Abstract
Objective:
(1) To determine the effect of bimaxillary orthognathic surgery on pharyngeal airway, hyoid bone, and craniocervical posture in Class III bimaxillary surgery patients. (2) To evaluate short-term and long-term results. (3) To compare short- and long-term values.
Materials and Methods:
Twenty-six Class III adult patients treated with bimaxillary surgery were included in the study. Cephalometric records were taken before treatment (T1), before surgery (T2), and 5 months (T3), 1.4 years (T4), 3 years (T5), and 5 years (T6) postsurgery.
Results:
No significant differences were identified in craniocervical angulation between time intervals. There was a significant superior movement of hyoid bone at postsurgery (T3; P < .05); however, adaptation occurred to the normal position in the long term. A nonsignificant decrease occurred at the oropharyngeal middle pharyngeal distance parameter; however, this was compensated with a significant increase between T5 and T6 (P < .001). A significant decrease was observed in the hypopharyngeal Go-P parameter between T3 and T1 (P < .01), but it recovered with a nonsignificant increase in the long term. A significant increase in nasopharyngeal area was observed between T3 and T1 (P < .05). The hypopharyngeal area significantly increased between T5 and T6, and PNS-R significantly increased between T3 and T1 (P < .05).
Conclusion:
The pharyngeal areas adversely affected after surgery recover at long-term follow-up; thus, adaptation occurs after bimaxillary surgery.
Keywords: Bimaxillary surgery, Airway, Long-term, Class III
INTRODUCTION
Combined orthodontic and orthognathic surgical treatment has become a common treatment modality for the correction of facial deformities. An important aspect of orthognathic surgery is the effect of skeletal movements and changes in the position of hyoid bone, tongue, soft palate, and posture (thus, pharyngeal airway).
The pharyngeal upper airway has attracted much attention because snoring and sleep apnea are known to be closely associated with its volume. Many authors have reported a decrease in airway dimensions after Class III orthognathic surgery1–11 and, accordingly, extension of the head posture.5,12–14 In some studies, posterior and inferior movement of the hyoid bone was detected after surgery in the short term2,6,15,16,17; however, this movement returned to its original position in the long term.2,4,5,11,17–19
Some studies have shown that with time, physiologic adaptation of the soft tissues occur and the airway is restored to its original position.7,10,11 However, Eggensperger et al.15 reported that the pharyngeal airway narrowed immediately after surgery in patients with mandibular set back, and it did so consistently during the 12-year follow-up period.
In bimaxillary surgery patients, the decrease in the pharyngeal airway is found to be significant and milder when compared with mandibular set-back surgeries.8,9,20 The long-term effects of bimaxillary operations on the pharyngeal airway have been evaluated in a few studies.7,21,22 However, those studies differ in materials and methodologies and thus can be interpreted differently. The aim of our study was to assess the pharyngeal airway, hyoid bone, and cervical posture in the short and long term after bimaxillary surgery in Class III patients by comparing the hard tissue changes and results between time periods.
MATERIALS AND METHODS
The subjects of this study were selected among the patients treated at the University of Ankara, Faculty of Dentistry, Department of Orthodontics and Maxillofacial Surgery, between 1998 and 2011. The material consisted of lateral cephalometric films of Class III orthognathic surgery patients. Inclusion criteria were nonsyndromic adult patients older than 17 years with skeletal Class III (ANB less than −4°) and dental Class III deformity, surgical treatment consisting of bimaxillary surgery without mandible border recontouring, and lateral cephalograms of good quality. Exclusion criteria included previous orthognathic surgery, genioplasty, obstructive sleep apnea, cleft, and craniofacial anomalies. Institutional Ethical Board approval was obtained to conduct this study and patient consent from each patient were received.
