Abstract
This study aims to establish how pediatric fracture patterns were altered at a level 1 trauma center in a state that implemented a shutdown during the initial height of COVID-19. After IRB approval, we identified 2017 patients treated at a pediatric institution for definitive management of a fracture between 26 March and 31 May 2018, 2019, or 2020. Dates were chosen based on statewide stay-at-home orders for Colorado. Patients were excluded for treatment at another institution (n = 148), no fracture noted in clinic (n = 18), or other (n = 13). Data were retrospectively collected from the remaining 1838 patients regarding demographics, fracture injury, mechanism, and treatment. Odds ratios (ORs) were calculated for each variable during COVID-19 relative to prior years. The number of fractures during 2020 decreased by 26% relative to 2019 and 23% to 2018. A larger proportion of patients experienced at least a 5-day delay to definitive treatment [OR: 1.55, confidence interval (CI): 1.23–1.96, P = 0.0002]. Rates of non-accidental trauma (NAT) increased non-significantly (OR: 2.67, CI: 0.86–8.32, P = 0.0900) during 2020 (1.2%) relative to 2018 (0.6%) and 2019 (0.3%). Fractures occurring at home increased to 79.9% (OR: 6.44, CI: 5.04–8.22, P < 0.0001). Despite less overall trauma during shelter-in-place orders, greater fracture numbers were seen among younger children and severe fractures were likely among older children. Patients may hesitate to seek care during 2020. Rates of NAT doubled during 2020. As communities prepare for future waves, treatment centers should warn against common fracture mechanisms and raise awareness of NAT.
Keywords: COVID-19, fracture trends, non-accidental trauma during COVID-19, pediatric trauma, trauma patterns
Introduction
Fractures represent a significant portion of pediatric injuries [1]. Despite well-established trends in pediatric fracture patterns, the coronavirus disease 2019 (COVID-19) pandemic uprooted the spring and summer of 2020 that usually mark an uptick in injury rates [2,3]. Closures of schools and extracurriculars resulting from state-wide stay-at-home (SAH) orders are hypothesized to change these trends.
A recent study examining changes to the patterns of pediatric fractures presenting to a single level I trauma center during the height of the COVID-19 pandemic identified a decrease in the number of overall fractures, with a smaller proportion of these occurring due to sports, and a larger percentage occurring at home [4]. At least five other studies have noted similar changes to trauma rates during the pandemic [5–9]. These patterns have yet to be explored throughout the USA, particularly within the Rocky Mountain region where outdoor recreation and high-energy mechanism traumas are common.
Similar to prior work, this study aims to identify how trends, rates, and mechanisms of pediatric fractures were altered by the coronavirus pandemic and associated SAH/shelter-in-place (SIP) orders at a single, level I pediatric trauma center in the Western USA. Fractures are an ideal injury to study because they typically present with significant pain and are accurately and easily diagnosed using imaging [10–13]. For these reasons it is unlikely fractures will be underreported relative to other injuries. Furthermore, we examined COVID-specific concerns including delays in care and rates of non-accidental trauma (NAT) during the SAH/SIP period.
Methods
Following IRB approval, we identified 2017 patients who were referred to an outpatient orthopedic clinic at a quaternary pediatric institution with a level I trauma center for definitive management of a fracture between 26 March and 31 May 2018, 2019, or 2020. These dates were chosen based upon the start of statewide SAH orders in this state through the end of a standard public-school year. Patients were excluded for any of the following: any treatment at another institution (n = 148), no fracture noted in clinic (n = 18), or other reason (n = 13). The final population included 1838 patients treated for a fracture during this time frame.
Data were collected from each patient’s chart regarding demographics, injury mechanism/location, fracture characteristics, and treatment. Demographics included sex, ethnicity, race, age, and comorbidities (spina bifida, cerebral palsy, developmental hip dysplasia, clubfoot, genetic disorders, or neuromuscular disorders). Injury mechanism was categorized as a trampoline accident, bike/scooter/skateboard accident, ski/snowboard accident, fall from either standing height or elevation, motor vehicle crash, NAT, other impacts, or other. Injury locations included home, car, school, organized sports, or others. Fracture characteristics and treatment variables collected included: laterality, bone, open/closed fracture, open/closed reduction, operative/non-operative treatment, and date of treatment.
Finally, we noted the number of days from injury to definitive treatment in order to analyze any delay in time to care during 2020 relative to control years. A delay in care was defined as greater than five days from initial injury to definitive treatment. Five days were selected because it represents the 75th percentile for time from injury to definitive treatment across the entire study.
Statistical methods
Descriptive statistics were used to summarize demographic and injury-related characteristics. Logistic regression analyses were used to test for differences in our primary covariates, odds of NAT, fractures requiring operative treatment, and delay (>5 days) in definitive treatment during the COVID-19 time period (2020) relative to the control time periods (2018 and 2019). Logistic regression analyses were also used to test for differences in patient demographics (Table 1), injury mechanism/location (Tables 2 and 3), and fracture characteristics/treatment (Table 4). We also tested whether differences were dependent on patient age (age × time period interaction). In this analysis, we focused on the primary covariates as well as all variables that were significantly different between the time periods. Finally, a meta-analysis, meta r package, was used to combine NAT results from our study with that performed by Kovler et al. [14,15]. Figures were created to augment the primary analysis by describing temporal trends in data during all three time periods. In order to detect temporal trends, the investigated dates were divided into six, eleven-day intervals. Median values for each year were included in the figures.
