Abstract
A National Academies of Sciences, Engineering, and Medicine committee developed a plan to implement high-quality primary care. One of the 5 key objectives was designing information technology that serves the patient, family, and interprofessional care team. The committee defined high-quality primary care as the provision of whole person, integrated, accessible, and equitable healthcare by interprofessional teams who are accountable for addressing most of an individual’s health across settings and through sustained relationships. The committee recommended 2 essential actions for digital health. The first action is developing the next phase of digital health certification standards that support relationship-based, continuous, person-centered care; simplify user experience; ensure equitable access; and hold vendors accountable. Second, the committee recommended adopting a comprehensive aggregate patient data system usable by any certified digital health tool. This article reviews primary care’s digital health needs and describes successful digital health for primary care.
INTRODUCTION
A new consensus report by the National Academies of Sciences, Engineering, and Medicine (NASEM) states that primary care should be a common good accessible to everyone and supported by government and private sectors.1,2 In the US, primary care provides more than one-third of all healthcare visits and more than half of outpatient visits, yet only receives 5.4% of overall healthcare spending.1 This is substantially lower than other countries.3 Primary care is the only part of the health sector with evidence for improving both health and equity, but has no federal coordinating agency, no dedicated research support, a declining workforce pipeline, and insufficient access. For primary care to be a common good, these deficiencies must be addressed.
To develop this report, a 20-member committee with transdisciplinary expertise was charged with examining the current state of primary care, building upon a 1996 Institute of Medicine report, and developing a plan to assure uptake of its recommendations.4 The committee began its work by revisiting the definition of primary care, providing a description of high-quality primary care in practice. Digital health was not included in the 1996 report, but the committee recognized the need to address it, particularly since digital health can either support or hinder high-quality primary care.
The committee identified 5 overarching objectives, each with a set of specific actions and accountable actors (Box 1). The objectives include (1) Pay for primary care teams to care for people, not doctors to deliver services; (2) Ensure that high-quality primary care is available to every individual and family in every community; (3) Train primary care teams where people live and work; (4) Design information technology that serves the patient, family, and interprofessional care team; and (5) Ensure that high-quality primary care is implemented in the US. The latter addressed the committee’s critical charge of designing an implementation plan. This article summarizes the recommendations related to information technology and describes their connection to the implementation plan; specifically, highlighting the need for measures related to digital health.
Box 1.
Five objectives for achieving high-quality primary care
| 1. Pay for primary care teams to care for people, not doctors to deliver services |
|
| 2. Ensure that high quality primary care is available to every individual and family in every community |
|
| 3. Train primary care teams where people live and work |
|
| 4. Design information technology that serves the patient, family, and interprofessional care team |
|
| 5. Ensure that high-quality primary care is implemented in the United States |
|
|
Primary care’s digital health needs
Digital health has become an essential component of healthcare. Just as primary care can be viewed as a common good,5 digital health can be viewed as a common good to support the entire healthcare system. Without highly functioning digital technologies designed to support the functions of primary care, accomplishing the aims of the NASEM report will not be possible.
Critical primary care functions, defined by Barbara Starfield’s 4 Cs of primary care, have unique digital health needs.6 First, primary care is comprehensive. Primary care clinicians focus on whole-person health. Accomplishing this requires whole-person information that could be applied to any potential health situation. Second, primary care is commonly the point of first contact. Information-seeking and data collection for new health issues often start in primary care. Third, primary care is based on a continuous longitudinal relationship. Rather than tracking episodes of care, digital health must support understanding individuals’ health trajectories as issues evolve and resolve over time. Fourth, primary care is charged with coordinating care. As a result, we rely on primary care to find, enter, and share comprehensive patient information, essentially being the curator of a patient’s electronic health record. This monumental task is not sustainable. Adding to Dr Starfield’s description, primary care is also contextual, and must integrate information from people’s daily lives into existing information systems in an automated fashion—things like social determinants of health and information from wearables or home monitoring.