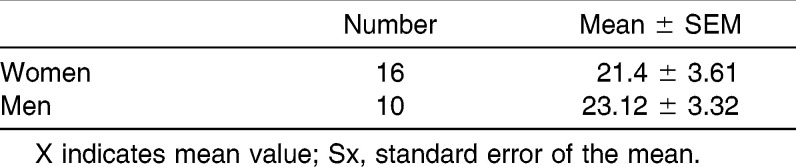
The material consisted of 26 adult patients (between 17 and 29 years). All of the patients were treated orthodontically and surgically with the same doctor and treatment protocol. The mean year of patients according to gender at pretreatment evaluation is shown in Table 1. Bilateral sagittal split ramus osteotomy with semi-rigid fixation and Le Fort I osteotomy with rigid fixation were used for the mandible and maxilla. In the Le Fort I surgical technique, the maxilla was positioned upward when needed.
Table 1.
Mean Year and Number of Subjects at Pretreatment Evaluation
The lateral cephalometric films taken at different treatment and retention phases were used for the study. The patients existing presurgery but with missing pretreatment films or patients existing pretreatment but with missing presurgery cephalometric films were also included in the study. The number of lateral cephalometric films used at different time periods are as follows:
T1: pretreatment radiograph (n = 24)
T2: presurgery radiograph (n = 25)
T3: postsurgery radiograph (n = 11)
T4: posttreatment radiograph (at the end of the fixed treatment; n = 26)
T5: first retention radiograph (n = 24)
T6: second retention radiograph (n = 9)
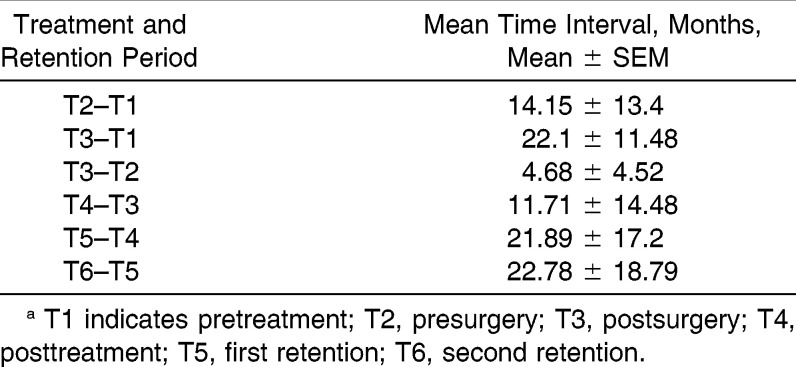
The time intervals between treatment and retention periods are shown in Table 2.
Table 2.
Time Intervals Between the Cephalometric Films Taken at Different Treatment and Retention Periodsa
Cephalometric Analysis
The lateral cephalometric radiographs were taken by the same operator on the same machine under standardized conditions in the natural head position with the mandible in centric relation; patients were informed not to swallow during radiography. Lateral cephalograms were traced and cephalometric reference points were determined by using acetate paper. Seven degrees to the sella nasion plane through the sella point was taken as the horizontal reference plane, and perpendicular to the horizontal reference plane through the S point was taken as the vertical reference plane (Figure 1). These reference planes were used as the guides in measuring the projected distances of the reference landmarks (Figure 1). Ten skeletal and dental (Figure 1), seven craniocervical and hyoidal (Figure 2), seven pharyngeal linear (Figure 3), and three pharyngeal area (Figure 4) measurements were used in the study. Linear and angular measurements were done with the help of PorDios (Purpose on Request Digitizer Input Out-put System, trademark of the Institute of Orthodontic Computer Science, Aarhus, Denmark) cephalometric analysis program. Area measurements of the pharyngeal airway were done with a digital planimeter (Ushikata X-Plan380Dııı/460Dııı, Tokyo, Japan; Figure 5a,b). The pharyngeal airway measurements were chosen similar to the investigations done previously.9,23,24
Figure 1.