Table 1.
Demographics and patient-level injury characteristics
| 2018 (n = 653) | 2019 (n = 682) | 2020 (n = 503) | Contrast: 2020 vs. 2018/2019 | OR | LCL | UCL | P value | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||||
| Female, n (%) | 268 | 41.0 | 273 | 40.0 | 208 | 41.4 | Female vs. male | 1.04 | 0.85 | 1.29 | 0.6893 |
| Comorbidity, n (%) | 13 | 2.0% | 10 | 1.5% | 9 | 1.8% | Present vs. absent | 1.04 | 0.48 | 2.26 | 0.9220 |
| Private insurance, n (%) | 291 | 44.6% | 319 | 46.8% | 239 | 47.5% | Private insurance: Y vs. N | 1.08 | 0.88 | 1.32 | 0.4849 |
| Non-english as primary language, n (%) | 611 | 93.6% | 651 | 95.5% | 490 | 97.4% | English as primary language | 2.18 | 1.20 | 3.97 | 0.0108 |
| Race, n (%) | |||||||||||
| White Hispanic or Latino Black or African American Native American or American Indian Asian/Pacific Islander More than one race Other Unknown Ethnicity, n (%) Hispanic or Latino Not Hispanic or Latino Other Unknown |
464 | 71.1 | 463 | 67.9 | 378 | 75.1 | Race: white vs. non-white | 1.33 | 1.05 | 1.68 | 0.0163 |
| 0 | 0.0 | 1 | 0.1 | 1 | 0.2 | ||||||
| 31 | 4.7 | 36 | 5.3 | 19 | 3.8 | ||||||
| 6 | 0.9 | 9 | 1.3 | 3 | 0.6 | ||||||
| 18 | 2.8 | 16 | 2.3 | 3 | 0.6 | ||||||
| 25 | 3.8 | 28 | 4.1 | 18 | 3.6 | ||||||
| 68 | 10.4 | 87 | 12.8 | 30 | 6.0 | ||||||
| 41 | 6.3 | 42 | 6.2 | 51 | 10.1 | ||||||
| 149 | 22.8 | 145 | 21.3 | 100 | 19.9 | Ethnicity: Hispanic vs. Non-Hispanic | 0.88 | 0.68 | 1.13 | 0.3187 | |
| 457 | 70.0 | 488 | 71.6 | 352 | 70.0 | ||||||
| 2 | 0.3 | 0 | 0.0 | 0 | 0.0 | ||||||
| 45 | 6.9 | 49 | 7.2 | 51 | 10.1 | ||||||
| Age at presentation, mean (SD) | 9.1 | 4 | 9.4 | 4.3 | 8.3 | 4.3 | Age per 1-year increase | 0.95 | 0.93 | 0.97 | < 0.0001 |
LCL, lower control limit; OR, odds ratio; UCL, upper control limit.
Table 2.
Mechanism of injury
| 2018 (n = 653) | 2019 (n = 682) | 2020 (n = 503) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Trampoline | 34 | 5.2 | 46 | 6.7 | 52 | 10.3 |
| Bike/scooter/skateboard | 63 | 9.7 | 79 | 11.5 | 147 | 29.2 |
| Fall from height | 173 | 26.6 | 149 | 21.8 | 84 | 16.7 |
| Fall from elevation | 86 | 13.2 | 80 | 11.7 | 43 | 8.5 |
| Impact | 86 | 13.2 | 80 | 11.7 | 43 | 8.5 |
| Unknown/other | 114 | 17.5 | 169 | 24.7 | 67 | 13.3 |
| Non-accidental trauma | 4 | 0.6 | 2 | 0.3 | 6 | 1.2 |
Table 3.
Location of injury
| 2018 (n = 653) | 2019 (n = 682) | 2020 (n = 503) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Home/family recreation | 256 | 39.2 | 254 | 37.2 | 402 | 79.9 |
| Car | 11 | 1.7 | 19 | 2.8 | 7 | 1.4 |
| School | 102 | 15.6 | 76 | 11.1 | 1 | 0.2 |
| Organized sports practice/game | 104 | 15.9 | 109 | 16.0 | 10 | 2.0 |
| Other | 68 | 10.4 | 72 | 10.6 | 27 | 5.4 |
| Unknown | 112 | 17.2 | 152 | 22.3 | 56 | 11.1 |
Table 4.
Fracture treatment patterns
| 2018 (n = 653) | 2019 (n = 682) | 2020 (n = 503) | Contrast: 2020 vs. 2018/2019 | OR | LCL | UCL | P value | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||||
| Delay >5 days in time from injury to definitive treatment, n (%) | 132 | 20.2 | 151 | 22.1 | 148 | 29.4 | Delay in treatment: yes vs. no | 1.55 | 1.23 | 1.96 | 0.0002 |
| Operative treatment | 42 | 6.4 | 51 | 7.5 | 35 | 7.0 | Operative treatment: yes vs. no | 1.00 | 0.67 | 1.49 | 0.9952 |
| Open reduction in OR, n (%) | 16 | 2.5 | 27 | 4.0 | 18 | 3.6 | Open reduction: yes vs. no | 1.12 | 0.64 | 1.95 | 0.7029 |
| Open fracture, n (%) | 9 | 1.4 | 9 | 1.3 | 7 | 1.4 | Open fracture: yes vs. no | 1.03 | 0.43 | 2.49 | 0.9426 |
| Multiple fractures, n (%) | 14 | 2.1 | 11 | 1.6 | 15 | 3.0 | Multiple Fractures: yes vs. no | 1.61 | 0.84 | 3.08 | 0.1495 |
LCL, lower control limit; OR, odds ratio; UCL, upper control limit.
