appropriate conservative treatment and recommended weight reduction is not possible, there is only the choice between refusing an arthroplasty operation or performing it off-label. In these situations, the surgeon should explicitly inform the patient about potential risks and benefits of both alternatives (including the specified formal contraindication) and obtain written informed consent before offering the surgical procedure. Otherwise, there is a potential danger being accused of having violated a standard of care and committed a fault causing liability.30
Mix & match application
Implant manufacturers are responsible for the release of implants from their production to the hospitals. Prior to market release all medical implants have to be approved and marked (CE – Conformité Européene – certificate) by an appropriate body. This approval is given if products meet the requirements of the former Medical Devices Directive (now Medical Device Regulation MDR), and documents show that the implant does not entail a safety risk (Directive 93/42/EEC 1993, Regulation (EU) 2017/745 2017). Surgeons who mix components from different manufacturers in a combination which has not been tested or that does not comply with the product instructions as provided by the manufacturer, must be extremely careful, as they could potentially be asked to take responsibility for a new product. It is not clear if the same possibility could happen when they use different implants from the same manufacturer, as not all the possible combinations of product lines, for example of cups/liners and stems/heads, can be tested. Moreover, companies can merge by acquisition with consequent mix & match of components. Peters et al114 expressed the opinion that surgeons and other healthcare providers who mix components from different manufacturers could qualify as a ‘manufacturer of a finished product’ to whom the liability regime of the Directive applies. The European Product Liability Directive (85/374/EEC) states that the producer of a product is liable for damages suffered by a patient if this product appears to be defective. This Directive has been transposed into national law in all member states of the European Union. For these reasons, surgeons are required to be extremely cautious, even if they use mix & match for better clinical outcomes, that there is no evidence of defective combination nor incompatibility.
In 2010, the MHRA2 circulated a warning to all trusts in England that devices should not be modified. In some EU countries it has been hypothesized that the surgeon is legally considered a ‘designer’ of a new hip device, once he decides to mix and match components for THA. In other European countries, however, such a formal implication has never been considered, making regulation even more difficult to interpret.
This heterogeneous practice may lead to legal implications and carry the risk of liability toward patients in case of failure clearly due to mix & match. Very recently, Peters et al114 approached this topic in an annotation paper. The authors even mention the possibility that mixing of components might be considered negligent when unauthorized and discouraged by the manufacturer, untested by orthopaedic surgeons and unapproved by law, when medical publications have shown clinical risks. Interestingly, the same group of authors show in a Dutch Arthroplasty Registry study, how mixed and non-mixed components had similar medium-term revision rates.5 They also report that liability regimes in this field vary by country in the EU and that a search of case law in the UK, Germany and the Netherlands revealed that, until now, no orthopaedic surgeon has never been held responsible as the manufacturer of a finished product of mixed components.114
In revision surgery, where a combination of components from different manufacturers can prevent additional patient morbidity, and appropriately matching spare parts are sometimes no longer available, the potential legal impact of mixing may be more difficult. It is not acceptable, therefore, that surgeons, who retain a well-fixed stem or cup (in order to reduce morbidity as best as possible) and combine it with a head or cement a liner from another company if the previous one is not available or feasible, are regarded as ‘manufacturers’ in a legal sense.
Summary
It is important that surgeons are well aware of potential liability problems when considering off-label application and especially mix & match while taking care of their patients in the best of their evidence-based practice.
Key elements for the protection of patients as well as surgeons in such a situation should include comprehensive patient information about features of implants, possible alternatives (based on a procedurally well-defined and documented benefit risk analysis) and informed consent.
In addition, it is necessary to develop regulations which protect surgeons who mix components in primary or revision arthroplasty based on best scientific evidence and knowledge from the risk of litigation.
Recommendation 10: Further research is necessary to obtain more data about the appropriate indications and outcomes for off-label procedures in THA and TKA.
Results of consensus voting: 100% agreement, 0% disagreement, 0% abstention
It is clear from the previous chapters that many surgeons feel that there are strong indications for the use of off-label implants and mixing and matching. It has also been shown that there are dangers and sometimes an increased lack of predictability of outcomes.
By definition, none of these products or combinations carry a CE mark, or if they have a CE mark and are being used off-label the CE mark is unlikely to be relevant. This means they have not been comprehensively tested. Pre-clinical testing of so far unapproved mix & match cases must have its supporters. These tests could focus on the most likely causes of failure such as accelerated wear, increased fretting and corrosive behaviour of the mixed and matched materials. They would include a full range of mechanical testing and tests to include, for example, fracture performance, galvanic corrosion etc.52,115
Arthroplasty registries
Most European countries have national or regional joint registries and although not all of them monitor implants on a regular basis many do. Several of them are able to monitor mix & match very accurately and the NJR offers the facility of ‘supplier feedback’ to manufacturers who are therefore able to monitor the use of their devices in real time, including mix & match. The Dutch Arthroplasty Register (LROI) offers offline ‘supplier feedback’ to manufacturers in order to monitor past performance of their devices (also including mix & match). Many monitor patient characteristics such as BMI, and these data will also be available. By developing the registries a little further, it would be perfectly possible to generate a rich data set where many of these patient as well as implant characteristics on implant performance (i.e. implant survival) could be evaluated for safety. The latter can be used as real evidence feedback to surgeons, to guide them in their clinical decisions.
To further optimize outcomes for patients, all these data could be collated into an implant performance indicator (IPI), which allows multifactorial judgement (i.e. influence of implant, mix & match and non-mix & match, surgical practice, hospital performance) as a feedback to all those who are involved in TJA. The latter can be used as input into further research of the effects of mix & match and all off-label activity.