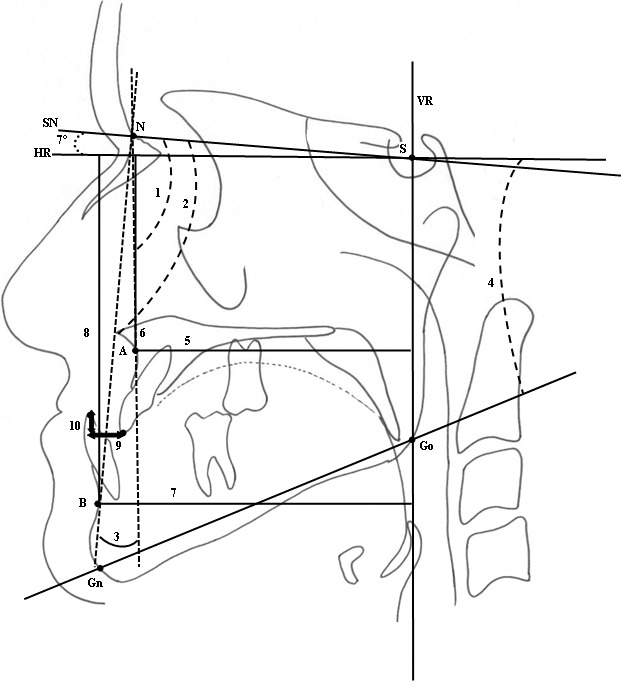
Skeletal measurements. (1) SNA. (2) SNB. (3) ANB. (4) GoGnSN. (5) A-VR. (6) A-HR. (7) B-VR. (8) B-HR. Dental measurements. (9) Overjet. (10) Overbite.
Figure 2.
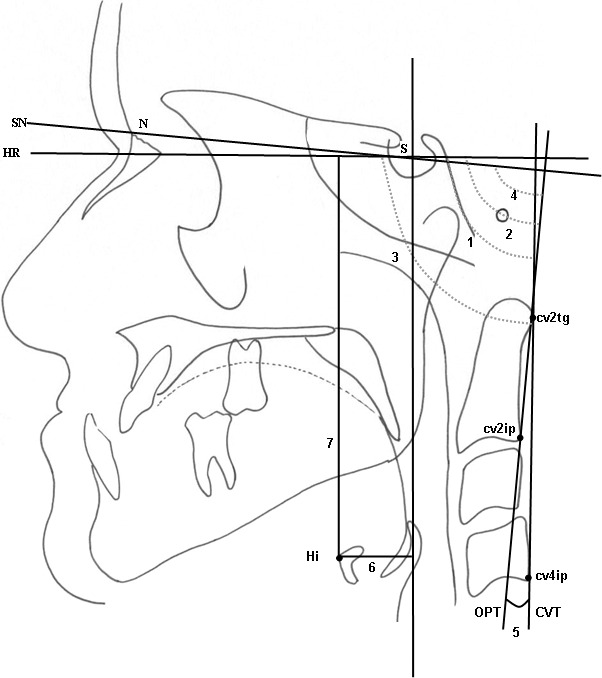
Craniocervical and hyoidal measurements. (1) SN.OPT. (2) SN.CVT. (3) OPT.HR. (4) CVT.HR. (5) OPT.CVT. (6) Hi-VR. (7) Hi-HR.
Figure 3.
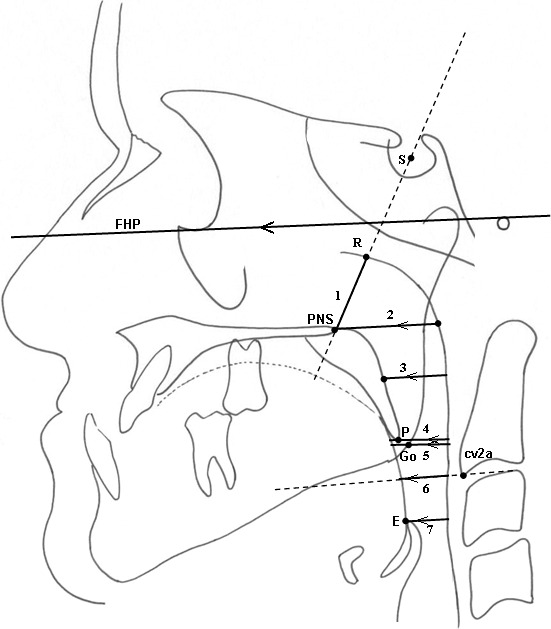
Pharyngeal linear measurements. (1) PNS-R: on the line passing from PNS and R. (2) PPS: palatal pharyngeal distance: on the line passing from PNS, parallel to FHP. (3) SPSS, superior posterior pharyngeal distance: on the line passing from the midpoint of the soft palate, parallel to FHP. (4) MPS, middle pharyngeal distance: on the line passing from P, parallel to FHP. (5) Go-P, gonial pharyngeal distance: on the line passing from Go, parallel to FHP. (6) IPS, inferior pharyngeal distance: on the line passing from cv2a, parallel to FHP. (7) EPS, epiglottic pharyngeal distance: on the line passing from E, parallel to FHP.