Results
A total of 1838 patients met the criteria for inclusion in the study. The number of fractures in 2020 during the COVID-19 SAH orders decreased by 26% relative to the same period in 2019 and 23% relative to 2018. Overall, the distribution of demographics (Table 1), treatment patterns (Table 2), injury mechanisms (Table 3), injury location (Table 4), and injury region (Table 5) were similar during the two control years (2018 and 2019), therefore, the two control periods were combined into a single control period for all subsequent analyses.
Table 5.
Fracture by skeletal region
| 2018 (n = 653) | 2019 (n = 682) | 2020 (n = 503) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | N | % | |
| Axial fractures, n (%) | ||||||
| Skull | 0 | 0.0 | 1 | 0.1 | 0 | 0.0 |
| Facial bones | 0 | 0.0 | 0 | 0.0 | 2 | 0.4 |
| Thoracic spine | 1 | 0.2 | 0 | 0.0 | 2 | 0.4 |
| Lumbar spine | 0 | 0.0 | 1 | 0.1 | 2 | 0.4 |
| Sacrum/coccyx | 0 | 0.0 | 1 | 0.1 | 0 | 0.0 |
| Ribs | 1 | 0.2 | 0 | 0.0 | 3 | 0.6 |
| Lower extremity fractures, n (%) | ||||||
| Femur | 10 | 1.5 | 15 | 2.2 | 10 | 2.0 |
| Tibia | 36 | 5.5 | 59 | 8.7 | 45 | 8.9 |
| Fibula | 20 | 3.1 | 22 | 3.2 | 15 | 3.0 |
| Tibia and fibula | 14 | 2.1 | 11 | 1.6 | 15 | 3.0 |
| Tarsal bone(s) | 1 | 0.2 | 5 | 0.7 | 6 | 1.2 |
| Metatarsals | 21 | 3.2 | 28 | 4.1 | 11 | 2.2 |
| Phalanges | 19 | 2.9 | 19 | 2.8 | 19 | 3.8 |
| Other/multiple | 0 | 0.0 | 5 | 0.7 | 2 | 0.4 |
| Patella | 1 | 0.2 | 2 | 0.3 | 0 | 0.0 |
| Upper extremity fractures, n (%) | ||||||
| Clavicle | 41 | 6.3 | 35 | 5.1 | 27 | 5.4 |
| Scapula | 0 | 0.0 | 2 | 0.3 | 0 | 0.0 |
| Humerus | 79 | 12.1 | 78 | 11.4 | 65 | 12.9 |
| Radius | 169 | 25.9 | 172 | 25.2 | 105 | 20.9 |
| Ulna | 11 | 1.7 | 12 | 1.8 | 17 | 3.4 |
| Radius and ulna | 107 | 16.4 | 102 | 15.0 | 104 | 20.7 |
| Carpal bone(s) | 6 | 0.9 | 10 | 1.5 | 10 | 2.0 |
| Metacarpal | 26 | 4.0 | 29 | 4.3 | 16 | 3.2 |
| Phalanges | 75 | 11.5 | 69 | 10.1 | 27 | 5.4 |
| Other/multiple | 5 | 0.8 | 3 | 0.4 | 9 | 1.8 |
Primary results: severity, delay in treatment, and non-accidental trauma
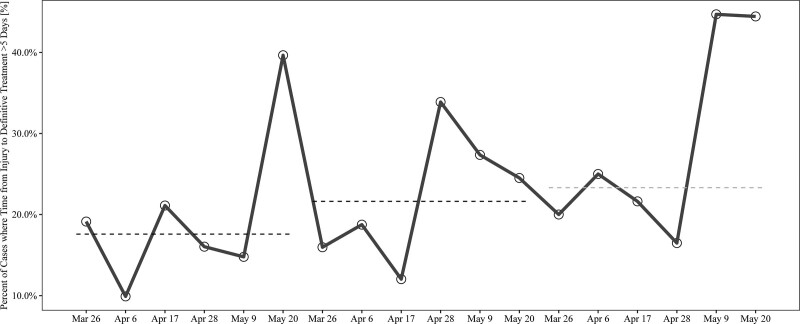
There was no significant difference in the odds of a fracture requiring operative treatment during the SAH period relative to the control [OR: 1.00, 95% confidence interval (CI): 0.67–1.49, P = 0.9952]. There was a significant increase in the proportion of patients who underwent definitive treatment greater than 5 days after their initial injury during 2020 (OR: 1.55, 95% CI: 1.23–1.96, P = 0.0002; Table 2). The relationship between delay in treatment during 2020 did not differ (P = 0.9905) between fractures treated operatively (OR: 1.56) and those treated nonoperatively (OR: 1.55). As described in Fig. 1, the proportion of patients that experienced delayed care increased towards the end of May 2020.