When the committee considered digital health, it broadly considered use of any technology to care for individual patients and communities. Digital health tools included but were not limited to electronic health records, patient portals, mobile applications, telemedicine platforms, registries, analytic systems, remote monitoring, wearable technology, communication systems, artificial intelligence, chatbots, etc.
NASEM digital health recommendations
The fourth NASEM objective, to design information technology that serves the patient, family, and interprofessional care team, included 2 specific recommended actions. Action 4.1: Office of National Coordinator (ONC) and Centers for Medicare and Medicaid services (CMS) should develop the next phase of digital health certification standards that support relationship-based, continuous, and person-centered care; simplify the user experience; ensure equitable access and use; and hold vendors accountable.1
This approach is fundamentally different from the original 3 phases of Meaningful Use.7,8 While Meaningful Use achieved its goal of promoting the adoption and implementation of electronic health records across health settings,9,10 it fell short of driving the full range of technology advances that primary care requires.11 The committee recommends that systems align with the functions of primary care—supporting relationships; providing access and continuous contact over time; collecting and understanding each patient’s story; and having a person/patient/family-centric focus rather than a disease focus.
To demonstrate that digital health meets primary care teams’ needs, digital health systems must automatically measure user experience (eg, clicks, time spent using the system, data transferred without manual review, efficiency of care, and health outcomes), rather than asking clinicians to check boxes, conduct queries, or create reports to prove that digital health systems are effective. Primary care needs sensemaking functionality and automated tools that make the right care at the right time easy to deliver.12 These functions span a range of actions, including things like supporting the diagnostic process, enabling shared decision-making, automating documentation and delivery, and anticipating needs. Critically, for this next phase of digital health certification, the committee recommends vendors and state and national support agencies, not clinicians and health systems, be held accountable and responsible for failing to achieve benchmarks. Prior Meaningful Use certifications put significant burden on clinicians and health systems with bonuses followed by penalties.13–15
Action 4.2: ONC and CMS should plan for and adopt a comprehensive aggregate patient data system to enable primary care clinicians and interprofessional teams to easily access comprehensive patient data needed to provide whole-person care. 1 While this is a big ask, US policy makers cannot continue to allow information siloing, which leads to inefficiencies, waste, and errors.1 To be actionable, data needs to be usable by any certified digital health tool at the point of care with patients’ permission.
This action could be accomplished through 3 (or more) potential mechanisms: (1) a centralized comprehensive data warehouse, (2) patient-retained data files, such as an individual health data card, or (3) distributed sources connected by a real-time functional health information exchange. Each of these mechanisms would have unique challenges16 but, if operationalized as envisioned, would allow any clinician to instantly access all of a person’s health information, with permission, at the point of care.
Specific obstacles that would need to be addressed to enact a comprehensive aggregate patient data system include cost, coding and semantics, privacy and security, fragmented healthcare, equitable access and informatics systems, and current policies supporting digital health.17,18 While these barriers are significant, they have been overcome by other nations that have created more comprehensive health information systems.19,20
If we continue to pursue the functional health information exchange, many have called for the exchange to be designed similar to the banking exchange. Banks move money through the Society for Worldwide Interbank Financial Telecommunications messaging systems. Starting with 293 banks, now more than 11 000 banks use the system, paying membership and per-transaction fees. Similar investments would be needed to establish and sustain such a system for health data; yet healthcare invests substantially less than banking in data exhange.21–23
Complicating matters, health data is more complex than financial data. Despite advances in adopting common data models, wide variations in semantics and coding standards remain, as do free text, redundancy, and human data entry errors, which must be addressed to ensure data quality.17 Privacy and security are paramount concerns with any approach. Recent ransomware attacks on the communications, energy, financial, and healthcare sectors highlight the risk for digital health. A coordinated national approach to protect data, rather than our current reliance on health systems and vendors, would likely be more secure. Finally, we need to address the fact that patient information is a competitive advantage for both health systems and digital health vendors, and clinician and digital health vendor reimbursement models reinforce information fragmentation over interoperability.18
What does success look like?
The NASEM committee presented a vision for primary care digital health.1 The functions of effective digital health include aggregating, analyzing, and applying information for action (Figure 1).