Figure 4.
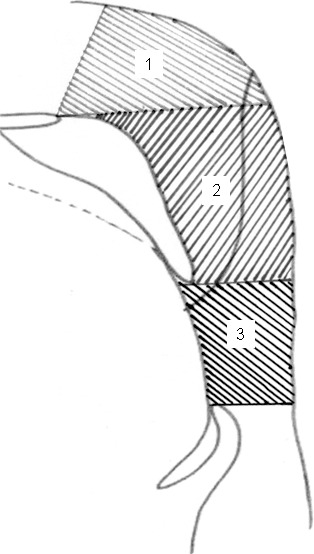
Pharyngeal area measurements. (1) Nasopharynx. (2) Oropharynx. (3) Hypopharynx.
Figure 5.
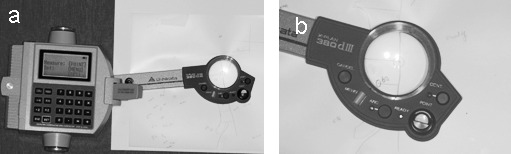
(a) Digital planimeter. (b) Measurement of the areas using a digital planimeter.
Statistical Analysis
The mean values and standard error of the means at each time interval were calculated. To determine the differences between the periods T2–T1, T3–T1, T3–T2, T4–T3, T5–T4, and T6–T5, a paired t-test was used.
Error Study
All digitizing points and measurements were repeated on 35 randomly selected radiographs. Measurements were compared, and correlation coefficients (r2) were obtained. Cephalometric landmarks of the radiographs were digitized twice, area measurements were repeated three times by the same investigator, and the average values of three measurements were calculated to eliminate errors in measurements.
RESULTS
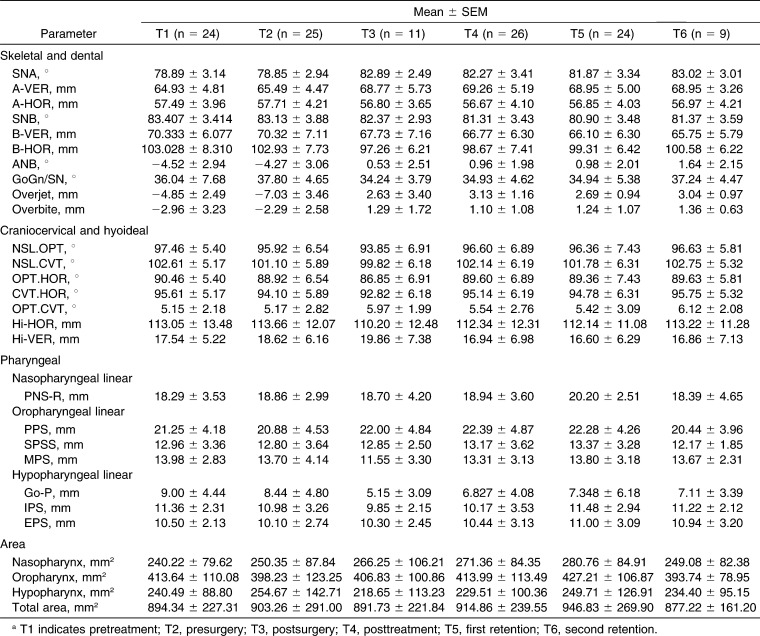
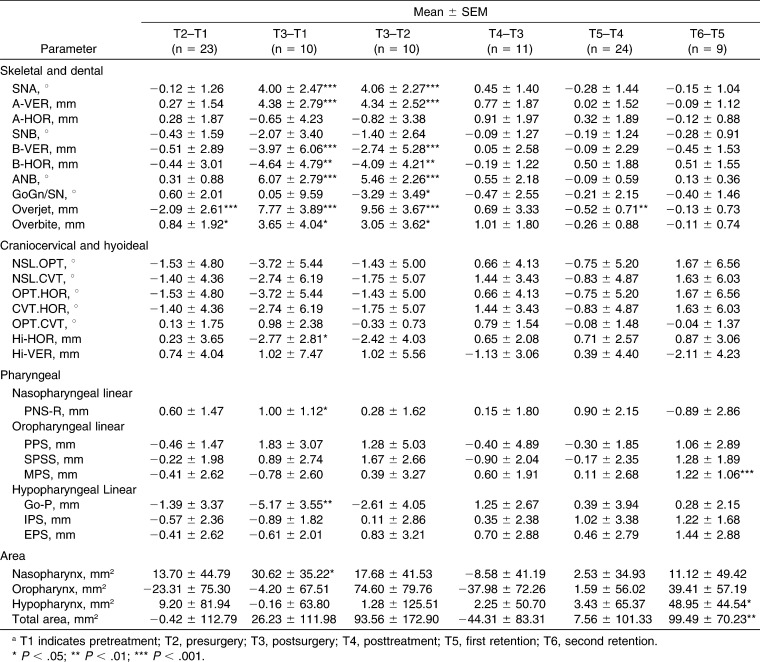
The reliability of the method was high, with the correlation coefficients ranging between .9910 and .9963. The mean values and standard error of the means of the variables at each time interval are presented in Table 3. The mean amount of maxillary advancement was 4.38 and mandibular set back was 3.97 mm. In Table 4, the statistical means of the differences and the standard error of the means of the parameters between time intervals are presented. No significant differences were identified in craniocervical angulation between time intervals. There was no significant relapse in skeletal parameters. Overjet significantly reduced between T5 and T4 time intervals (P < .01). There was a significant superior movement of hyoid bone at postsurgery (T3; P < .05); however, adaptation occurred to normal position in the long term. A significant increase was detected in the middle pharyngeal distance (MPS) parameter between the first and second retention radiographs (T5–T6; P < .001). A significant decrease was observed in Go-P between T3 and T1 (P < .01), and a significant increase in nasopharyngeal area was observed between T3 and T1 (P < .05). The hypopharyngeal area significantly increased between T5 and T6, and PNS-R significantly increased between T3 and T1 (P < .05).