Fig. 1.
Percentage of fractures where time from injury to definitive treatment was >5 days. Data are summarized in 11-day intervals each year. The black lines represent median values across 2018 and 2019. The gray line represents median values across 2020. Five days was selected to define a delay as the 75th percentile for time to definitive treatment. *The final interval includes 12 days.
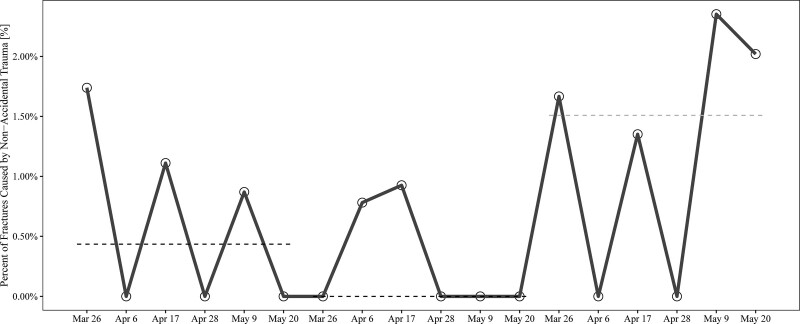
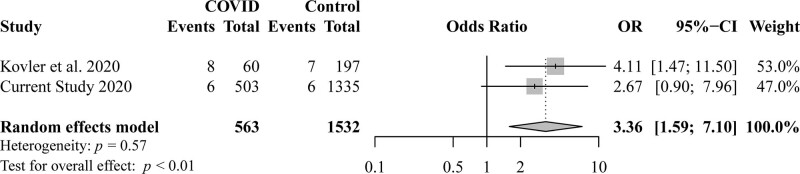
Although nonsignificant, there was an increase in the odds of a pediatric fracture occurring secondary to NAT during 2020 relative to the control (OR: 2.67, 95% CI: 0.86–8.32, P = 0.0900; Fig. 2). This observation was consistent with Kovler et al. [15], who adopted a similar research design using a trauma database. A meta-analysis was used to combine these results (Fig. 3), and the overall effect revealed a consistent increase in the occurrence of NAT during the 2020 SAH period (OR: 3.36, 95% CI: 1.59–7.10, P < 0.01).
Fig. 2.
Percentage of fractures related to non-accidental trauma (NAT). The x-axis represents time. Data are summarized in 11-day intervals within each year to identify temporal trends in the variables of interest (y) axis. Black lines represent median across intervals in 2018 and 2019, respectively. The gray line represents the median across 2020 intervals. *Final interval includes 12 days.
Fig. 3.
Meta-analysis of NAT occurrence in 2020 compared to previous two reference years. The forest plot includes the two pediatric studies on the y axis and the effect size, odds ratio representing odd of NAT during 2020 relative to the two prior years, on the x-axis. NAT, non-accidental trauma.
Patient demographics
Patients presenting during the SAH orders in 2020 were significantly more likely to identify their race as white and speak English as a primary language compared to the prior 2 years (Table 1). Patients presenting in 2020 were also significantly younger (Table 1).
Injury mechanism and location
During COVID-19 SAH orders, injuries were more likely to occur at home (OR: 6.44, 95% CI: 5.04–8.22, P < 0.0001) and involve trampolines, bikes, or scooters (OR: 3.47, 95% CI: 2.68–4.50, P < 0.0001) (Table 2). There was a significant decrease in the odds of fracture occurring during an organized sport during 2020 relative to prior years (OR: 0.11, 95% CI: 0.06–0.20, P < 0.0001).
Fracture characteristics and treatment
There was no significant difference in variables reflecting fracture severity in 2020 relative to the control years including need for open reduction, presence of an open fracture and presence of multiple fractures (Table 4). In all three years, fractures most commonly occurred in the upper extremity with 79.4% (n = 516), 74.9% (n = 513), and 74.8% (n = 376) in 2018, 2019, and 2020 respectively. The most commonly fractured bone in all years was the radius with isolated fractures at 26.0% (n = 169), 25.1% (n = 172), and 20.9% (n = 105) in 2018, 2019, and 2020 respectively. There was no significant shift in upper extremity fractures (OR: 0.87, 95% CI: 0.69, 95% CI: 0.69–1.11, P = 0.2558), lower extremity fractures (OR: 1.14, 95% CI: 0.90–1.46, P = 0.2778), and axial/pelvic fractures (OR: 2.06, 95% CI: 0.90–4.74, P = 0.0874).
