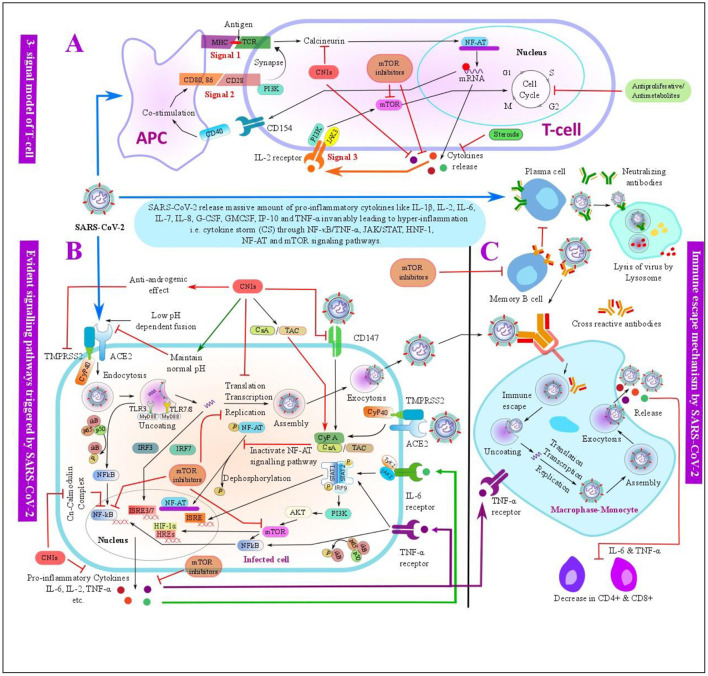
Figure 6.
Schematic overview of the evident pathways triggered by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and the possible mechanisms of immunosuppressants (ISs) used in the LT with its anti-SARS-CoV-2 effects. (A) Three-signal model of the T-cell: SARS-CoV-2 antigen is presented by an antigen-presenting cell (APC) to the T-cell by binding the major histocompatibility complex (MCH) to T-cell receptor (TCR), this further triggers the T-cell signal for an activation and proliferation of the T-cells. Costimulator molecules and its ligand bind at signal 2, which further synapse to TCR at the signal 1. The activation of signals 1 and 2 results in the release of interleukin-2 (IL-2) and other factors. The release of IL-2 further activates an IL-2 receptor on the T-cell surface, which triggers signal 3 for T-cell activation and proliferation. These signals can be inhibited by ISs such as CNIs, antiproliferative/antimetabolites, corticosteroids, and mTORis at various steps. (B) Evident pathways triggered by SARS-CoV-2 infection- SARS-CoV-2 may trigger intracellular pathways such as IFN regulatory factor-3 (IRF3), nuclear factor κB/tumor necrosis factor-α (NF-κB/TNF-α), janus kinase/signal transducers and activators of transcription (JAK/STAT), nuclear factor of activated T-cells (NF-AT), hypoxia-inducible factor 1 (HIF-1), and mammalian target of rapamycin (mTOR) signaling pathways within the infected cells, and these pathways can be targeted by the ISs -such as CNIs and mTOR used in LT at various steps. (C) Normal immune process of the monocyte-macrophage and possible immune escape mechanism of SARS-CoV-2. Post SARS-CoV-2 infection, SARS-CoV-2 spike protein is bound to the neutralizing antibodies produced by the mature plasma cells, which is then engulfed by the monocyte-macrophage and further decomposed by the lysosome present in the monocyte-macrophage as a normal immune process. SARS-CoV-2 may escape an immune system by the antibody-dependent enhancement (ADE), memory B-cells may secrete a cross-reactive antibody that may bind with SARS-CoV-2 with a weak affinity, which are further engulfed by the monocyte-macrophage. SARS-CoV-2 may get separated from the cross-reactive antibody due to a weak binding consequently leading to an immune escape and further replication and release of the virus along with other cytokines like IL-6 and TNF-α, which may advance to a cytokine storm. In addition, cytokines like IL-6 and TNF-α downregulate CD4+ and CD8+ T-cells. mTOR inhibitors can inhibit the activation of the memory B-cells and therefore downregulate the ADE process. ACE2, angiotensin-converting enzyme 2; AKT, protein kinase B; APC, antigen-presenting cell; CsA, cyclosporine A; CD, cluster of differentiation; CNI, calcineurin inhibitor; CyP, cyclophilin; G-CSF, granulocyte colony-stimulating factor; GM-CSF, granulocyte-macrophage colony-stimulating factor; HIF-1, hypoxia-inducible factor 1; HREs, hormone response elements; IFN, interferon; IgG, immunoglobulin G; IgM, immunoglobulin M; IL, interleukin; IP-10, interferon gamma-induced protein 10; IRF, IFN regulatory factor; ISRE, interferon-stimulated response element; JAK, janus kinase; MHC, major histocompatibility complex; mTOR, mammalian target of rapamycin; NF-AT, nuclear factor of activated T-cells; NF-κB, nuclear factor κB; PI3K, phosphoinositide 3-kinase; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; STAT, signal transducers and activators of transcription; TAC, tacrolimus; TCR, T-cell receptor; TLRs, toll-like receptors; TMPRSS2, transmembrane protease serine 2; TNF-α, tumor necrosis factor-α.