Table 3.
Means and Standard Error of the Means of the Parameters According to Time Intervalsa
Table 4.
Statistical Means of the Differences and the Standard Error of the Means of the Parameters Between Time Intervalsa
DISCUSSION
Lateral cephalograms and computed tomography (CT) have been used to assess the pharyngeal airway space in patients after orthognathic surgery.13,19 According to Riley et al.,25 the pharyngeal airway space measured by cephalograms was highly correlated with measurements using a three-dimensional CT scan with considerably high accuracy in predictability.
A total of 26 subjects were used in the study. The missing pretreatment radiographs of the patients were compensated with presurgery radiographs, or vice versa. Also, some second retention radiographs were missing postsurgery, and those missing radiographs were considered in the statistical comparison. Therefore, the comparisons differ in terms of number of subjects between time intervals. Gender difference was not considered in our subjects. In the studies of Değerliyurt et al.26 and Kim et al.,27 no difference was observed between genders.
We used several retention records to make a more detailed evaluation of postsurgery outcome of the airway, hyoideal, and cervical posture parameters. Our postsurgery records were taken 5 months (short term), 1.4 years (T4), 3.2 years (T5), and 5.1 years (T6) after surgery. These retention records are the longest in the literature for pharyngeal airway evaluation in bimaxillary surgery patients. The mean amount of maxillary advancement was 4.38 with no impaction, and mandibular set back was 3.97 mm. No significant relapse was detected in skeletal variables between postsurgery treatment and retention records.