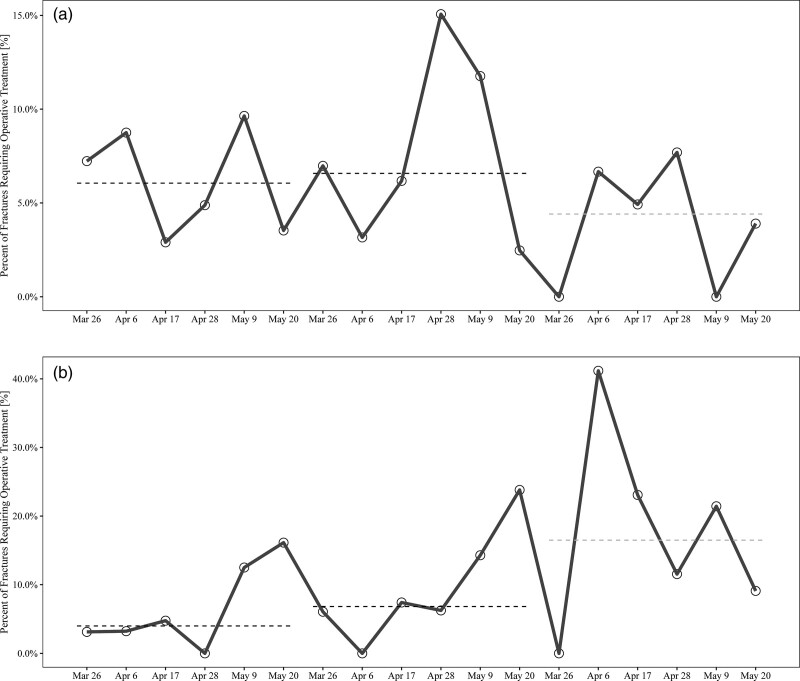
Age-related heterogeneity
We also tested whether the COVID SAH orders in 2020 had a differential effect on older versus younger children (age × time period interaction). In this analysis, we focused on the primary covariates as well as all variables that significantly differed between 2020 and the control period. We did not test NAT in this analysis because NAT injuries were only documented in younger children during both time periods (age range among NAT fractures: 0.1–3.7 years). There was no significant association between age- and sport-related fractures (P = 0.5962), trampoline-related fractures (P = 0.1226), primary language (P = 0.8249), race (P = 0.5591), or delay in treatment (P = 0.2749). There was significant age-related heterogeneity in the magnitude of the change in the following variables during 2020 relative to the control years: occurrence of an injury at home (P = 0.0004), bike/scooter related injures (P = 0.0050), and the need for operative treatment (P = 0.0246). This indicates that age modified the association between the 2020 period and these variables. Home injuries and bike injuries increased to a significantly greater degree in older subjects compared to younger subjects in 2020 (Table 6). Similarly, the need for operative treatment in 2020 relative to the control years was significantly higher in older compared to younger subjects (Table 6 and Fig. 4a vs. Fig. 4b).
Table 6.
Age-related heterogeneity in location and severity of injuries
| Contrasta | OR | LCL | UCL | P value |
|---|---|---|---|---|
| Fracture occurring at home | ||||
| Odds of home fracture: 2-year-old | 2.93 | 1.79 | 4.79 | < 0.0001 |
| Odds of home fracture: 10-year-old | 7.14 | 5.52 | 9.23 | < 0.0001 |
| Odds of home fracture: 16-year-old | 13.93 | 8.52 | 22.78 | < 0.0001 |
| Fracture involving bike/scooter mechanism of injury | ||||
| Odds of bike fracture: 2-year-old | 1.56 | 0.74 | 3.25 | 0.2402 |
| Odds of bike fracture: 10-year-old | 4.07 | 3.10 | 5.34 | < 0.0001 |
| Odds of bike fracture: 16-year-old | 8.38 | 4.84 | 14.52 | < 0.0001 |
| Fracture requiring reduction | ||||
| Odds of surgery: 2-year-old | 0.47 | 0.20 | 1.10 | 0.0811 |
| Odds of surgery: 10-year-old | 1.08 | 0.72 | 1.62 | 0.7261 |
| Odds of surgery: 16-year-old | 2.00 | 1.04 | 3.88 | 0.0390 |
LCL, lower control limit; OR, odds ratio; UCL, upper control limit.
ORs interpreted as change in odds of the exposure variable (location, mechanism, or need for surgery) during 2020 relative to odds of exposure variable during the control years for a subject of a given age (2-year-old, 10-year-old, or 16-year-old). ORs demonstrate greater effect of 2020 on older subjects relative to younger subjects.
Fig. 4.
Percentage of fractures requiring operative treatment among younger (a) vs. older individuals (b). Data are summarized in 11-day intervals. Black lines represent median values across 2018 and 2019. The gray line represents median values across 2020. Older subjects are defined as >9.4 years (75th percentile) and younger subjects are defined as those who were <9.4 years at initial injury. *Final interval includes 12 days.
Discussion
This study highlights the impact that COVID-19 and associated SAH/SIP orders had on pediatric fracture patterns at a single institution in the Western USA. Between 26 March and 31 May 2020, there were significantly fewer patients presenting with fractures compared to the same timeframe in the prior years, however, 2020 saw a greater proportion of fractures caused by high energy mechanism injuries such as trampoline or bike accidents. Due to the widespread SAH orders and early closures of ski resorts, none of these injuries were due to snow sport accidents [16]. This lack of injuries may account for some of the decline in overall fracture numbers seen during 2020. Similar to previous years, the most commonly fractured bone was the radius, but in 2020 there was an increase in rates of both bone forearm fractures, which is consistent with the increase of high energy mechanisms [1,2,17–20]. There were significant increases in the percentage of fractures resulting from scooter, bicycle, skateboard, and trampoline accidents. Interestingly, the patients that presented in 2020 also had a lower average age than those in 2018 and 2019.