Figure 1.
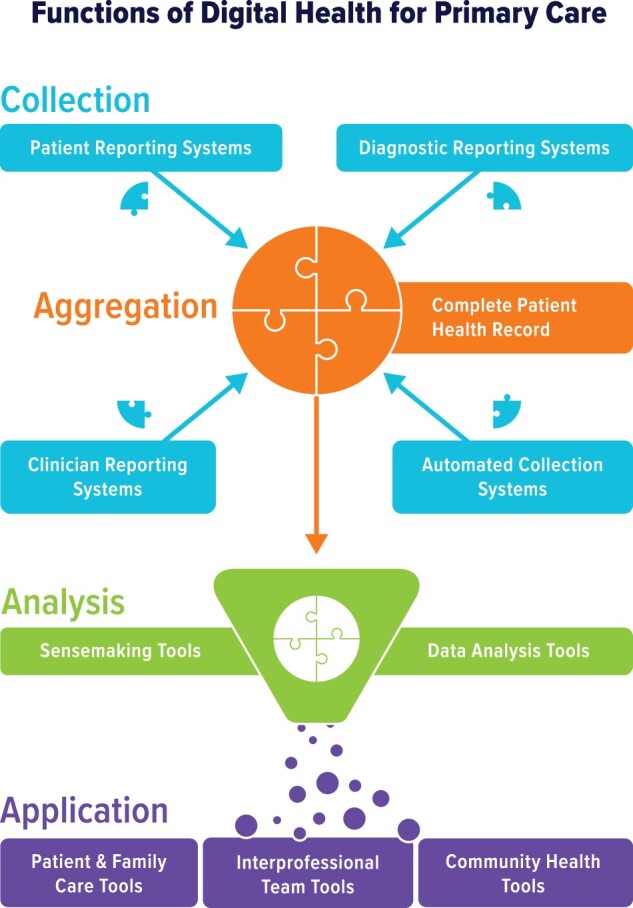
Functions of digital health for primary care.
Digital health needs to help primary care clinicians with collecting information, aggregating and analyzing information, and applying information to decision-making and clinical care. Multiple digital health tools can collect information from different audiences (patients, clinicians, diagnostic tests, and automated tools, such as wearables). Once information is aggregated, automated systems are needed to analyze the information to make it usable by patients, families, and care teams. Reprinted with permission from National Academies of Sciences Engineering and Medicine. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care.1
High-quality primary care requires automated data collection and documentation to minimize reliance on clinician data sorting and entry. Sources include clinicians (eg, care team, community partners), patients (eg, patient reported behaviors, values, needs), biometrics (eg, blood pressure, blood sugar), and other sources of information that affect health (eg, environmental data, social descriptors) from all settings (inpatient, outpatient, community). All healthcare team members need to generate and access health information. Patients, not vendors or health systems, should “own” their data and be able to grant care team members access to it.
While the comprehensive health record described in Action 4.2 is needed to inform evidence-based, whole-person care, the quantity of information can be overwhelming for users. Clinician- and patient-facing tools, such as artificial intelligence, are needed to parse relevant data, understand implications and interrelationships of data, and aid decision-making and health promotion.
Most importantly, information must be applied to care. Digital health systems must engage and activate patients and populations by translating medical content into lay language, allowing patients to state and communicate goals, and providing logic, support, and tools to facilitate their actions. Digital health systems should promote national quality and safety standards by automating the use of up-to-date guidelines and easy access to quality metric reports. Registries, alerts, reminders, and other population health tools can proactively and automatically identify persons who require care and even deliver care through artificial intelligence, chat bots, avatars, and ambient computing. Integrated communication tools can help teams better coordinate care across settings and over time.
Across the entire range of digital health functionality, systems must work with a broad range of audiences with diverse needs, particularly socially and economically marginalized and medically underserved people. Community engagement can ensure that the design and implementation of digital health helps those most in need. Mobile technology can better reach underserved populations, but infrastructure, systemic inequities, and current market forces must be addressed to truly promote equity.