The increase of the nasopharyngeal dimension is in agreement with other studies.9,20,28,29 When the maxilla and mandible are protruded, widening occurs in the velopharyngeal airway with the elevation of the tissues attached to the maxilla, mandible, and hyoid bone.30 Nasopharynx area and PNS-R increase was significant at the short-term follow-up (T3–T1) and this increase is maintained although a slight decrease was observed at nasopharyngeal area T4–T3 stage. According to the CT study by Park et al.,22 a nonsignificant increase at the 5-month period and a nonsignificant decrease to presurgery values at 1.4 years postsurgery was observed in the nasopharynx. Greco et al.28 found a long-term increase in nasopharyngeal level after isolated maxillary advancement surgery, and similarly, Aydemir et al.9 and Jacobsone et al.21 found a significant increase in nasopharyngeal level in bimaxillary surgery patients after 1 year and 3 years postsurgery, respectively.
Bimaxillary operations reduce the negative effect of mandibular set back on the oropharynx with the advancement of the maxilla.7,8 No significant change was observed in oropharyngeal area in our study, which is in agreement with other studies.8,9 According to Park et al.,22 a significant decrease occurs at the oropharyngeal area and does not recover after surgery. This result can be due to the greater amount of set back in that study, as there is a correlation between the jaw movements and a change in airway measurements.31
According to Becker et al.,31 the nasopharynx, upper oropharynx, and middle oropharynx increase whereas the lower oropharynx decreases after bimaxillary surgery. Similarly, in our study, palatal pharyngeal distance and superior posterior pharyngeal distance tended to increase while MPS tended to decrease postsurgery. A significant increase between 3 and 5 years (P < .001) was observed at the MPS level; thus, we can evaluate this as an adaptation that occurred at the lower oropharynx.
In a CT study by Park et al.,22 a nonsignificant decrease was observed in the hypopharynx at the short follow-up period but recovered in the long term. We also did not find any significant change in the hypopharynx area, which is also in accordance with other studies.8,9 However, a significant increase occurred at 3 to 5 years of follow-up; thus, the total airway increased significantly in 3–5 years of follow-up (P < .01). In our study, from the period T5 to T6, a significant increase was observed in the oropharyngeal MPS parameter, hypopharyngeal parameter, and total area parameter, although there was no skeletal relapse in parameters at that period.
In our study, hyoid bone moved superior after 5 months postsurgery but returned to its original position in the long term. This is in accordance with the study by Marşan et al.32 According to our results, the pharyngeal airway continues to adapt to the new skeletal and soft tissue environment until the 5-year follow-up. Especially from 3 to 5 years postsurgery, a significant increase occurred in the hypopharynx, MPS, and total pharyngeal area. Bimaxillary surgery did not have an adverse effect on pharyngeal airway and, on the contrary, tends to enlarge the pharyngeal airway at long-term follow-up.
After surgery, with the help of the biomechanical positional change at the supra and infra hyoid muscles, reflexive adaptation at the pharyngeal area occurs. Occlusion and neuromuscular factors play an important role in the stomathognathic system's balance and adaptation. There is a limitation in our study with regard to the number of records at the time points. Thus, further investigation with larger databases is needed for long-term pharyngeal evaluation after orthognathic surgery.
CONCLUSIONS
Stabile widening occurs at the nasopharyngeal area after bimaxillary surgical operations.
The areas affected adversely after surgery recover at long-term follow-up.
The hyoid bone moves superior in the short term but comes to the original position at the long term.
No significant change occurs in craniocervical posture.