Retrieval studies
Studies on revised implant components may help to evaluate whether and to what extend mix & match conditions lead to a relevant material degradation. By comparing matched and mixed cases, retrieval studies which are considering the real conditions in the human body may help to better evaluate the effect of mixing and matching.54
Recommendation 11: Where manufacturers have ceased regular production of an implant, they make provision for some of these legacy devices to remain available when required in revision operations. This initiative should be supported by regulators to ensure simplified re-certification.
Results of consensus voting: 100% agreement, 0% disagreement, 0% abstention
Whilst the hope of both the patient and the surgeon is that their new joint replacement will last them throughout the rest of the patient’s life, 5–8% of the best performing joint replacements will have required revision by the 15th year from their insertion. Revision is always a major procedure and by the time it is required the patient may be elderly and be suffering from comorbidities that make the operation riskier and rehabilitation more prolonged. The problems that lead to revision include wear, osteolysis (loss of bone around the implant) and very importantly periprosthetic fractures that can occur either side of all TJAs and dislocation in THA.
In this context it is desirable that the revision could be as uninvasive as possible, as well as tissue/implant sparing, especially in the older and more fragile patients who received a TJA many years before. For this aim, ‘spare parts’ of the implant must be available ideally for ever. Unfortunately, every orthopaedic surgeon (together with his/her patient) has had to undertake these challenging operations without the ‘same’ implants being available. Exchanging a perfectly functioning implant just because mix & match has been banned cannot be acceptable. This situation can be even worse in TKA and can also apply to surgical instruments.
The excuses that have been offered by manufacturers for legacy devices not being available are varied:
The implant is no longer being marketed for commercial reasons.
The original manufacturing company has been acquired by another company who are not interested in promoting that specific device any longer.
The costs of maintaining the stock.
Problems with sterilization.
Re-certification and medical device regulations.
It is reported that it is possible to have custom made or equivalent implants by the companies, but this option has found little favour on account of delays and expense. In some countries these requests may have to go to health ministers and also to ethics committees. Revision can be an urgently required procedure and requests along these pathways are rarely dealt with expeditiously.
Analysis of previous and new regulations for implant use is outside the scope of this article, but we strongly advocate that these demanding clinical situations should be managed in a proper and compassionate way both by manufacturers and by regulatory bodies, for the very best interest of patients.
An alternative could be that when surgeons start using a particular joint replacement, they could insist that they will only use it if there is a written guarantee for ‘spare parts’ to be indefinitely available after regular production of an implant has stopped.
Recommendation 12: In order to ensure safety of head-taper assembly in hip arthroplasty, standardization committees and implant manufacturing industry are encouraged to develop a uniform definition which integrates geometric and topographical features of the taper to reduce the potential of incompatibility.
Results of consensus voting: 90% agreement, 3.33% disagreement, 6.67% abstention
In a modular femoral component of a THA, the head is held on to the stem by a taper junction. The femoral taper should fit tightly into the head taper. The majority of tapers have unique properties and dimensions, i.e. length, taper angle, diameter, straightness, roundness, surface finish and surface properties.43 These differences are sometimes very subtle and not easily visible to the naked eye. It is agreed that for a secure and durable fit the femoral ball head taper and the stem taper should match each other precisely.
Trebše et al59 reported data from their institutional registry that showed that when the head and stem were from different manufacturers, the clinical results were inferior. On the basis of their findings, they recommended that the regulating bodies should introduce a standard taper, with defined tolerances, that would be adopted universally and its use by manufacturers should be compulsory.
Thus contemporary research has confirmed what Cales and Stefani116 advocated over 20 years ago. They cited several very important advantages of the standardization of bores and cones:
Reduction in the risk of a mistake during surgery
Smaller hospital inventories resulting in a direct and significant economic benefit
The main obvious advantage would be for the surgeon and for the patient as it would allow a well-fitting taper connection during revision surgery in cases where stem retention was desirable and a replica head (with the original matched taper) was not available.
Whilst recognizing the independence and competitiveness of the manufacturers, it has been demonstrated that there is a strong argument for implant manufacturers to come to an agreement with the regulatory bodies for there to be a standard design for all stem/head combinations. Eventually this could become mandatory.
Furthermore, standardization of the articular bearing interface might be a solution to reduce the clinical risks of mix & match. In fact, some dimensional aspects are already standardized. For example, ISO 7206-2 specifies the bearing dimensions and requires that the spherical polyethylene liner shall have a diameter slightly larger (+0.1 to 0.3 mm) than the nominal bearing diameter. Consequently, pinching of the bearing is not expected even if a head and a polyethylene liner from different manufacturers are combined, although this is not the intention under the ISO standard. If further interfaces were standardized, generalized pre-clinical tests may help to identify safe combinations which might then be approved. If both interfaces are standardized it should be expected that the failure risk of mixing and matching can be reduced. Nevertheless, the CE approval process lies in the hands of the implant manufactures and they would need to assume responsibility if they approved mix & match for clinical application, which is a challenge for the manufactures. Research may help to bridge the gap.
Conclusions
Up until now manufacturers and regulators have instituted their own policies around the issues of ‘off-label’ and ‘mix & match’ and apparently applied them without always taking into account the needs of some patients. Surgeons have sometimes disregarded the instructions of manufacturers and taken it upon themselves to go off-label or to mix & match components from more than one manufacturer. Our first conclusion is that the status quo is not satisfactory in terms of contemporary practice, for any of the parties involved, and that each party must take into account the views and concerns of the other parties. We have concluded that by providing a forum for each of these groups to share their views and concerns there is scope for agreement about the major issues involved. Evidently it is possible to improve their understanding of the challenges that these issues bring, in the safe and effective management of patients requiring joint replacement. We found that the consensus voting was a very effective method of focusing the thoughts of all the participants (see Table 3).