Parental fear of COVID-19 exposure at a hospital may have caused hesitation to seek treatment during 2020. Hospitals are generally viewed as high-risk settings for communicable disease and this study supports the possibility of a societal aversion to hospital-based care during an international pandemic by identifying a delay to definitive treatment in 2020 [21]. A higher percentage of patients had more than a 5-day delay from injury to definitive care in our outpatient orthopedic clinic during 2020 relative to the control time frame. This delay was noted regardless of need for operative treatment, indicating one possible cause for this delay is parental hesitation to treatment at a hospital setting, rather than operating room availability secondary to pandemic-related clinical and surgical cutbacks. Hospitals and institutions began limiting clinic and surgery volumes and implemented a required COVID-19 test prior to any procedure potentially further delaying definitive management, particularly when COVID-19 testing was limited. A delay to treatment also brings into question whether there was adequate availability of orthopedists during the initial peak of COVID-19 when many surgical cases were canceled or delayed, and specialized physicians were recruited to assist in medical units. While the delay noted in the 2020 cohort could be due to patient hesitation, surgeon availability, or required COVID-19 testing, it is unknown what the cause is.
One unfortunate consequence of increased time at home for younger children instead of school, daycare, or extra-curricular activities, is an increase in injuries secondary to NAT and other sequelae of volatile home life. Increased time at home as well as increased stress, for both children and guardians, have been shown to be associated with higher rates of child abuse in all forms [22–24]. This, in combination with removing the daily observations of trained specialists such as teachers, nurses, and coaches, puts children at increased risk for abuse [25,26]. NAT is confirmed in only about 1–2% of cases despite the true quantity of children affected by abuse likely being much higher [27]. While not statistically significant, this study showed an increase in fractures secondary to NAT in 2020 during the SAH period. Kovler et al. (2020) [15] conducted a similar study and also identified an increase in percentage of NAT relative to all trauma cases secondary to COVID-19 SAH orders. When taken in conjunction with the study by Kovler et al. [15], the increase in NAT during this time period should be interpreted as a clinically and statistically significant finding, as described by our meta-analysis of the two data sets (Fig. 3). There are strong indications that instances of NAT have become increasingly prevalent during COVID-19 SAH orders. Wong et al. discuss various strategies to prevent child abuse during COVID-19 among at-risk children, including those with behavioral health needs and supports, children in foster families, and children requiring individualized medical care [28]. These strategies include frequent telehealth visits with counselors, care team members and family and friends, informational resources, healthcare resources, and alternative outlets for stress for both children and guardians [28]. Further, during periods of increased stress such as COVID-19, nationally established abuse awareness campaigns such as Pinwheels for Prevention, Period of PURPLE Crying, and the prevention and intervention programs offered by the National Children’s Advocacy Center become more important than ever [29–32]. Awareness and advocacy are often underutilized tools to prevent these incidents in children. As schools transition to primarily virtual learning during SAH orders, NAT should be strongly considered by healthcare providers when treating pediatric fractures, especially those in high-risk populations [15].
There was a decrease in the average age of patients seeking care in 2020. Despite this larger overall burden on younger children, older children were more likely to sustain a high energy fracture secondary to a trampoline or bike accident and more likely to require operative treatment. The decreased average age of children presenting with fractures in 2020 can be explained in part by the increase in injuries in the home. In prior years, younger children and toddlers would typically be in some form of school or daycare. Removing younger children from this supervised environment and placing them in a possibly less controlled home environment, particularly when parents and caregivers are juggling other responsibilities such as work, may increase their risk of injury resulting in fracture compared to prior years [33]. Younger children are also less likely to be participating in sports than their older counterparts as the average age at which children enter organized sports is about 6–8 years old [34]. Thus, it follows that older children’s overall risk of fracture may have remained neutral, or even decreased, due to the removal of a potentially risky extracurricular activity When older children participate in unsupervised recreation at home, however, they are likely more prone to a severe fracture requiring operative treatment if they do inevitably incur an injury.
Many of the changes seen in 2020 are likely to be explained by one expected consequence of SAH orders: the increase in injuries occurring at home compared to prior years. At the initial height of the coronavirus pandemic (22 April 2020), more than 83% of learners worldwide were affected by closures of schools and organized sports [35]. From March to May 2020, schools were not yet as prepared for virtual education as they were entering the school year in Fall of 2020 [35]. Thus, at that early point, many of these children were at home with no virtual schoolwork, allowing more time for recreation. While waiting for education systems to catch up with virtual learning demands, parents struggled to find sources of supervision and entertainment for their children. Compared to organized sports programs and schools where safeguards, supervision, and often medical interventions are in place, children at home may be unsupervised and have access to recreational equipment that can be risky when misused [33]. Human-powered and motorized vehicles such as bicycles, scooters, and skateboards are particularly prevalent mechanisms of injury among pediatric patients and in this study. Growing instances of these mechanisms are likely due in part to the recent surge of e-scooter/bicycle sharing apps, and their subsequent increased availability to a broader population [33,36,37]. Trampolines are another frequent source of high-energy fractures among children. Both local and global news sources reported increased sales and resulting trampoline shortages throughout the spring and early summer of 2020 [38–41]. The increased time for recreation in combination with the accessibility of these common sources of injury may begin to explain the increase in high-energy injury mechanisms seen in 2020.