REFERENCES
- 1.Hochban W, Schurmann R, Bradenburg U, Conradt R. Mandibular setback for the surgical correction of mandibular hyperplasia—does it provoke sleep-related breathing disorders. Int J Oral Maxillofac Surg. 1996;25:333–338. doi: 10.1016/s0901-5027(06)80024-x. [DOI] [PubMed] [Google Scholar]
- 2.Güven O, Saraçoğlu U. Changes in pharyngeal airway space and hyoid bone positions after body ostectomies and sagittal split ramus osteotomies. J Craniofac Surg. 2005;16:23–30. doi: 10.1097/00001665-200501000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Hwang S, Chung CJ, Choi YJ, Huh JK, Kim KH. Changes of hyoid, tongue and pharyngeal airway after mandibular set back surgery by intraoral vertical ramus osteotomy. Angle Orthod. 2010;80:302–308. doi: 10.2319/040209-188.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Enacar A, Aksoy AU, Sençift Y, Haydar B, Aras K. Changes in hypopharyngeal airway space and in tongue and hyoid bone positions following the surgical correction of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1994;9:285–290. [PubMed] [Google Scholar]
- 5.Achilleos S, Krogstad O, Lyberg T. Surgical mandible setback and changes in uvuloglossopharyngeal morphology and head posture: a short- and long-term cephalometric study in males. Eur J Orthod. 2000;22:383–394. doi: 10.1093/ejo/22.4.383. [DOI] [PubMed] [Google Scholar]
- 6.Kawamata A, Fujishita M. Three-dimensional computed tomographic evaluation of morphologic airway changes after mandibular set back osteotomy for prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:278–287. doi: 10.1016/s1079-2104(00)70089-8. [DOI] [PubMed] [Google Scholar]
- 7.Chen F, Terada K, Hua Y, Saito I. Effects of bimaxillary surgery and mandibular set back surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. Am J Orthod Dentofacial Orthop. 2007;131:372–377. doi: 10.1016/j.ajodo.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 8.Değerliyurt K, Koichiro U, Hashiba Y, Marukawa K, Nakagawa K, Yamamato E. A comparative CT evaluation of pharyngeal airway changes in class III patients receiving bimaxillary surgery or mandibular set back surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:495–502. doi: 10.1016/j.tripleo.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Aydemir H, Memikoğlu U, Karasu H. Pharyngeal airway space, hyoid bone position and head posture after orthognathic surgery in Class III patients. Angle Orthod. 2012;82:993–1000. doi: 10.2319/091911-597.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wickwire NA, White RP, Jr, Proffit WR. The effect of mandibular osteotomy on tongue position. J Oral Surg. 1972;30:184–190. [PubMed] [Google Scholar]
- 11.Athanasiou AE, Toutoutzakis N, Mavreas D, Ritzaus M, Wenzel A. Alterations of hyoid bone position and pharyngeal depth and their relationship after surgical correction of mandibular prognathism. Am J Orthod Dentofac Orthop. 1991;100:259–265. doi: 10.1016/0889-5406(91)70063-3. [DOI] [PubMed] [Google Scholar]
- 12.Fromm B, Lundberg M. Postural behaviour of the hyoid bone in normal occlusion and before and after surgical correction of mandibular protrusion. Sven Tandlak Tidskr. 1970;63:425–433. [PubMed] [Google Scholar]
- 13.Wenzel A, Williams S, Ritzau M. Changes in head posture and nasopharyngeal airway following surgical correction of mandibular prognathism. Eur J Orthod. 1989;11:37–42. doi: 10.1093/oxfordjournals.ejo.a035962. [DOI] [PubMed] [Google Scholar]
- 14.Muto T, Yamazaki A, Takeda S. Relationship between the pharyngeal airway space and craniofacial morphology, taking into account head posture. Int J Oral Maxillofac Surg. 2006;36:132–136. doi: 10.1016/j.ijom.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 15.Eggensperger N, Smolka W, Ilzuka T. Long-term changes of hyoid bone position and pharyngeal airway size following mandibular setback by sagittal split ramus osteotomy. J Craniomaxillofac Surg. 2005;33:111–117. doi: 10.1016/j.jcms.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Wickwire NA, White RP, Jr, Proffit WR. The effect of mandibular osteotomy on tongue position. J Oral Surg. 1972;30:184–190. [PubMed] [Google Scholar]