Table 3.
Overview on recommendations with voting results at the consensus conference
| Recommendation | % of delegate votes | Eligible to vote | |||
|---|---|---|---|---|---|
| Agree | Disagree | Abstain | |||
| 1 | There may be indications for the application of THA or TKA implants for purposes outside the one for which the manufacturer intended both in primary and revision arthroplasty (off-label use). | 100 % (n = 26) |
0% | 0% | 26 |
| 2 | Prior to the application of a medical device for hip or knee arthroplasty off-label, surgeons should balance the risks and benefits to the patient, obtain informed consent, and document the decision process appropriately. | 100% (n = 26) |
0% | 0% | 26 |
| 3 | In obese patients, primary and revision arthroplasty is associated with increased peri- and postoperative risks. Off-label use of implants must be considered carefully by surgeons and patients. | 100% (n = 25) |
0% | 0% | 25 |
| 4 | Due to product liability it is commonly accepted in primary THA to use all components from one manufacturer. If evidence suggests, however, that the combination of devices from different manufacturers has superior results, patients may benefit from selective and documented application of mixing and matching. | 96.15%(n = 25) | 3.85% (n = 1) |
0% | 26 |
| 5 | When, in revision THA and TKA, only one component needs revising, mix & match should be allowed. Taking the patient’s risk-benefit balance, the available evidence and the current state of the art into account, surgeons should be allowed to avoid replacing a component purely to avoid mix & match. | 100% (n = 28) |
0% | 0% | 28 |
| 6 | It is crucial for surgeons to only combine implants that are compatible. Mismatch of components, where their sizes or connections do not fit, may have catastrophic effects. It is essential that appropriate measures should be put in place to avoid component mismatch. | 100% (n = 29) |
0% | 0% | 29 |
| 7 | As always, surgeons must be fully aware of the features of the components that they use off-label, must be appropriately trained and must audit their results. | 100% (n = 29) |
0% | 0% | 29 |
| 8 | As mix & match is an off-label procedure, the reasons should be explained to the patient and informed consent obtained. | 96.43% (n = 27) | 0% | 3.57% (n = 1) | 28 |
| 9 | If the application of off-label and mix & match follows recommendations 1–8 for the clinical benefit of the patient, surgeons should not be considered as ‘implant manufacturers’. | 89.29% (n = 25) |
3.57% (n = 1) |
7.14% (n = 2) |
28 |
| 10 | Further research is necessary to obtain more data about the appropriate indications and outcomes for off-label procedures in THA and TKA. | 100% (n = 27) |
0% | 0% | 27 |
| 11 | Where manufacturers have ceased regular production of an implant, they make provision for some of these legacy devices to remain available when required in revision operations. This initiative should be supported by regulators to ensure simplified re-certification. | 100% (n = 27) |
0% | 0% | 27 |
| 12 | In order to ensure safety of head-taper assembly in THA, standardization committees and implant manufacturing industry are encouraged to develop a uniform definition which integrates geometric and topographical features of the taper to reduce the potential of incompatibility. | 90.0% (n = 27) |
3.33% (n = 1) |
6.67% (n = 2) |
30 |
Our final conclusion is that patients should always be at the centre of any discussion regarding these issues, if it involves them, and this cannot be overemphasized. We look forward to these conclusions being acted upon.
Acknowledgments
The authors would like to thank all other members of the Implant and Patient Safety (IPSI) Steering Group, who participated during the consensus process: Achakri H., Atilla B., Betteridge N., Cónsul-Tejero E.*, Epinette J.A., Hailer N.P., Hirschmann T., Marchetti F., Muenger P., Münnig M., Neyret P., Orlandini L., Pasquier G., Ruck S., Tranqulilli-Leali P., van Hellemondt G., Verheyen C., Wiek D., Wirtz D., Zündorf J.*
*Cónsul-Tejero E. and Zündorf J. as representatives of the Federal Institute for Drugs and Medical Devices (BfArM) have only commented and provided a vote on recommendation 12. All other recommendations have been neither commented nor voted on by BfArM. The use of components and/or combinations of components not covered by the instructions for use accompanying the devices is not recommended by BfArM. According to their regulatory point of view, only authorized combinations should be used.
In addition, we would like to express our gratitude to all EFORT board members and national delegates who participated at the final consensus meeting, as well as Cornelia Lützner, Julia Scheibe and Sabrina Marchal, who provided administrative support. We appreciate the generous financial support (unrestricted educational grant) from the Medical Faculty of the Technical University of Dresden. Finally, we would like to thank the members of the International Society of Arthroplasty Registries (ISAR), who provided data for Table 1, and the National Joint Registry for other tables.
Footnotes
ICMJE Conflict of interest statement: KPG is a board member and Immediate Past President of EFORT (2020–2021), and also a board member of the German Society of Orthopaedics and Traumatology. RGHHN is currently Secretary General of EFORT (2021–2023). KPG has received payments via the University of Dresden from EFORT, in support of this manuscript. KPG, LZ, PK, PKA and TL all received logistic help and staff support for organization of the consensus conference from EFORT, and support from the Medical Faculty at the University of Dresden for infrastructure (room and audio-visual cost, staff support) for the organization of the consensus conference (unrestricted educational grants). The authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. US Food and Drug Administration: Guidance for Institutional Review Boards and Clinical Investigators. ‘Off-label’ and investigational use of marketed drugs, biologics and medical devices. Rockville, MD: FDA, 1998. [Google Scholar]
- 2. Medicines and Healthcare products Regulatory Agency (MHRA). Guidance: off-label use of a medical device 2014. https://www.gov.uk/government/publications/medical-devices-off-label-use/off-label-use-of-a-medical-device. (date last accessed 30 April 2021).