Leadership, scorecard, and research
The committee made 3 overarching recommendations to ensure that the committee’s actions for implementing high-quality primary care occur. First, the committee recommended that the Department of Health and Human Services establish a Secretary’s Council on Primary Care for leadership to coordinate primary care policy, ensure adequate resources, and report progress. Coordinating digital health actions would be an important task for this council. ONC’s Recognized Coordinating Entity, charged with implementation of key interoperability provisions under Title IV of the Cures Act, can also lead in establishing the committee’s proposed comprehensive aggregate patient data system.24
The committee also proposed a scorecard to track implementation progress, success, and failures. Scorecard metrics would ideally be already in use, easily understood, built on data that is regularly collected and available, and appropriate at the state and national level. No metrics meeting these criteria currently exist for digital health, reinforcing the committee’s call to establish the next phase of digital certification. Metrics to define success should be built into the certification process. Finally, the committee highlighted the need for more research through a new Office of Primary Care Research at the National Institutes of Health and through funding investments in primary care research at the Agency for Healthcare Research and Quality. Needed research would build on the science of implementing and disseminating best practices. Robust research in digital health would be a vital component of these efforts.
CONCLUSIONS
Common goods are defined as shared and beneficial resources for all community members. They require collective action supported by policies. For primary care to achieve its desired common good status, collective action from the digital health community and policy makers is needed to create an easily accessible, equitable, and comprehensive patient record in order to ensure that digital health design truly supports the practice of primary care.
FUNDING
None.
AUTHOR CONTRIBUTIONS
AK, RP, LL, and BO were all members of the NASEM committee on Implementing High Quality Primary Care. All participated in developing the original report and recommendations from the committee. RP co-chaired the committee. AK wrote this manuscript summarizing the digital health recommendations with input and revision from all authors.
ACKNOWLEDGMENTS
We would like to thank the members of the NASEM Implementing High Quality Primary Care committee for contributing to the report and recommendations, including Asaf Bitton, Tumaini Coker, Carrie Colla, Molly Cooke, Jennifer DeVoe, Rebecca Etz, Susan Fisher-Owens, Jackson Griggs, Shawna Hudson, Shreya Kangovi, Christopher Koller, Linda McCauley, Mary McClurg, Brenda Reiss-Brennan, Hector Rodriguez, and Robert Weyant. We would also like to thank the staff at the NASEM for their leadership and support, including Marc Meisnere, Sharyl Nass, and Sarah Robinson.
DISCLAIMERS
Dr Leykum receives salary from the Department of Veterans Affairs Health Services Research and Development Service. This work does not represent the position of the Department of Veterans Affairs.
DATA AVAILABILITY
Not applicable. This article presents a consensus panel perspective.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.National Academies of Sciences Engineering and Medicine. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. National Academies Press; 2021. https://www.nationalacademies.org/our-work/implementing-high-quality-primary-care Accessed September 7, 2021. [PubMed]
- 2. Phillips RL Jr, McCauley LA, Koller CF.. Implementing high-quality primary care: a report from the national academies of sciences, engineering, and medicine. JAMA 2021; 325 (24): 2437–8. [DOI] [PubMed] [Google Scholar]
- 3.Organisation for Economic Co-operation and Development. Deriving preliminary estimates of primary care spending under the SHA 2011 framework; 2011. https://www.oecd.org/health/health-systems/Preliminary-Estimates-of-Primary-Care-Spending-under-SHA-2011-Framework.pdf Accessed September 7, 2021.
- 4. Donaldson MS, Yordy KD, Lohr KN, Vanselow NA.. Primary Care: America's Health in a New Era. Washington, DC: National Academy Press; 1996. [PubMed] [Google Scholar]
- 5. Larson EB, Roberts KB, Grumbach K.. Primary care, generalism, public good: deja vu? Again! Ann Intern Med 2005; 142 (8): 671–4. [DOI] [PubMed] [Google Scholar]
- 6. Starfield B, Shi L, Macinko J.. Contribution of primary care to health systems and health. Milbank Q 2005; 83 (3): 457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blumenthal D, Tavenner M.. The “meaningful use” regulation for electronic health records. N Engl J Med 2010; 363 (6): 501–4. [DOI] [PubMed] [Google Scholar]
- 8.The American Recovery and Reinvestment Act of 2009; 2009. http://thomas.loc.gov/cgi-bin/query/z?c111:H.R.1 Accessed September 7, 2021.