- 17.Lew K. Changes in tongue and hyoid bone positions following anterior mandibular subapical osteotomy in patients with Class III malocclusion. Int J Adult Orthodon Orthognath Surg. 1993;8:123–128. [PubMed] [Google Scholar]
- 18.Tselnik M, Pogrel AM. Assessment of the pharyngeal airway space after mandibular set back surgery. J Oral Maxillofac Surg. 2000;58:282–285. doi: 10.1016/s0278-2391(00)90053-3. [DOI] [PubMed] [Google Scholar]
- 19.Kawakami M, Yamamoto K, Fujimoto M, Ohgi K, Inoue M, Kirita T. Changes in tongue and hyoid positions, and posterior airway space following mandibular set back surgery. J Craniomaxillofac Surg. 2005;33:107–110. doi: 10.1016/j.jcms.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Samman N, Tang SS, Xia J. Cephalometric study of the upper airway in surgically corrected Class III deformity. Int J Adult Orthodon Orthognath Surg. 2002;17:180–190. [PubMed] [Google Scholar]
- 21.Jacobsone G, Stanvik A, Espeland L. The effect of maxillary advancement and impaction on the upper airway after bimaxillary surgery to correct Class III malocclusion. Am J Orthod Dentofac Orthop. 2011;139:369–376. doi: 10.1016/j.ajodo.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 22.Park SB, Kim YI, Son WS, Hwang DS, Cho BH. Cone-beam computed tomography evaluation of short- and long-term airway change and stability after orthognathic surgery in patients with Class III skeletal deformities: bimaxillary surgery and mandibular set back surgery. Int J Oral Maxillofac Surg. 2012;41:87–93. doi: 10.1016/j.ijom.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 23.Ono T, Lowe AA, Ferguson KA, Fleetham JA. Associations among upper airway structure, body position and obesity in skeletal Class I male patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1996;109:625–634. doi: 10.1016/s0889-5406(96)70074-4. [DOI] [PubMed] [Google Scholar]
- 24.Tsuiki S, Hiyama S, Ono T, Immura N, Ishiwata N, Kuroda T. Effect of a titratable oral appliance on supine airway size in awake non-apneic individuals. Sleep. 2001;24:554–560. doi: 10.1093/sleep/24.5.554. [DOI] [PubMed] [Google Scholar]
- 25.Riley RW, Powell NB, Guilleminault C. Maxillary, mandibular and hyoid advancement for treatment of obstructive sleep apnea: a review of 40 patients. J Oral Maxillofac Surg. 1990;48:20–26. doi: 10.1016/0278-2391(90)90174-z. [DOI] [PubMed] [Google Scholar]
- 26.Değerliyurt K, Ueki K, Hashiba Y, et al. The effect of mandibular setback or two-jaws surgery on pharyngeal airway among different genders. Int J Oral Maxillofac Surg. 2009;38:647–652. doi: 10.1016/j.ijom.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 27.Kim JS, Kim JK, Hong SC, Cho JH. Pharyngeal airway changes after sagittal split ramus osteotomy of the mandible: a comparison between genders. J Oral Maxillofac Surg. 2010;68:1802–1806. doi: 10.1016/j.joms.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 28.Greco JM, Frohberg U, Van Sickels JE. Cephalometric analysis of long-term airway space changes with maxillary osteotomies. Oral Surg Oral Med Oral Pathol. 1990;70:552–554. doi: 10.1016/0030-4220(90)90394-8. [DOI] [PubMed] [Google Scholar]
- 29.Pereira-Filho VA, Castro-Silva LM, Moraes M. Cephalometric evaluation of pharyngeal airway space changes in class III patients undergoing orthognathic surgery. J Oral Maxillofac Surg. 2011;69:409–415. doi: 10.1016/j.joms.2011.02.132. [DOI] [PubMed] [Google Scholar]
- 30.Riley RW, Nelson B, Powell NB, Guilleminault C. Obstructive sleep apnea syndrome: a surgical protocol for dynamic upper airway reconstruction. J Oral Maxillofac Surg. 1993;51:742–747. doi: 10.1016/s0278-2391(10)80412-4. [DOI] [PubMed] [Google Scholar]
- 31.Becker OE, Avelar RL, Göelzer JG, Dolzan Ado N, Haas OL, Jr, De Oliveira RB. Pharyngeal airway changes in Class III patients treated with double jaw orthognathic surgery—maxillary advancement and mandibular setback. J Oral Maxillofac Surg. 2012;70:639–647. doi: 10.1016/j.joms.2012.07.052. [DOI] [PubMed] [Google Scholar]
- 32.Marşan G, Kuvat SV, Öztaş E, Cura N, Süzal Z, Emekli U. Oropharyngeal airway changes following bimaxillary surgery in Class III female adults. J Craniomaxillofac Surg. 2008;37:69–73. doi: 10.1016/j.jcms.2008.11.001. [DOI] [PubMed] [Google Scholar]