- 3. Tucker K. ‘Mix and match’: the use of components from more than one manufacturer in a total hip replacement. Orthopaedic Proceedings 2018;97-B:Supp 12. [Google Scholar]
- 4. Malcolm T, Szubski CR, Schiltz NK, Klika AK, Koroukian SM, Barsoum WK. Prevalence and perioperative outcomes of off-label total hip and knee arthroplasty in the United States, 2000–2010. J Arthroplasty 2015;30:1872–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Peters RM, van Steenbergen LN, Bulstra SK, et al. Nationwide review of mixed and non-mixed components from different manufacturers in total hip arthroplasty. Acta Orthop 2016;87:356–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cats-Baril W, Gehrke T, Huff K, Kendoff D, Maltenfort M, Parvizi J. International consensus on periprosthetic joint infection: description of the consensus process. Clin Orthop Relat Res 2013;471:4065–4075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zagra L. Advances in hip arthroplasty surgery: what is justified? EFORT Open Rev 2017;2:171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu J, Small T, Masch J, Goldblum A, Klika A, Barsoum W. Third place award off-label versus on-label outcomes of total joint arthroplasty. Curr Orthop Pract 2016;27:355–359. [Google Scholar]
- 9. Marie-Hardy L, O’Loughlin P, Bonnin M, Ait Si, Selmi T. Two cases of deliberate implant mismatch in knee arthroplasty. SICOT J 2020;6:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nunley P, Frank K, Stone M. Patient selection in cervical disc arthroplasty. Int J Spine Surg 2020;14:S29–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McFarland EG, Huri G, Hyun YS, Petersen SA, Srikumaran U. Reverse total shoulder arthroplasty without bone-grafting for severe glenoid bone loss in patients with osteoarthritis and intact rotator cuff. J Bone Joint Surg [Am] 2016;98-A:1801–1807. [DOI] [PubMed] [Google Scholar]
- 12. Taylor BC, Triplet JJ, El-Sabawi T. Off-label use in orthopaedic surgery. J Am Acad Orthop Surg 2019;27:e767–e774. [DOI] [PubMed] [Google Scholar]
- 13. Zindrick MR. Orthopaedic surgery and Food and Drug Administration off-label uses. Clin Orthop Relat Res 2000;378:31–38. [DOI] [PubMed] [Google Scholar]
- 14. Günther KP, Wegner T, Kirschner S, Hartmann A. [Modular reconstruction in acetabular revision with antiprotrusio cages and metal augments: the cage-and-augment system]. Oper Orthop Traumatol 2014;26:141–155. [DOI] [PubMed] [Google Scholar]
- 15. Anand R, Graves SE, de Steiger RN, et al. What is the benefit of introducing new hip and knee prostheses? J Bone Joint Surg [Am] 2011;93-A:51–54. [DOI] [PubMed] [Google Scholar]
- 16. Benson M, Boehler N, Szendroi M, Zagra L, Puget J. Ethical standards for orthopaedic surgeons. J Bone Joint Surg [Br] 2014;96-B:1130–1132. [DOI] [PubMed] [Google Scholar]
- 17. Craik JD, Bircher MD, Rickman M. Hip and knee arthroplasty implants contraindicated in obesity. Ann R Coll Surg Engl 2016;98:295–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD, Team I; INFORM Team. Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. PLoS One 2016;11:e0150866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu W, Wahafu T, Cheng M, Cheng T, Zhang Y, Zhang X. The influence of obesity on primary total hip arthroplasty outcomes: a meta-analysis of prospective cohort studies. Orthop Traumatol Surg Res 2015;101:289–296. [DOI] [PubMed] [Google Scholar]
- 20. Ma Z, Guo F, Qi J, Xiang W, Zhang J. Meta-analysis shows that obesity may be a significant risk factor for prosthetic joint infections. Int Orthop 2016;40:659–667. [DOI] [PubMed] [Google Scholar]
- 21. Onggo JR, Onggo JD, de Steiger R, Hau R. Greater risks of complications, infections, and revisions in the obese versus non-obese total hip arthroplasty population of 2,190,824 patients: a meta-analysis and systematic review. Osteoarthritis Cartilage 2020;28:31–44. [DOI] [PubMed] [Google Scholar]
- 22. Ponnusamy KE, Somerville L, McCalden RW, Marsh J, Vasarhelyi EM. Revision rates and functional outcome scores for severely, morbidly, and super-obese patients undergoing primary total hip arthroplasty: a systematic review and meta-analysis. JBJS Rev 2019;7:e11. [DOI] [PubMed] [Google Scholar]
- 23. Boyce L, Prasad A, Barrett M, et al. The outcomes of total knee arthroplasty in morbidly obese patients: a systematic review of the literature. Arch Orthop Trauma Surg 2019;139:553–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chaudhry H, Ponnusamy K, Somerville L, McCalden RW, Marsh J, Vasarhelyi EM. Revision rates and functional outcomes among severely, morbidly, and super-obese patients following primary total knee arthroplasty: a systematic review and meta-analysis. JBJS Rev 2019;7:e9. [DOI] [PubMed] [Google Scholar]
- 25. Sun K, Li H. Body mass index as a predictor of outcome in total knee replace: a systemic review and meta-analysis. Knee 2017;24:917–924. [DOI] [PubMed] [Google Scholar]
- 26. Barrett MC, Whitehouse MR, Blom AW, Kunutsor SK. Host-related factors for venous thromboembolism following total joint replacement: a meta-analysis of 89 observational studies involving over 14 million hip and knee replacements. J Orthop Sci 2020;25:267–275. [DOI] [PubMed] [Google Scholar]
- 27. Second International Consensus Meeting on Musculoskeletal Infection. Proceedings of the Second International Consensus Meeting on Musculoskeletal Infection: Hip and Knee 2019. https://icmphilly.com/wp-content/uploads/2018/11/Hip-and-Knee.pdf (date last accessed 30 May 2021).