- 9. Adler-Milstein J, Jha AK.. HITECH act drove large gains in hospital electronic health record adoption. Health Aff (Millwood) 2017; 36 (8): 1416–22. [DOI] [PubMed] [Google Scholar]
- 10. Hsiao CJ, Jha AK, King J, Patel V, Furukawa MF, Mostashari F.. Office-based physicians are responding to incentives and assistance by adopting and using electronic health records. Health Aff (Millwood) 2013; 32 (8): 1470–7. [DOI] [PubMed] [Google Scholar]
- 11. Krist AH, Beasley JW, Crosson JC, et al. Electronic health record functionality needed to better support primary care. J Am Med Inform Assoc 2014; 21 (5): 764–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Campbell R. The five “rights” of clinical decision support. J AHIMA 2013; 84 (10): 42–7. quiz 48. [PubMed] [Google Scholar]
- 13.Medscape. Meaningful Use: What Is It, and Where Did It Go? https://www.medscape.com/courses/section/870105 Accessed September 7, 2021.
- 14. Fleming NS, Becker ER, Culler SD, et al. The impact of electronic health records on workflow and financial measures in primary care practices. Health Serv Res 2014; 49 (1 Pt 2): 405–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goetz Goldberg D, Kuzel AJ, Feng LB, DeShazo JP, Love LE.. EHRs in primary care practices: benefits, challenges, and successful strategies. Am J Manag Care 2012; 18 (2): e48-54–e54. [PubMed] [Google Scholar]
- 16. Donahue M, Bouhaddou O, Hsing N, et al. Veterans health information exchange: successes and challenges of nationwide interoperability. AMIA Annu Symp Proc 2018; 2018: 385–94. [PMC free article] [PubMed] [Google Scholar]
- 17. Shull JG. Digital Health and the State of Interoperable Electronic Health Records. JMIR Med Inform 2019; 7 (4): e12712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Glaser J. What Banking Can Teach Health Care About Handling Customer Data. Harvard Business Review; 2019. https://hbr.org/2019/10/what-banking-can-teach-health-care-about-handling-customer-data Accessed September 7, 2021.
- 19. Huerta JE, Villar CA, Fernandez MC, Cuenca GM, Acebedo IA. NHS Electronic Health Record System. Madrid Health Information Institute; 2018. https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/docs/HCDSNS_English.pdf Accessed September 7, 2021.
- 20. Payne TH, Lovis C, Gutteridge C, et al. Status of health information exchange: a comparison of six countries. J Glob Health 2019; 9 (2): 0204279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fedak V. Big Data Analytics in the Banking Sector; 2018. https://medium.datadriveninvestor.com/big-data-analytics-in-the-banking-sector-b7cb98d27ed2 Accessed September 7, 2021.
- 22.Big Data Investments in the Healthcare & Pharmaceutical Industry Will Account for Nearly $4.7 Billion in 2018 Alone. Research and Markets; 2018. https://www.prnewswire.com/news-releases/big-data-investments-in-the-healthcare–pharmaceutical-industry-will-account-for-nearly-4-7-billion-in-2018-alone-300688346.html Accessed September 7, 2021.
- 23.IT Spending and Staffing Benchmarks 2020/2021. Avasant Research; 2020. https://www.computereconomics.com/page.cfm?name=it-spending-and-staffing-study Accessed September 7, 2021.
- 24.Trusted Exchange Framework and Common Agreement – Recognized Coordinating Entity (RCE); 2019. HealthIT.gov. https://www.healthit.gov/topic/onc-funding-opportunities/trusted-exchange-framework-and-common-agreement-recognized Accessed September 7, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable. This article presents a consensus panel perspective.