Limitations
The findings in this study may not be generalizable to other regions of the USA or the world. Despite the global nature of COVID-19, SAH orders are expected to have regional implications and it is unknown how different areas will react to SAH/SIP orders secondary to COVID-19. This study may be biased for high energy injuries as patients were selected from an institution with a level I trauma status. Given this status, patients with more severe injuries have a higher likelihood of presenting or being transferred to this institution. This possible bias is less significant, however, because we are comparing within a single institution. This study is also limited to collecting data only from patients seeking care. We were unable to account for patients who chose not to receive care due to pandemic-related hesitation or went to a PCP, urgent care, or other facility for care. Another final of this study is the small sample size in which to analyze NAT. Providers may have been more sensitive to the possibility of NAT during 2020, identifying instances that may have gone overlooked in previous years.
Conclusion
Despite lower rates of trauma during the SAH/SIP orders, greater fracture numbers were seen among younger children at home and older children were more likely to sustain a severe injury requiring aggressive treatment. During 2020 patients were more likely to experience a 5-day delay to definitive treatment. This is especially concerning given that greater numbers of fractures were seen from high-energy mechanisms such as trampoline, scooter, skateboarding, and bicycle accidents. As pandemic response measures continue, orthopedic treatment centers should educate patients and guardians regarding common fracture mechanisms, be prepared to treat high-energy injuries, and continue to consider the possibility of NAT, particularly in vulnerable populations.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hedström EM, Svensson O, Bergström U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop 2010; 81:148–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Randsborg PH, Gulbrandsen P, Saltytė Benth J, Sivertsen EA, Hammer OL, Fuglesang HF, Arøen A. Fractures in children: epidemiology and activity-specific fracture rates. J Bone Joint Surg Am 2013; 95:e42. [DOI] [PubMed] [Google Scholar]
- 3.Mathison DJ, Agrawal D. An update on the epidemiology of pediatric fractures. Pediatr Emerg Care 2010; 26:594–603. [DOI] [PubMed] [Google Scholar]
- 4.Bram JT, Johnson MA, Magee LC, Mehta NN, Fazal FZ, Baldwin KD, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop 2020; 40:373–379. [DOI] [PubMed] [Google Scholar]
- 5.Fahy S, Moore J, Kelly M, Flannery O, Kenny P. Analysing the variation in volume and nature of trauma presentations during COVID-19 lockdown in Ireland. Bone Jt Open 2020; 1:261–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hernigou J, Morel X, Callewier A, Bath O, Hernigou P. Staying home during “COVID-19” decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty eight children and the “tsunami of recommendations” could not lockdown twelve elective operations. Int Orthop 2020; 44:1473–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sugand K, Park C, Morgan C, Dyke R, Aframian A, Hulme A, et al. Impact of the COVID-19 pandemic on paediatric orthopaedic trauma workload in central London: a multi-centre longitudinal observational study over the “golden weeks”. Acta Orthop 2020; 91:633–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sheridan GA, Nagle M, Russell S, Varghese S, O'Loughlin PF, Boran S, et al. Pediatric trauma and the COVID-19 pandemic: a 12-year comparison in a level-1 trauma center. HSS J ® 2020; 16(S1):92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nabian MH, Vosoughi F, Najafi F, Khabiri SS, Nafisi M, Veisi J, et al. Epidemiological pattern of pediatric trauma in COVID-19 outbreak: data from a tertiary trauma center in Iran. Injury 2020; 51:2811–2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gourde J, Damian FJ. ED fracture pain management in children. J Emerg Nurs 2012; 38:91–97. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell SAT, Majuta LA, Mantyh PW. New insights in understanding and treating bone fracture pain. Curr Osteoporos Rep 2018; 16:325–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alves CJ, Neto E, Sousa DM, Leitão L, Vasconcelos DM, Ribeiro-Silva M, et al. Fracture pain-Traveling unknown pathways. Bone 2016; 85:107–114. [DOI] [PubMed] [Google Scholar]
- 13.Augat P, Morgan EF, Lujan TJ, MacGillivray TJ, Cheung WH. Imaging techniques for the assessment of fracture repair. Injury 2014; 45 (Suppl 2):S16–S22. [DOI] [PubMed] [Google Scholar]
- 14.Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 2019; 22:153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kovler ML, Ziegfeld S, Ryan LM, Goldstein MA, Gardner R, Garcia AV, Nasr IW. Increased proportion of physical child abuse injuries at a level I pediatric trauma center during the Covid-19 pandemic. Child Abuse Negl 2021; 116:104756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer J. Colorado extends mandatory ski area closures into early April. [The Denver Post Web site]. 2020. https://theknow.denverpost.com/2020/03/19/colorado-ski-resorts-still-closed-coronavirus/235736/. [Accessed 3 December 2020].