- 28. Cizmic Z, Feng JE, Huang R, et al. Hip and knee section, prevention, host related: Proceedings of International Consensus on Orthopedic Infections. J Arthroplasty 2019;34:S255–S270. [DOI] [PubMed] [Google Scholar]
- 29. Ighani Arani P, Wretenberg P, Ottosson J, Robertsson O, W-Dahl A. Bariatric surgery prior to total knee arthroplasty is not associated with lower risk of revision: a register-based study of 441 patients. Acta Orthop 2021;92:97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ploeger MM, Müller NH, Wirtz DC, Kohlhof H. [Obesity in revision total knee arthroplasty: a systematic review and legal assessment]. Z Orthop Unfall 2018;156:436–442. [DOI] [PubMed] [Google Scholar]
- 31. Roth A, Khlopas A, George J, et al. The effect of body mass index on 30-day complications after revision total hip and knee arthroplasty. J Arthroplasty 2019;34:S242–S248. [DOI] [PubMed] [Google Scholar]
- 32. Kenney C, Dick S, Lea J, Liu J, Ebraheim NA. A systematic review of the causes of failure of revision total hip arthroplasty. J Orthop 2019;16:393–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Herold F, Nötzli H, Eijer H. Short proximal components in modular revision stems carry a higher risk for stem fractures. Hip Int 2021;31:398–403. [DOI] [PubMed] [Google Scholar]
- 34. Krueger DR, Guenther KP, Deml MC, Perka C. Mechanical failure of 113 uncemented modular revision femoral components. J Bone Joint Surg [Br] 2020;102-B:573–579. [DOI] [PubMed] [Google Scholar]
- 35. Krull A, Morlock MM, Bishop NE. Factors influencing taper failure of modular revision hip stems. Med Eng Phys 2018;54:65–73. [DOI] [PubMed] [Google Scholar]
- 36. Lakstein D, Eliaz N, Levi O, et al. Fracture of cementless femoral stems at the mid-stem junction in modular revision hip arthroplasty systems. J Bone Joint Surg [Am] 2011;93-A:57–65. [DOI] [PubMed] [Google Scholar]
- 37. Barrack RL, Burke DW, Cook SD, Skinner HB, Harris WH. Complications related to modularity of total hip components. J Bone Joint Surg [Br] 1993;75-B:688–692. [DOI] [PubMed] [Google Scholar]
- 38. Higgs GB, Hanzlik JA, MacDonald DW, Gilbert JL, Rimnac CM, Kurtz SM; Implant Research Center Writing Committee. Is increased modularity associated with increased fretting and corrosion damage in metal-on-metal total hip arthroplasty devices? A retrieval study. J Arthroplasty 2013;28:2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kurtz SM, Kocagöz SB, Hanzlik JA, et al. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin Orthop Relat Res 2013;471:3270–3282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Morlock M, Nassutt R, Janssen R, Willmann G, Honl M. Mismatched wear couple zirconium oxide and aluminum oxide in total hip arthroplasty. J Arthroplasty 2001;16:1071–1074. [DOI] [PubMed] [Google Scholar]
- 41. Sonntag R, Reinders J, Rieger JS, Heitzmann DWW, Kretzer JP. Hard-on-hard lubrication in the artificial hip under dynamic loading conditions. PLoS One 2013;8:e71622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mueller U, Bormann T, Schroeder S, Kretzer JP. Taper junctions in modular hip joint replacements: what affects their stability? J Mech Behav Biomed Mater 2021;116:104258. [DOI] [PubMed] [Google Scholar]
- 43. Mueller U, Panzram B, Braun S, Sonntag R, Kretzer JP. Mixing of head-stem components in total hip arthroplasty. J Arthroplasty 2018;33:945–951. [DOI] [PubMed] [Google Scholar]
- 44. Carli A, Politis A, Zukor D, Huk O, Antoniou J. Clinically significant corrosion at the head-neck taper interface in total hip arthroplasty: a systematic review and case series. Hip Int 2015;25:7–14. [DOI] [PubMed] [Google Scholar]
- 45. Esposito CI, Wright TM, Goodman SB, Berry DJ; Clinical, Biological and Bioengineering Study Groups from Carl T. Brighton Workshop. What is the trouble with trunnions? Clin Orthop Relat Res 2014;472:3652–3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Parekh JJH, Chan N, Noble P. Effect of angular mismatch tolerance on trunnion micro-motion in metal-on-metal THA designs. Orthop Proc 2013;95-B:261. [Google Scholar]
- 47. Hernigou P, Queinnec S, Flouzat Lachaniette CH. One hundred and fifty years of history of the Morse taper: from Stephen A. Morse in 1864 to complications related to modularity in hip arthroplasty. Int Orthop 2013;37:2081–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hohman DW, Affonso J, Anders M. Ceramic-on-ceramic failure secondary to head-neck taper mismatch. Am J Orthop 2011;40:571–573. [PubMed] [Google Scholar]
- 49. Hussenbocus S, Kosuge D, Solomon LB, Howie DW, Oskouei RH. Head-neck taper corrosion in hip arthroplasty. BioMed Res Int 2015;2015:758123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chana R, Esposito C, Campbell PA, Walter WK, Walter WL. Mixing and matching causing taper wear: corrosion associated with pseudotumour formation. J Bone Joint Surg [Br] 2012;94-B:281–286. [DOI] [PubMed] [Google Scholar]
- 51. Callaway GH, Flynn W, Ranawat CS, Sculco TP. Fracture of the femoral head after ceramic-on-polyethylene total hip arthroplasty. J Arthroplasty 1995;10:855–859. [DOI] [PubMed] [Google Scholar]
