Figure 3.
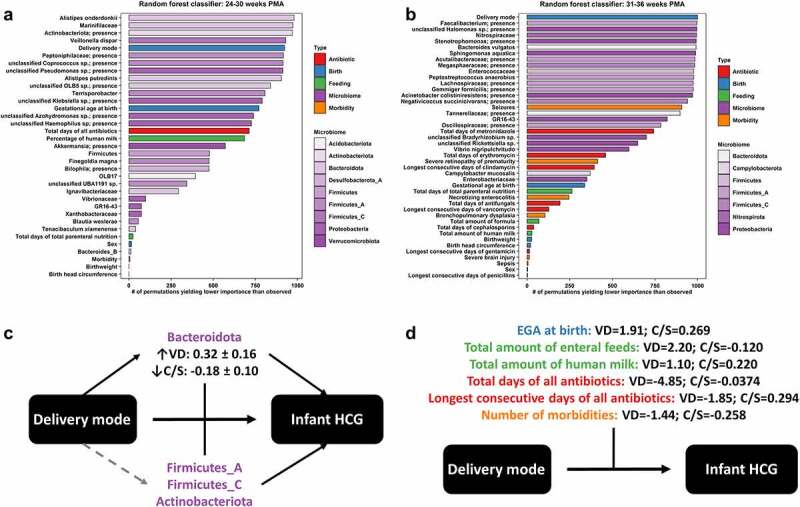
Influence of clinical factors on fecal microbiome and infant head circumference growth relationships. Random forest classifiers were built for predicting appropriate head circumference growth (HCG) trajectory versus any suboptimal HCG trajectory for infants as defined in legend for Figure 1, at the distinct key time points of 24–30 completed weeks postmenstrual age (PMA) (a) and 31–36 completed weeks PMA (b). The relative importance of features was ranked by permutation importance, or the number of permutations yielding lower importance than observed out of 1001. Fecal microbiome features (purple, with shading by bacterial phylum) out ranked most clinical factors, including antibiotics (red), birth (i.e., patient demographic) factors (blue), enteral feeding (green), and morbidity (orange). The exception to this rule was delivery mode, which was examined further by moderation analysis (c + d). Vaginal delivery (VD) significantly (solid black) increased the abundance of fecal Bacteroidota (least squares mean and standard error indicated), and the abundance of fecal Bacteroidota was both significantly directly associated with infant HCG trajectories and significantly moderated the effect of delivery mode on infant HCG trajectories (c). The abundances of other fecal microbial taxa (see Table 3) were also both significantly directly associated with infant HCG trajectories and significantly moderated the effect of delivery mode on infant HCG trajectories but were not significantly (dashed gray) increased in abundance by VD. Several clinical factors significantly moderated the effect of delivery mode on infant HCG trajectories (d); these clinical factors impacted more specifically VD infants and not Cesarean-section (C/S) delivered infants as indicated by the large differences in Cohen’s D effect sizes (appropriate/any suboptimal HCG trajectory) by delivery mode. That would explain why a significant direct effect of these clinical factors on infant HCG trajectories was mostly not observed