- 17.Naranje SM, Erali RA, Warner WC, Jr, Sawyer JR, Kelly DM. Epidemiology of pediatric fractures presenting to Emergency Departments in the United States. J Pediatr Orthop 2016; 36:e45–e48. [DOI] [PubMed] [Google Scholar]
- 18.Lempesis V, Rosengren BE, Nilsson JÅ, Landin L, Tiderius CJ, Karlsson MK. Time trends in pediatric fracture incidence in Sweden during the period 1950-2006. Acta Orthop 2017; 88:440–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valerio G, Gallè F, Mancusi C, Di Onofrio V, Colapietro M, Guida P, Liguori G. Pattern of fractures across pediatric age groups: analysis of individual and lifestyle factors. BMC Public Health 2010; 10:656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kopjar B, Wickizer TM. Fractures among children: incidence and impact on daily activities. Inj Prev 1998; 4:194–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ciacchini B, Tonioli F, Marciano C, Faticato MG, Borali E, Pini Prato A, Felici E. Reluctance to seek pediatric care during the COVID-19 pandemic and the risks of delayed diagnosis. Ital J Pediatr 2020; 46:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berger RP, Fromkin JB, Stutz H, Makoroff K, Scribano PV, Feldman K, et al. Abusive head trauma during a time of increased unemployment: a multicenter analysis. Pediatrics 2011; 128:637–643. [DOI] [PubMed] [Google Scholar]
- 23.Keenan HT, Marshall SW, Nocera MA, Runyan DK. Increased incidence of inflicted traumatic brain injury in children after a natural disaster. Am J Prev Med 2004; 26:189–193. [DOI] [PubMed] [Google Scholar]
- 24.Feltman DM, Moore GP, Beck AF, Siffermann E, Bellieni C, Lantos J. Seeking normalcy as the curve flattens: ethical considerations for pediatricians managing collateral damage of coronavirus disease-2019. J Pediatr 2020; 225:233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jordan KS, MacKay P, Woods SJ. Child maltreatment: optimizing recognition and reporting by School Nurses. NASN Sch Nurse 2017; 32:192–199. [DOI] [PubMed] [Google Scholar]
- 26.Walsh K, Bridgstock R, Farrell A, Rassafiani M, Schweitzer R. Case, teacher and school characteristics influencing teachers’ detection and reporting of child physical abuse and neglect: results from an Australian survey. Child Abuse Negl 2008; 32:983–993. [DOI] [PubMed] [Google Scholar]
- 27.Pomeranz ES. Child abuse and conditions that mimic it. Pediatr Clin North Am 2018; 65:1135–1150. [DOI] [PubMed] [Google Scholar]
- 28.Wong CA, Ming D, Maslow G, Gifford EJ. Mitigating the impacts of the COVID-19 pandemic response on at-risk children. Pediatrics 2020; 146:e20200973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Child Physical Abuse Prevention. [Prevent Child Abuse America Web site]. 2020. preventchildabuse.org/what-we-do/child-physical-abuse-prevention. [Accessed 26 February 2021].
- 30.Pinwheels for Prevention. [Prevent Child Abuse America Web site]. 2021. preventchildabuse.org/resources/pinwheels-for-prevention/. [Accessed 26 February 2021].
- 31.Syndrome NCoSB. Period of PURPLE Crying Program. [National Center on Shaken Baby Syndrome Web site]. dontshake.org/purple-crying. [Accessed 26 February 2021].
- 32.NCAC. About Child Abuse. [National Children’s Advocacy Center Web site]. 2020. https://www.nationalcac.org/about-child-abuse/. [Accessed 2 March 2021].
- 33.Notrica DM, Sayrs LW, Kirsch L, Kelly C, Nickoles T, Greenberg J, et al. Inflicted versus unintentional injury: towards improved detection and surveillance of supervisory neglect. J Pediatr Surg 2020; 55:341–345. [DOI] [PubMed] [Google Scholar]
- 34.Logan K, Cuff S; Council On Sports Medicine And Fitness. Organized sports for children, preadolescents, and adolescents. Pediatrics 2019e20190997. [DOI] [PubMed] [Google Scholar]
- 35.UNESCO. “Education: From Disruption to Recovery”. [UNESCO Web site]. https://en.unesco.org/covid19/educationresponse. [Accessed 8 September 2020].
- 36.Kobayashi LM, Williams E, Brown CV, Emigh BJ, Bansal V, Badiee J, et al. The e-merging e-pidemic of e-scooters. Trauma Surg Acute Care Open 2019; 4:e000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Griffin R, Parks CT, Rue LW, III, McGwin G., Jr. Comparison of severe injuries between powered and nonpowered scooters among children aged 2 to 12 in the United States. Ambul Pediatr 2008; 8:379–382. [DOI] [PubMed] [Google Scholar]
- 38.Herrman J. The New Panic Buys: Kayaks, Pools, Tents and Trampolines. 2020.The New York Times; [Google Scholar]
- 39.Richards A. Trampoline shortage hits Australia as COVID-19 impacts Chinese manufacturers. [ABC Goldfields-Esperance Web site]. 2020. https://www.abc.net.au/news/2020-04-30/trampoline-shortage-hits-australia-due-to-covid-19/12193474. [Accessed 2 December 2020].
- 40.King A. Having a hard time finding a pool, hot tub, or trampoline to buy? Here’s why. [CBC News Web site]. 2020. https://www.cbc.ca/news/canada/toronto/pools-hottubs-trampolines-covid-19-1.5605455. [Accessed 2 December 2020].
- 41.Peres J. Trampolines, playgrounds sell out as parents try to occupy kids. [Denver Channel Web site]. 2020. https://www.thedenverchannel.com/news/national/coronavirus/trampolines-playgrounds-sell-out-as-parents-try-to-occupy-kids. [Accessed 2 December 2020].