- 52. Gührs J, Körner M, Bechstedt M, Krull A, Morlock MM. Stem taper mismatch has a critical effect on ceramic head fracture risk in modular hip arthroplasty. Clin Biomech (Bristol, Avon) 2017;41:106–110. [DOI] [PubMed] [Google Scholar]
- 53. Cook R, Latham J, Wood R. The performance of mixed manufacturer metal on metal total hip replacements. JISRF Reconstructive Review 2017;7:13–20. [Google Scholar]
- 54. Whittaker RK, Hothi HS, Meswania JM, et al. The effect of using components from different manufacturers on the rate of wear and corrosion of the head-stem taper junction of metal-on-metal hip arthroplasties. J Bone Joint Surg [Br] 2016;98-B:917–924. [DOI] [PubMed] [Google Scholar]
- 55. Werner PH, Ettema HB, Witt F, Morlock MM, Verheyen CC. Basic principles and uniform terminology for the head-neck junction in hip replacement. Hip Int 2015;25:115–119. [DOI] [PubMed] [Google Scholar]
- 56. Taylor JW, Frampton C, Rothwell AG. Long-term survival of total hip arthroplasty using implants from different manufacturers. J Arthroplasty 2018;33:491–495. [DOI] [PubMed] [Google Scholar]
- 57. Tucker K, Pickford M, Newell C, Howard P, Hunt LP, Blom AW. Mixing of components from different manufacturers in total hip arthroplasty: prevalence and comparative outcomes. Acta Orthop 2015;86:671–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Swedish Hip Arthroplasty Register. Annual report 2019. https://www.researchgate.net/publication/349426568_Swedish_Hip_Arthroplasty_Register_Annual_report_2019 (date last accessed 30 June 2021).
- 59. Trebše R, Valič M, Savarin D, Milošev I, Levašič V. Survival rate of total hip replacements with matched and with mixed components with 10.7 years mean follow-up. Hip Int 2020. 10.1177/1120700020972710 [Epub ahead of print]. [DOI] [PubMed]
- 60. Zagra L, Maccario C, Mondini A, Bianchi L. Treatment of failures related to articulation material in THA. A comprehensive algorithm of surgical options and open questions. HIP Int. 2014;24:48-57. 10.5301/hipint.5000170 [DOI] [PubMed] [Google Scholar]
- 61. Weber P, Steinbrück A, Paulus AC, et al. [Partial exchange in total hip arthroplasty: what can we combine?]. Orthopade 2017;46:142–147. [DOI] [PubMed] [Google Scholar]
- 62. Kim KW, Yoo JJ, Kim MN, Kim HJ. Isolated acetabular liner exchange for polyethylene wear and osteolysis with well-fixed metal shell. Clin Orthop Surg 2019;11:270–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Helwig P, Konstantinidis L, Hirschmüller A, et al. Modular sleeves with ceramic heads in isolated acetabular cup revision in younger patients: laboratory and experimental analysis of suitability and clinical outcomes. Int Orthop 2013;37:15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hoberg M, Konrads C, Huber S, et al. Outcome of a modular head-neck adapter system in revision hip arthroplasty. Arch Orthop Trauma Surg 2015;135:1469–1474. [DOI] [PubMed] [Google Scholar]
- 65. Jack CM, Molloy DO, Walter WL, Zicat BA, Walter WK. The use of ceramic-on-ceramic bearings in isolated revision of the acetabular component. J Bone Joint Surg [Br] 2013;95-B:333–338. [DOI] [PubMed] [Google Scholar]
- 66. Kim Y, Kim YH, Hwang KT, Choi IY. Isolated acetabular revision with ceramic-on-ceramic bearings using a ceramic head with a metal sleeve. J Arthroplasty 2014;29:2420–2423. [DOI] [PubMed] [Google Scholar]
- 67. Woelfle JV, Fraitzl CR, Reichel H, Wernerus D. Significantly reduced leg length discrepancy and increased femoral offset by application of a head-neck adapter in revision total hip arthroplasty. J Arthroplasty 2014;29:1301–1307. [DOI] [PubMed] [Google Scholar]
- 68. Dabis J, Hutt JR, Ward D, Field R, Mitchell PA, Sandiford NA. Clinical outcomes and dislocation rates after hip reconstruction using the Bioball system. Hip Int 2020;30:609–616. [DOI] [PubMed] [Google Scholar]
- 69. Callaghan JJ, Hennessy DW, Liu SS, Goetz KE, Heiner AD. Cementing acetabular liners into secure cementless shells for polyethylene wear provides durable mid-term fixation. Clin Orthop Relat Res 2012;470:3142–3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Delanois RE, Seyler TM, Essner A, Schmidig G, Mont MA. Cementation of a polyethylene liner into a metal shell. J Arthroplasty 2007;22:732–737. [DOI] [PubMed] [Google Scholar]
- 71. Rivkin G, Kandel L, Qutteineh B, Liebergall M, Mattan Y. Long term results of liner polyethylene cementation technique in revision for peri-acetabular osteolysis. J Arthroplasty 2015;30:1041–1043. [DOI] [PubMed] [Google Scholar]
- 72. Callaghan JJ, Parvizi J, Novak CC, et al. A constrained liner cemented into a secure cementless acetabular shell. J Bone Joint Surg [Am] 2004;86-A:2206–2211. [DOI] [PubMed] [Google Scholar]
- 73. Bensen CV, Del Schutte H, Jr, Weaver KD. Mechanical stability of polyethylene liners cemented into acetabular shells. Crit Rev Biomed Eng 2000;28:7–10. [DOI] [PubMed] [Google Scholar]
- 74. Bedard NA, Tetreault MW, Hanssen AD, et al. Intermediate to long-term follow-up of cementing liners into well-fixed acetabular components. J Bone Joint Surg [Am] 2020;102-A:1397–1404. [DOI] [PubMed] [Google Scholar]
- 75. Young GH, Abdel MP, Amendola RL, Goetz DD, Lewallen DG, Callaghan JJ. Cementing constrained liners into secure cementless shells: a minimum 15-year follow-up study. J Arthroplasty 2017;32:3480–3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Brown TS, Tibbo ME, Arsoy D, et al. Long-term outcomes of constrained liners cemented into retained, well-fixed acetabular components. J Bone Joint Surg [Am] 2019;101-A:620–627. [DOI] [PubMed] [Google Scholar]
- 77. Wegrzyn J, Thoreson AR, Guyen O, Lewallen DG, An KN. Cementation of a dual-mobility acetabular component into a well-fixed metal shell during revision total hip arthroplasty: a biomechanical validation. J Orthop Res 2013;31:991–997. [DOI] [PubMed] [Google Scholar]
- 78. Emara AK, Peterson J, Piuzzi NS, et al. Effect of liner offset and inclination on cement retention strength of metal-in-metal acetabular constructs: a biomechanical study. J Orthop Res 2021;39:813–820. [DOI] [PubMed] [Google Scholar]
- 79. Chalmers BP, Ledford CK, Taunton MJ, Sierra RJ, Lewallen DG, Trousdale RT. Cementation of a dual mobility construct in recurrently dislocating and high risk patients undergoing revision total arthroplasty. J Arthroplasty 2018;33:1501–1506. [DOI] [PubMed] [Google Scholar]
- 80. Plummer DR, Christy JM, Sporer SM, Paprosky WG, Della Valle CJ. Dual-mobility articulations for patients at high risk for dislocation. J Arthroplasty 2016;31:131–135. [DOI] [PubMed] [Google Scholar]
- 81. Wegrzyn J, Saugy CA, Guyen O, Antoniadis A. Cementation of a dual mobility cup into an existing well-fixed metal shell: a reliable option to manage wear-related recurrent dislocation in patients with high surgical risk. J Arthroplasty 2020;35:2561–2566. [DOI] [PubMed] [Google Scholar]
- 82. Moreta J, Uriarte I, Foruria X, Urra I, Aguirre U, Martínez-de Los Mozos JL. Cementation of a dual-mobility cup into a well-fixed cementless shell in patients with high risk of dislocation undergoing revision total hip arthroplasty. Hip Int 2021;31:97–102. [DOI] [PubMed] [Google Scholar]
- 83. Brüggemann A, Mallmin H, Bengtsson M, Hailer NP. Safety of use of tantalum in total hip arthroplasty. J Bone Joint Surg [Am] 2020;102-A:368–374. [DOI] [PubMed] [Google Scholar]
- 84. Brüggemann A, Mallmin H, Hailer NP. Do dual-mobility cups cemented into porous tantalum shells reduce the risk of dislocation after revision surgery? Acta Orthop 2018;89:156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Shield WP, III, Greenwell PH, Chapman DM, Dalury DF. Ignore the patella in revision total knee surgery: a minimum 5-year follow-up with patella component retention. J Arthroplasty 2019;34:S262–S265. [DOI] [PubMed] [Google Scholar]
- 86. Affatato S, Castiello E, Amendola L, Comitini S, Prudhon JL, Tigani D. Revision of a monoblock metal-on-metal cup using a dual mobility component: is it a reasonable option? Materials (Basel) 2020;13:E2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Chan MK, Caudwell M, Suchowersky A, Ashton A. Femoral side-only revision options for the Birmingham resurfacing arthroplasty. ANZ J Surg 2019;89:1016–1021. [DOI] [PubMed] [Google Scholar]
- 88. Renner L, Faschingbauer M, Boettner F. Is there a rationale to use a dual mobility poly insert for failed Birmingham metal-on-metal hip replacements? A retrieval analysis. Arch Orthop Trauma Surg 2015;135:1177–1181. [DOI] [PubMed] [Google Scholar]
- 89. D’Apolito R, Bandettini G, Jacquot FMP, Zagra L. Modular dual-mobility cups using ceramic liners: an original solution for selected indications? Hip Int 2020;30:59–65. [DOI] [PubMed] [Google Scholar]
- 90. Mäkinen TJ, Abolghasemian M, Watts E, et al. Management of massive acetabular bone defects in revision arthroplasty of the hip using a reconstruction cage and porous metal augment. J Bone Joint Surg [Br] 2017;99-B:607–613. [DOI] [PubMed] [Google Scholar]
- 91. Shah A, Lee SC, Ahn HS, Ong A, Jung KA. A novel technique of reshaping the post of a constrained liner to avoid post and primary box mismatch in a case of recurrent dislocation after total knee arthroplasty. Eur J Orthop Surg Traumatol 2019;29:221–226. [DOI] [PubMed] [Google Scholar]
- 92. Stokes AP, Rutherford AD. Mismatch of modular prosthetic components in total joint arthroplasty: the New Zealand experience. Orthop Proc 2005;87-B:321. [Google Scholar]
- 93. Howard P. Hip and knee mismatches recorded in the National Joint Registry. EFORT Annual Congress. EFORT Open Rev 2018;3. [Google Scholar]
- 94. Odgaard A, Laursen MB, Gromov K, et al. Mismatch ‘never events’ in hip and knee arthroplasty: a cohort and intervention study. J Bone Joint Surg [Br] 2019;101-B:960–969. [DOI] [PubMed] [Google Scholar]
- 95. Healthcare Safety Investigation Branch (HSIB). Investigation into the implantation of wrong protheses during joint replacement surgery. 2018. https://www.hsib.org.uk/documents/40/hsib_final_report_implantation_wrong_prostheses_during_surgery.pdf (date last accessed 30 September 2021).
- 96. National Guideline Centre (UK). Evidence review for wrong implant selection: joint replacement (primary): hip, knee and shoulder. London: National Institute for Health and Care Excellence (UK), 2020. [PubMed] [Google Scholar]
- 97. Ast MP, Mayman DJ, Bostrom MP, Gonzalez Della Valle A, Haas SB. Can we avoid implant-selection errors in total joint arthroplasty? Clin Orthop Relat Res 2019;477:130–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Duijsens AW, Keizer S, Vliet-Vlieland T, Nelissen RG. Resurfacing hip prostheses revisited: failure analysis during a 16-year follow-up. Int Orthop 2005;29:224–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Calistri A, Campbell P, Van Der Straeten C, De Smet KA. Hip resurfacing arthroplasty complicated by mismatched implant components. World J Orthop 2017;8:286–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Durand-Hill M, Henckel J, Burwell M, Skinner J, Hart A. Detection of incorrect manufacturer labelling of hip components. Skeletal Radiol 2017;46:105–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Hanks GA, Foster WC, Cardea JA. Total hip arthroplasty complicated by mismatched implant sizes: report of two cases. J Arthroplasty 1986;1:279–282. [DOI] [PubMed] [Google Scholar]
- 102. Ljung P, Lidgren L, Rydholm U. Hip socket wear due to component mismatch: a case report. Acta Orthop Scand 1989;60:223–224. [DOI] [PubMed] [Google Scholar]
- 103. Whittaker RK, Hexter A, Hothi HS, et al. Component size mismatch of metal on metal hip arthroplasty: an avoidable never event. J Arthroplasty 2014;29:1629–1634. [DOI] [PubMed] [Google Scholar]
- 104. Willmann G. [Ceramic cups for hip endoprostheses. 4: never mix and match]. Biomed Tech (Berl) 1998;43:184–186. [DOI] [PubMed] [Google Scholar]
- 105. Steens W, von Foerster G, Katzer A. Severe cobalt poisoning with loss of sight after ceramic-metal pairing in a hip: a case report. Acta Orthop 2006;77:830–832. [DOI] [PubMed] [Google Scholar]
- 106. Kang BJ, Ha YC, Hwang SC, Lee YK, Koo KH. Midterm results of large diameter Biolox forte ceramic head on delta ceramic liner articulation in total hip arthroplasty. J Arthroplasty 2014;29:2412–2414. [DOI] [PubMed] [Google Scholar]
- 107. Choy WS, Cha YH, Jeon CY, Lee KS, Kim HY. A minimum ten years of follow-up of alumina head on delta liner total hip arthroplasty. J Arthroplasty 2018;33:470–476. [DOI] [PubMed] [Google Scholar]
- 108. Koper MC, Mathijssen NMC, Witt F, Morlock MM, Vehmeijer SBW. Severe wear and pseudotumor formation due to taper mismatch in a total hip arthroplasty: a case report. JBJS Case Connect 2015;5:e29. [DOI] [PubMed] [Google Scholar]
- 109. Ashkanfar A, Langton DJ, Joyce TJ. A large taper mismatch is one of the key factors behind high wear rates and failure at the taper junction of total hip replacements: a finite element wear analysis. J Mech Behav Biomed Mater 2017;69:257–266. [DOI] [PubMed] [Google Scholar]
- 110. Fallahnezhad K, Oskouei RH, Badnava H, Taylor M. An adaptive finite element simulation of fretting wear damage at the head-neck taper junction of total hip replacement: the role of taper angle mismatch. J Mech Behav Biomed Mater 2017;75:58–67. [DOI] [PubMed] [Google Scholar]
- 111. Heylen S, Foubert K, Van Haver A, Nicolai P. Effect of femoro-tibial component size mismatch on outcome in primary total knee replacement. Knee 2016;23:532–534. [DOI] [PubMed] [Google Scholar]
- 112. Berend ME, Clarke HD, Meding JB, Carter JL, Davis KE. 0019 – Femoral-tibial component size ‘mismatch’ is one factor in aseptic loosening after TKA: an analysis of 13,776 TKAs. Knee 2017;24:I. [Google Scholar]
- 113. Young SW, Clarke HD, Graves SE, Liu YL, de Steiger RN. Higher rate of revision in PFC sigma primary total knee arthroplasty with mismatch of femoro-tibial component sizes. J Arthroplasty 2015;30:813–817. [DOI] [PubMed] [Google Scholar]
- 114. Peters RM, Hiemstra JT, Zijlstra WP, Bulstra SK, Stevens M. To mix or not to mix? Medicolegal implications of mixed components in total hip arthroplasty. Acta Orthop 2020;91:624–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Koerten HK, Onderwater JJM, Koerten EWA, Bernoski FP, Nelissen RGHH. Observations at the articular surface of hip prostheses: an analytical electron microscopy study on wear and corrosion. J Biomed Mater Res 2001;54:591–596. [DOI] [PubMed] [Google Scholar]
- 116. Cales B, Stefani Y. Risks and advantages in standardization of bores and cones for heads in modular hip prostheses. J Biomed Mater Res 1998;43:62–68. [DOI] [PubMed] [Google Scholar]